Chapter 1: Introduction
1.1 Introduction
The initial chapter talks about the importance of understanding key leadership roles in any hospital setting and how they affect patient safety. Adopting strategies that have been shown to work in healthcare results requires exceptional leadership. At the start, a research topic should be given to show how important it is to study leadership practices and how they are used in health. This provides us with a starting point for learning how leadership affects how practices are implemented, which in turn changes patient safety and care quality. This study will make it easier to see how the different aspects of healthcare leadership affect patient care (Harvey et al., 2020).
1.2 Background of the Research
The idea of study background shows how vital patient safety and quality are in healthcare organisations and how they must be dealt with. There have been improvements in knowledge and technology, but not everything is fair because there are a lot of medical mistakes that could have been avoided and even bad things that happen within this system. These things point to a systemic problem that needs to be fixed. Leadership is critical when it comes to shaping an organization’s culture or deciding which evidence-based methods to use to improve patient outcomes. To be able to find these methods, you need to understand the foundations on which leaders make decisions about changes that could lead to success. Many studies have already been done on different aspects of leadership in the healthcare industry. However, more must be learned about how evidence-based practices can be used at other sites where people provide healthcare for diverse populations. The researcher will look at the types of leadership that are needed to provide patient-centred care in the hopes that some light will have been shed on how to improve the performance of the healthcare system and, as a result, how this setup may have an effect on the outcome for patients (Kitson et al., 2021).
1.3 Rationale of the Research
The rationale of this research is that knowledge used in improving patient safety and delivery of care services depends on effective leadership. Although its particulars are recognized as crucial, there is almost nothing done well enough to close all the voids left in our knowledge of how leadership reflects on a career. This study aims to bridge these gaps by analyzing such targeted approaches and measures that leaders can improve both patients’ safety and quality of care. Health leaders, policymakers and practitioners will find the results of this study helpful in their work. However, it seeks to reveal a complex understanding of how leadership may affect healthcare delivery (Renolen et al., 2020).
1.4 Problem Statement
Although the importance of succeeding leadership in health care is acknowledged, as noted firstly, ignorance concerning evidence-based strategies for patient safety and exemplary treatment are outlined in this problem description. Problems will be encountered when trying to convert leadership thoughts into prevalent practices that maximize patient results, even with healthcare delivery reforms. This approach analyses techniques and strategies that managers might employ to raise patient safety standards and enhance the level of care in healthcare settings, attempting to address the previously described problem. The study intends to produce valuable results and feedback by elucidating this relationship, promoting the advancement of patient-centred care delivery and healthcare leadership (Sherwood and Barnsteiner, 2021).
1.5 Research Aim
The research aims to learn and illustrate the role of sufficient leadership in healthcare, primarily through introducing evidence-based practices that provide for increased patient safety and better quality of care.
1.6 Research Objectives
- To analyze the management impact of implementing proof-based practices in healthcare settings.
- Evaluate the techniques leaders can employ to enhance affected persons’ safety in the healthcare gadget.
- Understanding powerful management contributes to developing significant care for patients in healthcare centres.
1.7 Research Question
- How does management impact the implementation of proof-based practices in healthcare settings?
- What precise techniques can leaders employ to enhance affected persons’ safety in the healthcare gadget?
- How does powerful management contribute to developing significant patient care in healthcare centres?
1.8 Significance of the Research
This study is significant because it can bring about significant changes that will improve patient outcomes and healthcare delivery. As a result, this work assists healthcare organizations in understanding their responsibilities regarding patient safety and quality treatment by highlighting the significance of leadership in enforcing evidence-based procedures. To ensure the establishment of an atmosphere favourable to safety and excellence, the strategic leadership approach outlined in this research can assist in the design of decision-making processes and help create training programs for healthcare leaders. Additionally, the findings impact projects aimed at maximizing resource utilization and evidence-based care delivery through policy and practice implications. By bridging the gap between leadership theory and real-world implementation, this study advances patient-centred care and healthcare management, which benefits organizations, providers, and patients equally (Tucker et al., 2021).
1.9 Summary
In Chapter 1, it is clear that the subject of study herein refers to the importance and criticality aspect of having good leadership in every healthcare setting with an underlying notion i.e. patient safety as well as quality treatment which are guaranteed at all times without any hitches whatsoever. The purpose of the study is backgrounded and justified, which follows with a problem statement that focuses on a better understanding of leadership roles in the implementation of EBP.
Chapter 2: Literature Review
2.1 Introduction
This chapter talks about the research that has been done on leadership styles and how they affect both patient safety and the level of care given to patients in a healthcare setting. This part provides an overview of the main ideas and problems discussed in the literature. This sets the stage for a more in-depth discussion of several leadership styles tested to see how well they support evidence-based strategies that aim to improve patient outcomes. By compiling relevant literature, this gap analysis finds holes in the trends that have been seen and places that need more research. This helps explain leadership’s role in getting medical help to people who need it.
2.2 Management Impact on Implementing Evidence-Based Practices
One thing that helps evidence-based practices work well in healthcare is middle managers and nurse managers. They are the link between leadership and executive-level management, setting strategic directions and ensuring that the organization follows the rules meant to make things easier for frontline workers. The management impacts on application and EBPs have also been cut down. This includes both internal and external factors that help or hurt their acceptance.
In addition, Birken et al. (2018) did a thorough study of middle managers’ role in implementing EBP in a hospital setting. They said that middle managers are the ones who turn organizational strategies into deeds at the front lines. In the world of EBPs, middle managers are the ones who bring about change among healthcare workers. Through the lens of the author’s study, we can see how important it is for middle managers to understand leadership, communication skills, and organizational factors.
In 2023, Hosseini-Moghaddam et al. published a study in which nursing managers talked about what they thought made evidence-based practice easier or harder. Their results show that the organizational culture, the ease of access to resources, and the involvement of leaders are all critical for the introduction and execution steps to go smoothly. On the other hand, process notions equilibrium can also be provided by limits such as not having enough time to act within EBPs’ time frames and being overworked. Because of this, nurse managers should talk to different people about these problems and ask what can be done to solve them. One solution could be creating a culture where learning is valued, or another could offer teaching opportunities or specific training programmes for implementing EBP.
In their 2020 paper, Bond and Drake (2020) talked about the reliability of evidence-based practice evaluation, which supports methods of constant assessment. Their study shows how important it is to check and measure how well EBPs are being used since treatments must go as planned. In this case, managers’ significant jobs are to oversee the fidelity assessment processes and give feedback to frontline staff. They may also step in sometimes to help with problems related to putting standard quality standards into action.
Finally, using evidence-based methods in healthcare is complicated because of the way management works with these methods. By turning organizational goals into jobs that can be done, middle managers and nurse managers make it much easier to implement EBP more quickly. Evidence-based nursing processes are seen as valuable because of their work, advice, and assistance. This means that they must continue to be used in a way that makes progress. Using standardized testing methods also helps keep things honest and in line with tried-and-true best practices, which supports the usefulness of EBPs. Frontline staff are involved with organizational leadership because evidence-based delivery needs to be managed well for long-lasting changes in patient outcomes to happen.
2.3 Techniques for Enhancing Patient Safety
Many tactics and methods are used to try and lower the number of medical mistakes and other problems that can happen, like bad reactions to medications. One is making healthcare settings safer for patients and providing better care. Many ways were tried to make patients safer, focusing on building identification tools, teaching, and talking to each other.
Burgener (2020) focuses on how important good communication is for making patients happy and keeping them safe. Interdisciplinary teams need to speak clearly and avoid mistakes as much as possible so that the correct information gets across. Patients should also be able to communicate clearly with healthcare professionals. Interdisciplinary team meetings, standard communication standards, and organized handoffs are ways healthcare workers can improve their communication. These methods help create a safe environment.
al-Worafi (203) is all about making sure patients are safe. He goes to developing countries to find proof of how important research, education, and uses are. Case studies are the primary way he does this to make sure safety is taken care of. So, patient safety programmes that focus on patients, carers, and healthcare workers are vital for bringing attention to patient safety issues, ensuring best practices are used in all parts of healthcare, and giving stakeholders the power to create safer practice settings. Along with listing the strategies shown to improve patient safety, study and case reports often include specific real-life issues in practice, such as areas of clinical care that they assume are standard.
In their 2020 study, Guzman-Piera, Piera Jiménez, et al. look at different ways to identify patients and how that affects safety. Patients who are accurately identified get care tailored to them and no one else. This lowers the risk of medication mistakes, surgical emergencies, and other nasty things happening. Many things are used to make identifying patients easier and more accurate. These include biometric recognition, barcode reading, electronic health record systems, and more. Because of this, it is essential to understand the pros, cons, and risks of using different modes of identification to incorporate them into patient safety processes successfully.
To improve patient safety, we need a complete plan that eliminates the things that get in the way of communication, promotes learning and study, and uses good ways to find patients. Medical organizations can make care environments safer for their patients with lower risks to their well-being by developing a way to improve communication, setting aside money for research and teaching programmes, and putting in place reliable ID systems. However, making patient safety processes work well and improving outcomes across healthcare systems will only be possible if everyone works together, including leaders, patients, lawmakers, researchers, and others.
2.4 Understanding the Role of Effective Management in Patient Care
Proper patient care management is needed to ensure that high-quality healthcare services are provided well and positively affect both outcomes. Numerous articles have shown several facets of efficient healthcare management predicated on health literacy, communication, and culture.
Research on job-hopping among millennial workers in the US food and agriculture industry was conducted by Tetteh et al. (2021). This research highlights the importance of comprehending employees’ perspectives and intentions in an organizational environment, even though it is not directly applicable to the healthcare industry. Therefore, identifying and resolving problems that impact job satisfaction, employee engagement, and retention constitutes proper management. In the healthcare industry, this results in favourable working conditions that offer advancement opportunities and foster a collaborative culture among healthcare professionals.
Buttini et al.‘s (2021) report examined dry powder capsules. Among other things, they considered what constitutes a better dosing device through a system innovation model mechanism that can deliver optimal compliance with therapy recommendations from doctors or pharmacists. This included inhalers and product design and usability’s role in medication adherence and patient outcomes. Enhancing pharmaceutical delivery systems, providing patients with safe and efficient treatments, and promoting adherence through counselling and teaching are all examples of good management practices in the healthcare industry. Since they actively evaluate and implement innovative treatment modalities and technologies that enhance patient care and provide positive results, the importance of healthcare managers cannot be overstated.
Nutbeam and Lloyd (2021) examined health literacy as a social determinant of health, highlighting the importance of evaluating patients’ varying degrees of competency. The deployment of strategies to remove obstacles associated with low literacy is part of optimal management in health care; these strategies should include the use of graphical aids and plain-language documents, as well as patient participation in shared decision-making. Healthcare managers can aid in this process by creating and endorsing staff training programs to improve health communication abilities and promote patient-centred care techniques to accommodate a range of needs and preferences.
Finally, there are several different parts of how managers care for patients. These include aspects like health knowledge, product design, and staff participation. But if healthcare organizations deal with these issues, they can make patients safer, improve the level of care, and improve health outcomes. Enabling cultures that make work better, innovative healthcare delivery systems and patient-centred strategies that consider what the customer wants are all examples of managerial reactions. If managers want to improve patient care and make sure that this course is taught safely and effectively, they should do everything they can to bring attention to the relationships between all the people involved, from patients to healthcare workers.
2.5 Leadership Styles and their Impact on Patient Care
Leadership styles significantly affect the workplace, how happy workers are, and how well patients are cared for. This is very important for patients’ health. Several studies have examined how different types of nursing leadership affect nurses’ job satisfaction, the culture of the organization, and the general quality of health care.
Moreover, Spechia et al. (2021) did a complete study of the link between leadership styles and nurse satisfaction in general. The study only indirectly mentioned transformational leadership. It found that nurses with a vision were inspired, intellectually stimulated, and cared for as individuals were happier with their jobs. Transformational leaders not only get people excited, but they also create an environment that encourages professional growth by being flexible. They also help the people below them succeed. More nurses stay with the company, they work together better, and patients do better.
The transformational leadership method was talked about by Robbins and Davidhizar (2020), along with some unique aspects of this style in health care. Transformational leaders are charismatic and inspire their followers to be confident and trusting. They also get their followers to reach their full potential as people. Transformational leadership and high-quality results go hand in hand in the health field. This is clear from the fact that employees are highly engaged and happy with their work environments. Leadership that changes things encourages people from different fields to work together, have a standard knowledge of patient-centred care, and be willing to support quality initiatives that make patients more concerned about their safety.
Kalkan et al. (2020) examined how school managers’ leadership styles, how the organization saw them, and the type of school culture were related. This study shows more effects of different leadership styles on operational parts and culture. It’s important to note that these effects are not limited to healthcare. Leadership style in the healthcare business affects how well patients are cared for, how happy employees are with their jobs and the organization’s culture. Good leaders also build a culture of safety and accountability so that workers see their bosses as valuable partners.
Finally, the leadership styles used to build healthcare facilities affect both the level of engagement among staff and the general culture of the facility, which in turn affects how well patients do. As a result of the transformational leadership style, nurses are happier with their jobs, employees are more engaged, and patients get better care. This is because the style is future-focused and visionary, and it uses an inspirational and personalized approach to get people involved in solving problems together, which gives each person more power. A culture of confidence and cooperation, where people are encouraged to learn new things, and where leaders push people to do their best work so that the team can succeed. Healthcare providers can create a culture of good leadership and high-quality patient care by learning how different leadership styles affect the organization and how well patients are cared for.
2.6 Literature Gap
There needs to be more studies on how leadership styles directly affect patients in healthcare facilities. Many studies have examined how different leadership types affect workplace cultures, worker happiness, and even how well medical care is delivered. However, no clear link has been found between leadership styles and patient outcomes like readmission rates, satisfaction scores, and death rates. Transformational leadership has also been shown to be a good predictor of good outcomes in the medical field, such as job satisfaction and staff commitment. However, more study needs to be done to determine the effect these high levels of patient care have on outcomes. Furthermore, concentrating on the distinct effects of alternative leadership philosophies, such as transactional, servant, and authentic leadership, which may influence patient outcomes, may provide insight into workable procedures in the medical field. Completing this gap in the literature could support clinical practices, organizational policies, and leadership development programs in the healthcare industry that aim to improve patient outcomes while elevating the standard of care
2.7 Conceptual Framework
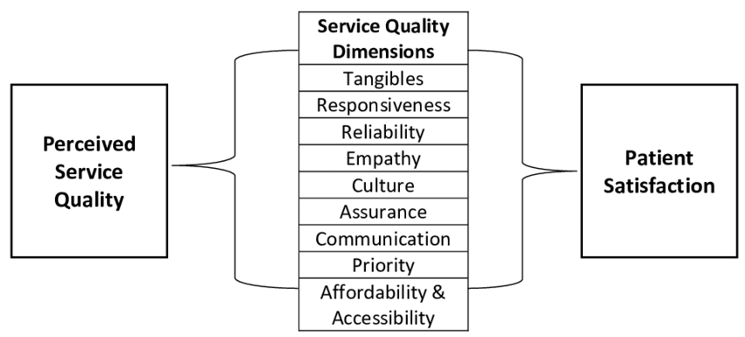
Figure: Conceptual Framework
Source: (Tetteh et al., 2021)
2.8 Summary
In summary, a thorough review of the literature on patient safety techniques, leadership philosophies, and how effective management affects patient care was presented in Chapter 2. Researchers concentrated on how leadership affects patient outcomes, organizational culture, and nurse work satisfaction. Transformational leadership emerged as a potent tool for raising employee engagement, fostering creativity, and raising product quality standards while showing concern for workers. Improved communication and appropriate identification techniques were among the instruments used to address patient safety, underscoring the multifaceted nature of the undertaking. Barriers to health literacy, workplace supportiveness, and effective drug delivery systems are highlighted by the patient care emphasis on management. While there are apparent gaps in the data, particularly on direct associations between leadership styles and patient outcomes, the various evaluated studies provided invaluable insights into the subtleties of healthcare leadership practices. To improve the health system’s performance as a whole, closing these gaps could be a source of information for organizational initiatives and evidence-based leadership development interventions. These interventions aim to deliver improved patient care.
References
Al-Worafi, Y., 2023. Patient safety in developing countries: Education, research, case studies. CRC Press.
Birken, S., Clary, A., Tabriz, A.A., Turner, K., Meza, R., Zizzi, A., Larson, M., Walker, J. and Charns, M., 2018. Middle managers’ role in implementing evidence-based practices in healthcare: a systematic review. Implementation Science, 13, pp.1-14.
Bond, G.R. and Drake, R.E., 2020. Assessing the fidelity of evidence-based practices: History and current status of a standardized measurement methodology. Administration and Policy in Mental Health and Mental Health Services Research, 47, pp.874-884.
Burgener, A.M., 2020. Enhancing communication to improve patient safety and to increase patient satisfaction. The health care manager, 39(3), pp.128-132.
Buttini, F., Quarta, E., Allegrini, C. and Lavorini, F., 2021. Understanding the importance of capsules in dry powder inhalers. Pharmaceutics, 13(11), p.1936.
Harvey, G., Kelly, J., Kitson, A., Thornton, K. and Owen, V., 2020. Leadership for evidence-based practice—Enforcing or enabling implementation? Collegian, 27(1), pp.57-62.
Hosseini‐Moghaddam, F., Mohammadpour, A., Bahri, N. and Mojalli, M., 2023. Nursing Managers’ perspectives on facilitators of and barriers to evidence‐based practice: A cross‐sectional study. Nursing Open, 10(9), pp.6237-6247.
Kalkan, Ü., Altınay Aksal, F., Altınay Gazi, Z., Atasoy, R. and Dağlı, G., 2020. The relationship between school administrators’ leadership styles, school culture, and organizational image. Sage Open, 10(1), p.2158244020902081.
Kitson, A.L., Harvey, G., Gifford, W., Hunter, S.C., Kelly, J., Cummings, G.G., Ehrenberg, A., Kislov, R., Pettersson, L., Wallin, L. and Wilson, P., 2021. How nursing leaders promote evidence‐based practice implementation at point‐of‐care: A four‐country exploratory study. Journal of Advanced Nursing, 77(5), pp.2447-2457.
Nutbeam, D. and Lloyd, J.E., 2021. Understanding and responding to health literacy as a social determinant of health. Annu Rev Public Health, 42(1), pp.159-73.
Piera-Jiménez, J., Dooling, J., Ranade-Kharkar, P., Pollock, S., Mann, D., Thornton, S., Duggal, R., Khatri, S., Shukla, B., Rudin, R. and Hillestad, R., 2020. Patient identification techniques–approaches, implications, and findings. Yearbook of medical informatics, 29(01), pp.081-086.
Renolen, Å., Hjaelmhult, E., Høye, S., Danbolt, L.J. and Kirkevold, M., 2020. Creating room for evidence‐based practice: Leader behaviour in hospital wards. Research in nursing & health, 43(1), pp.90-102.
Robbins, B. and Davidhizar, R., 2020. Transformational leadership in health care today. The Health Care Manager, 39(3), pp.117-121.
Sherwood, G. and Barnsteiner, J. eds., 2021. Quality and safety in nursing: A competency approach to improving outcomes. John Wiley & Sons.
Specchia, M.L., Cozzolino, M.R., Carini, E., Di Pilla, A., Galletti, C., Ricciardi, W. and Damiani, G., 2021. Leadership styles and nurses’ job satisfaction. Results of a systematic review. International journal of environmental research and public health, 18(4), p.1552.
Tetteh, I., Spaulding, A. and Ptukhina, M., 2021. Understanding the job-hopping syndrome among millennial employees in the US food and agribusiness sector: a national survey. International Food and Agribusiness Management Review, 24(1), pp.89-104.
Tucker, S., McNett, M., Mazurek Melnyk, B., Hanrahan, K., Hunter, S.C., Kim, B., Cullen, L. and Kitson, A., 2021. Implementation science: Application of evidence‐based practice models to improve healthcare quality. Worldviews on Evidence‐Based Nursing, 18(2), pp.76-84.
 write
write