Abstract
Peripheral Cardiovascular disease is an epidemic that can lead to death or amputation of limbs. The disease is evident as inadequate tissue intromission instigated by pre-existing atherosclerosis severely exacerbated by either emboli or thrombi. Several individuals suffer from significant extents of Peripheral Cardiovascular ailments. However, in cases of critical limb ischemia, this dormant ailment can suddenly be diagnosed as fatal, requiring emergency medical intervention to reduce mortality. Early recognition and taking early measures are critical in improving the consequences of the disease. This paper will highlight the disease’s symptoms and the treatment alternatives. Peripheral cardiovascular disease is associated with several risk factors, such as smoking, diabetes, previous coronary artery disease, and an inactive lifestyle. Finally, the article outlines the healthcare team’s significance in treating patients with the disease and available alternative interventions.
Introduction
Peripheral cardiovascular disease is an incurable gradual atherosclerotic ailment that causes partial or entire peripheral cardiovascular occlusion. The disease typically impacts the gastric aorta, iliac arteries, lower limbs, and in rare cases, the upper body. Around the globe it has impacted roughly 200 million individuals worldwide, therefore gaining global awareness because of its lengthened exposure risk factor. Patients suffering from the disease have irregular symptoms, some being asymptomatic while others are advancing to the arteries’ ulceration, amputation, intermittent claudication, and resting limb ischemia. Peripheral cardiovascular disease is an equivalent of cardiovascular ailments with related either high risk lethal, or treatable cardiovascular episodes regular occurrence like myocardial infarction or stroke. This illness is continuously developing, devitalizing pervasive, and demands urgent healthcare concerns for treating patients.
Discussion
Reasons for choosing this particular disease
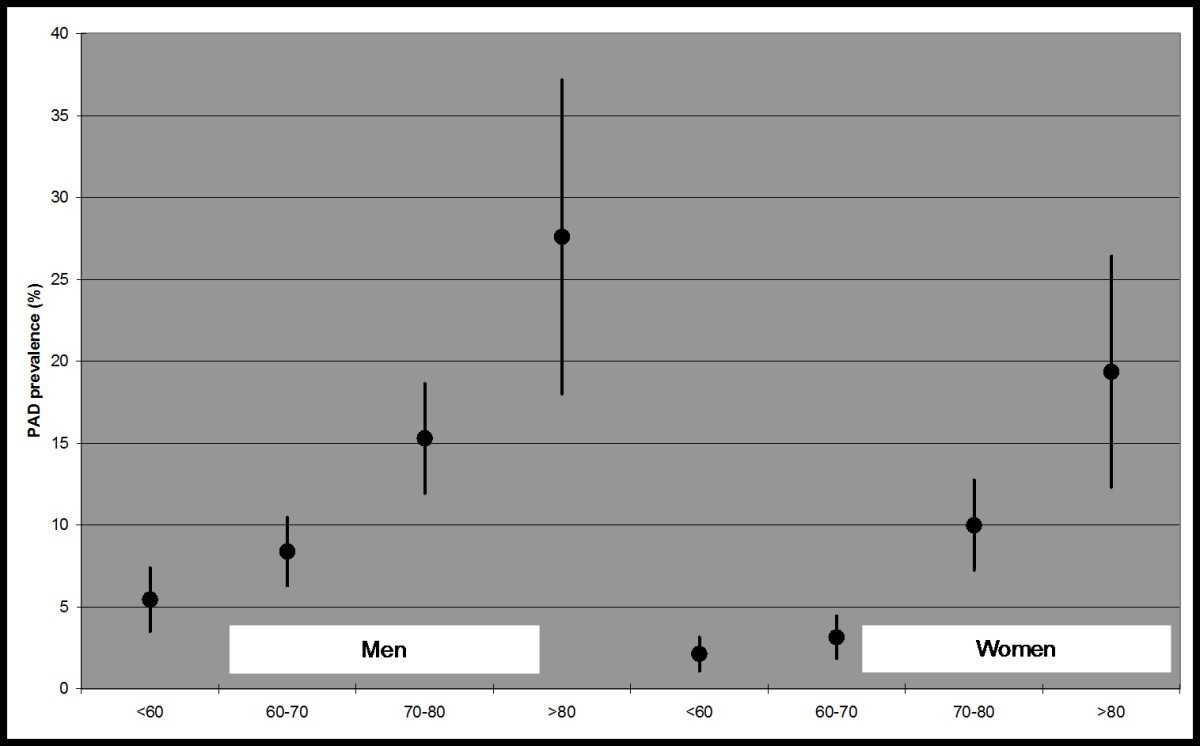
The reasons for choosing to delve into this disease are extensive, but firstly it is essential to understand that peripheral cardiovascular disease requires to be scrutinized since it affects between 8 to 10 million people in America; therefore, there is much worry to be concerned with the ailment (Figure 1). Despite the disease not being lethal, the other underlying effects are fatal since patients are more likely to have blockages in other body parts leading to more detrimental issues. Atherosclerosis, in particular, leads to the clogging of arteries with plaque deposits that restrain the flow of blood in other different body parts. Atherosclerosis generally elucidates why patients with peripheral cardiovascular disease are way more likely to get a stroke or a heart attack.
Early detection of peripheral cardiovascular disease is essential in addressing the disease and preventing heart attack, kidney malfunction, or stroke since the underlying cause is addressed early on. Moreover, prevention of such lethal effects of the disease is recommended by medical practitioners since little can be done about the prevalent risk factors, such as the history of occurrence in the family, racial risk, or age. However, one can change some lifestyle actions that drastically reduce the risk. Doctors advocate quitting smoking to lower the risk of complications and progression of the ailment (Kannel 61-68). Moreover, everybody must keep their blood pressure, cholesterol, and blood glucose at safe levels by consuming a healthy, balanced diet low in fat and cholesterol. Latent individuals should get more active by engaging in at least half an hour of daily activity to maintain a healthy body weight of a BMI below 24.9.
The signs and symptoms of Peripheral Cardiovascular Disease:
- Cellular level
Roughly half of the diagnosed individuals with Peripheral cardiovascular disease do not exhibit any symptoms. Those displaying symptoms commonly exhibit leg cramping (intermittent claudication) that is extremely painful and occurs during exercise. The pain relieves when resting since the muscle requires less blood flow, hence the pain’s disappearance. The pain may be experienced on both or a single leg, contingent on the area of the clogged blood vessel.
- Tissue level
Peripheral cardiovascular symptoms are usually baffling since people confuse the symptoms with typical aging-related pains or other illnesses like arthritis or nerve damage. Claudication is the most lenient symptom and involves muscle cramps, especially in the calves intensifying during exercise and diminishing during rest due to muscle tissues failing to cater to the heightened oxygen demand during the activity. Patients often experience trouble moving as fast as before, while those with the most severe form of the disease go through severe pain and get sores that do not heal. These sores and wounds might lead to amputation when not hastily treated.
- Organismal level
Most cases of the peripheral cardiovascular disease do not portray symptoms till later when the ailment has progressively advanced. The symptoms include vascular ulcers that do not heal, gangrene implying darkened locations on the skin or loss of skin, and in other cases, blue or dark purple shade to the skin. Muscular numbness occasioned by constant pain that feels like getting prickled by needles is prevalent, leading to muscular weakness. The most common symptom is intermittent claudication, which feels like cramps in the legs getting worse when exercising, and pain relief when the individual goes to rest.
Treatment/ cure
Diagnosed patients with peripheral cardiovascular disease need an accurate perspective to consider age, risk factors, the severity of the disease progression, and functionality. Treatment of the disease is categorized into two extensive divisions intended to lower cardiovascular risks and alleviate symptoms. Patients have a higher risk of coronary artery ailment fatality, cardiovascular-related deaths, and general mortality. Therefore, treatment commences with lifestyle alteration to halt the progression of the disease with the assistance of medical and intervention treatment needed to control symptoms and lower the risk of cardiovascular events. (Olin 678-92)
Cardiovascular Risk Factor Modification
Modification of the most threatening risk factors is vital for reducing cardiovascular risk. Firstly, ceasing smoking with immediate effect lowers the risk of progression, myocardial infarction, Acute arterial occlusion, and stroke. Reduction of smoking to mitigate cardiovascular consequences can be achieved through patient education and behavioral and clinical therapy. Routine use of statin therapy effectively reduces cardiovascular risks leading to mortality, and lowers the requirement for revascularization. Improved outcomes have been achieved through hypertension management by lowering the blood pressure to below 130/80 in individuals with diabetes and 140/90 in others since diabetes is a risk factor.
Exercise Therapy
Previous studies have displayed that superintended exercise therapy schemes have improved claudication symptoms. A practical outlook for treating patients with claudication is displayed in (Table 1). Exercise tremendously alleviated pain during walking by approximately 400 feet, according to a series of 27 studies (Gardner 975-980). The exercise therapy programs ideally comprised 30-45 minutes long sessions every 4-5 times weekly (Momsen 463-474)
Pharmacotherapy
Patients who do not show improvement signs from exercise programs and risk factor modification can be subjected to pharmacological therapy targeting intermittent claudication treatment. Cilostazol and naftidrofuryl medications are best fit for intermittent claudication. Cilostazol obstructs phosphodiesterase-3 and has shown platelet aggregation inhibition and vasodilatory properties impeding smooth muscle cell spread, leading to remarkably longer walking distances without pain. Naftidrofuryl is a 5-hydroxytryptamine-2- sensory receptor adversary that impedes glucose uptake and escalates adenosine triphosphate levels. Compared to cilostazol, It has fewer side effects and is highly recommended in the situation where it is available. (Thompson 1314-1319)
Revascularization
In the unlikely situation that the patient has enervative symptoms that are unresponsive to the previous treatment interventions, endovascular or surgical treatment might have to be introduced. Patients with debilitated claudication affecting routine chores indicate urgency for this intervention to rescue limbs from amputations demonstrated by ulceration, gangrene, and ischemic pain while not walking. The surgical decision is determined by several factors the patient’s mobility, risk of surgery, anatomy, the progression of the disease, and the doctor’s skills.
Conclusion/recommendations
The peripheral cardiovascular disease progresses systematically to cause undesired long-term consequences. Despite claudication symptoms staying unnoticeable for an extensive period, patients are subjected to the risk of fatality in the occurrence of cardiovascular events. Professional intervention is required to pin down patients at risk, impeding the secondary progression and providing patients with multiple options for treatment. Healthcare providers must educate patients on risk factors such as smoking, hypertension, high cholesterol levels, and diabetes. Considering that over three-quarters of the patients who die pass on due to cardiovascular events, a cardiologist should be engaged to offer patients multiple survival options. Cardiovascular medical experts are essential for patient education on future drug side effects and interactions and updates on the progression of the patient’s disease.
References
Gardner, A. W., & Poehlman, E. T. (1995). Exercise intervention programs for the treatment of claudication pain: a meta-analysis. Jama, 274(12), 975-980.
Kannel, W. B. (1973). The Framingham Study: cigarettes and the development of intermittent claudication. Geriatrics, 28, 61-68.
Momsen, A. H., et al. “Drug therapy for improving walking distance in intermittent claudication: a systematic review and meta-analysis of robust randomized controlled studies.” European Journal of Vascular and Endovascular Surgery 38.4 (2009): 463–474.
Olin, Jeffrey W, and Brett A Sea love. “Peripheral artery disease: current insight into the disease and its diagnosis and management.” Mayo Clinic proceedings vol. 85,7 (2010): 678–92. doi:10.4065/mcp.2010.0133
Thompson PD, Zimet R, Forbes WP, Zhang P. Meta-analysis of results from eight randomized, placebo-controlled trials on the effect of cilostazol on patients with intermittent claudication. Am J Cardiol. 2002;90(12):1314-1319
Tables and Figures
Table 1: Approach to the treatment of claudication.
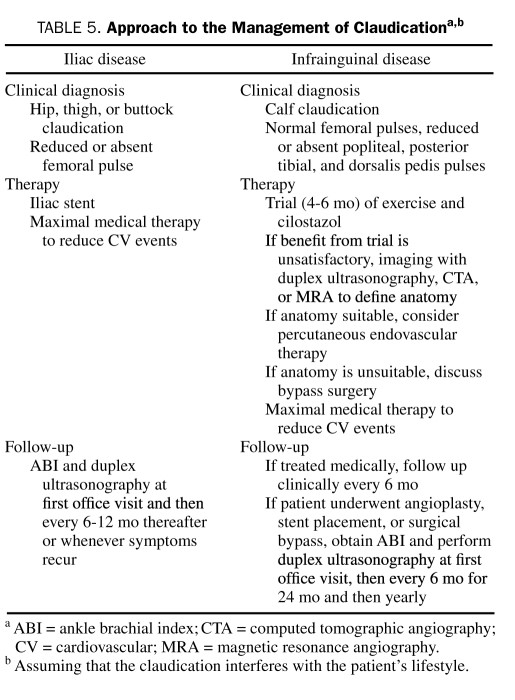
Figure 1: Prevalence of peripheral cardiovascular disease by age and gender.
 write
write