The Joint Commission. (2021). Speak Up for New Parents | The Joint Commission. Www.jointcommission.org. https://www.jointcommission.org/resources/for-consumers/speak-up-campaigns/for-new-parents/
The Joint Commission (2021) Speak Up for New Parents is a brochure helping new parents to make better decisions about their care. As having a child is a life-changing situation, it is significant that mothers be alert to clinical symptoms of hypertension and preeclampsia, hemorrhage, infections, and depression to seek appropriate medical help and care.
Summary of the Brochure
Hypertensive complications during pregnancy include gestational hypertension and preeclampsia, which may occur before, during, and after childbirth. Gestational hypertension in women is indicated by a systolic pressure of > 140 mmHg and a diastolic pressure of > 90mmHg or higher. In most cases, hypertension in these women occurs during the first 20 weeks of pregnancy, even in cases where the mother was not hypertensive before the pregnancy. Nevertheless, most mothers with gestational hypertension experience only a slight increase in blood pressure, while others develop severe hypertension, predisposing them to develop hypertension in the future (American College of Obstetricians and Gynecologists, 2021b).
Preeclampsia develops during 20 weeks of pregnancy and weeks after childbirth, and when it arises before the, it is termed early-onset preeclampsia. When this complication is undertreated, it leads to Hemolysis, Elevated Liver enzymes, and Low Platelet count (HELLP) syndrome that affects blood clotting and damages the red blood cells. Preeclampsia causes abdominal pain, chest, and bleeding in the liver. Women diagnosed with preeclampsia and whose babies were born preterm have pronounced risks of developing hypertension, stroke, and heart disease. In addition, experiencing preeclampsia once predisposes women to develop it again during future pregnancies (American College of Obstetricians and Gynecologists, 2021b). Therefore, women should pay attention to how they feel during and after pregnancy and contact an obstetrician when they experience symptoms, including swelling, shortness of breath, abrupt weight gain of above three or five pounds, nausea or vomiting, headaches, vision changes such as blurry vision, pain in the lower back, and in the upper right side of the stomach area which is not related to contractions.
Women are also at risk of experiencing obstetric hemorrhage, severe bleeding occurring before or after delivery. While uterine atony significantly leads to obstetric hemorrhage development, other factors, including incisions, lacerations, and homeostasis disorders, can also lead to this condition. Postpartum hemorrhage is commonly associated with a blood loss of >50ml. However, a blood loss of 100ml is tolerated in women without underlying medical conditions such as anemia (Mclintock & James, 2011). Due to the clinical impact of blood loss, it is crucial to consider that such an amount of blood loss has significant adverse effects in women with anemia. Early call for help is substantial in managing hemorrhage. Therefore, women should contact an obstetrician when they experience signs, including shortness of breath, weakness, feeling thirsty, increased heart rate, dizziness after arising from a chair or bed, rapid soaking of pads, development of large-quarter-sized blood clots, feeling cool and clammy, and lack of urination.
New mothers are also at pronounced risk of developing infections after giving birth. Postpartum infections are due to physiologic and iatrogenic trauma to the abdominal and reproductive, urinary tracts, and genitals during childbirth, allowing bacteria into these sterile environments. Postpartum infections are mainly more common in women who underwent cesarean section than those who underwent vaginal delivery. Risks in postpartum infections are pronounced in women with high BMI, diabetes hypertension, sexually transmitted infections, immune compromise, and group-B streptococcus positive status. Birth events attributed to increased infections risks include operative vaginal delivery, manual removal of the placenta, thick meconium staining, post-term labor, multiple internal exams, internal fetal or uterine monitoring, use of foley catheter, retained products of conception, and postpartum hemorrhage (Boushra & Rahman, 2020). Postpartum infections are highly fatal, and new mothers should contact an obstetrician when they observe signs, including rapid heart rates, foul-smelling discharge, paleness, fatigue, headaches, muscle aches, warm-painful redness near the surgical incision site, lower abdominal pain, low-grade fever, and chills.
New mothers also experience baby blues from 2-3 days after childbirth, where they begin to feel depressed, upset, and anxious. In addition, they may feel angry towards their child and partners, cry for no reason, experience trouble sleeping, making choices, eating, and question whether they can handle caring responsibilities (American College of Obstetricians and Gynecologists, 2018). However, baby blues may disappear between 1-2 weeks without any treatment intervention. On the other hand, new mothers are at risk of developing postpartum depression in which they experience anxiety, sadness, and despair, preventing them from completing their tasks typically. Postpartum depression arises after a year after delivery but, in common cases, occurs about 1-3 weeks after childbirth. Postpartum depression has detrimental effects on the parent’s health and the infant’s developmental outcomes. It negatively impacts the mother’s ability to nurture the child. In addition, depression reduces bonding chances between the mother and the child. This, in turn, negatively affects breastfeeding leading to cases of malnutrition and reduced infant growth rates. Poor bonding also leads to emotional, cognitive, and social development problems (Abadiga, 2019). The development of this complication is influenced by various aspects, including changes in hormone levels, fatigue, lifestyle, emotional factors, and depression history. Due to the possible side-effects of antidepressants medication, it is crucial to identify postpartum depression timely. New mothers should consult an obstetrician when they experience eating and sleeping difficulties, helplessness or sadness, thoughts of harming themselves and the baby, avoiding contact or bonding with the baby and slacking in getting out of bed.
Patient Communication
It is not always easy for pregnant and nursing mothers to find the exact words to talk about what they are experiencing since most of them assume their feelings result from pregnancy, hence confusing major disease symptoms with morning sickness symptoms. In addition, this population also raises many questions, including (am I supposed to feel this way?) which are sometimes hard to answer. The above brochure for pregnant and new mothers provides this group with information and tips that alert them if they need medical attention. The brochure presents symptoms that women might experience, and hence they find it easier to communicate them with their health care provider. In addition, it also helps mothers understand the terms used by the doctor, therefore, communication between the health care provider and the patient is improved. Efficient communication between the provider and the patient enhances the quick resolution of the problems identified or challenges encountered by the patient, enhances patients to decide on the care process, and enhances renewed confidence and motivation towards the provider, providing better clinical outcomes.
Personal Reflection
The reason for choosing this brochure is its relevancy in a crucial topic in modern medicine and society. In addition, the brochure has presented the information in a clear way in which mothers can understand. The topic was of interest as many women experience health problems during pregnancy, and in most cases, the complications endanger the mother and the fetus’s health. Notably, even women who were healthy before pregnancy are at risk of developing these complications. Therefore, I chose this topic to increase and sensitize knowledge on the benefits of regular parental checkups, enhancing clinicians to timely diagnose, treat, and manage these complications before they progress, thus mitigating potential risks. In addition, such a topic is useful in the current health care system as mothers need to understand symptoms of some common pregnancy complications to differentiate them from normal pregnancy feelings and symptoms such as morning sickness.
Evaluation of the brochure
The brochure provided information that could be used in patient education. Although obstetricians usually provide prenatal and postnatal care, it necessitates women to be conversant with the most common postnatal and prenatal complication symptoms to know when and under what circumstances they should visit the obstetrician. As many women face increased risks of developing complications due to their current conditions, incorporating such symptoms of common, occurring complications is necessary to educate patients on how to identify symptoms of these common complications and give them tips on managing and preventing the occurrence of such complications. This will reduce disease burdens in women and other adverse health effects to the mother and the infants as they can access timely management interventions of such complications when they are detected early. The information was presented clearly in a well-designed brochure, and it directly pinpointed the symptoms that women should look out for under various complications associated with pregnancy. Current literature supports information in the brochure, such as Neiger (2017), who suggests that most pregnancy-related complications often disappear shortly after childbirth, including hypertension and preeclampsia. However, mothers who developed these complications are at risk of developing them in future pregnancies.
Similarly, Schrey-Petersen et al. (2021) report that nearly half of maternal deaths occur after birth. The authors suggest that postpartum complications, including infections, hypertension, hemorrhage, and depression, are often life-threatening and demand timely diagnosis and urgent treatment intervention from medical professionals. This brochure will be significantly beneficial for pregnant women and nursing mothers. But can also be used by women planning for a pregnancy. This information increases patient safety as mothers become familiar with the clinical symptoms of pregnancy-related conditions and can seek medical attention at an early stage.
Conclusion
Finally, the brochure on Speak Up for New Parents has conclusively provided signs of various complications related to pregnancy, including hypertension, preeclampsia, hemorrhage, infections, and depression. The brochure emphasizes the need for mothers to be familiar with these symptoms to get early medical interventions. In addition, if left untreated, such complications are accompanied by adverse health effects to the mother and the child. For instance, mother-child-related depression affects their bonding that negatively influences the child’s cognitive, emotional, and social development. While most pregnancy-related complications disappear after delivery, mothers who develop these complications are at risk of developing them later in future pregnancies.
Similarly, women who were healthy before getting pregnant are also at pronounced risks of developing these complications. Evident research shows that most of these complications are associated with increased long-term maternal morbidity. Therefore, patient education on the various clinical manifestations of pregnancy-related complications is crucial for women to identify the symptoms of multiple complications to seek timely medical attention and reduce the associated risks.
Figure 1: Speak Up For New Parents
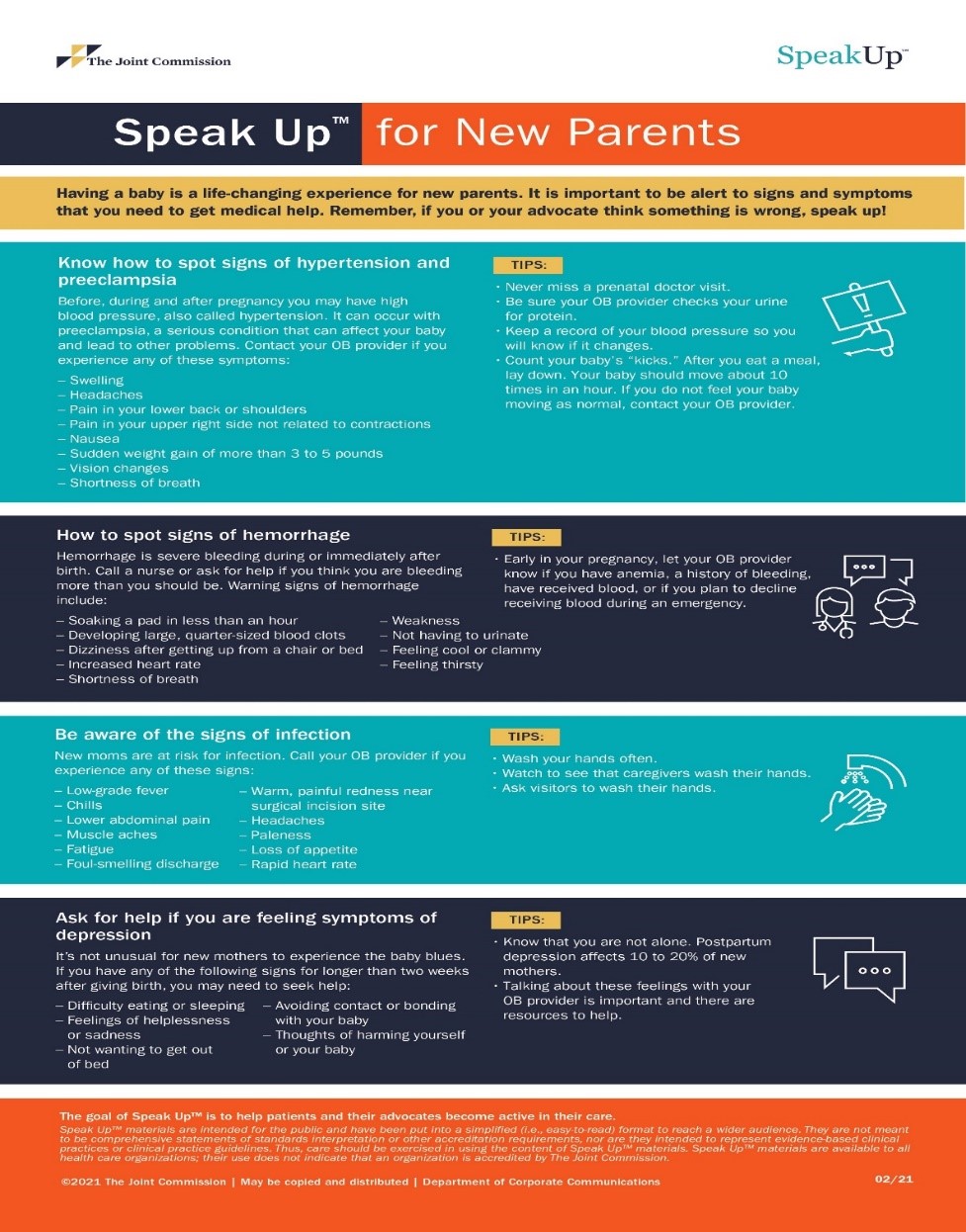
Notes: From The Joint Commission (Infographic) The Joint Commission, 2021
( https://www.jointcommission.org/resources/for-consumers/speak-up-campaigns/for-new-parents/)
References
Abadiga, M. (2019). Magnitude and associated factors of postpartum depression among women in Nekemte town, East Wollega zone, west Ethiopia, 2019: A community-based study. PLOS ONE, 14(11), e0224792. https://doi.org/10.1371/journal.pone.0224792
American College of Obstetricians and Gynecologists. (2018, November). Screening for Perinatal Depression. Www.acog.org. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2018/11/screening-for-perinatal-depression
American College of Obstetricians and Gynecologists. (2021a). Postpartum Depression. Www.acog.org. https://www.acog.org/womens-health/faqs/postpartum-depression
American College of Obstetricians and Gynecologists. (2021b). Preeclampsia and High Blood Pressure During Pregnancy. Www.acog.org. https://www.acog.org/womens-health/faqs/preeclampsia-and-high-blood-pressure-during-pregnancy?utm_source=redirect&utm_medium=web&utm_campaign=otn
Boushra, M., & Rahman, O. (2020). Postpartum Infection. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK560804/
Mclintock, C., & James, A. H. (2011). Obstetric hemorrhage. Journal of Thrombosis and Haemostasis, 9(8), 1441–1451. https://doi.org/10.1111/j.1538-7836.2011.04398.x
Neiger, R. (2017). Long-Term Effects of Pregnancy Complications on Maternal Health: A Review. Journal of Clinical Medicine, 6(8), 76. https://doi.org/10.3390/jcm6080076
Schrey-Petersen, S., Tauscher, A., Dathan-Stumpf, A., & Stepan, H. (2021). Diseases and Complications of the Puerperium. Deutsches Ärzteblatt International, 118(25), 436–446. https://doi.org/10.3238/arztebl.m2021.0168
The Joint Commission. (2021). Speak Up For New Parents | The Joint Commission. Www.jointcommission.org. https://www.jointcommission.org/resources/for-consumers/speak-up-campaigns/for-new-parents/
 write
write