Introduction
Youth suicide is a significant public health concern in the UK, with suicide remaining the leading cause of death for young people aged 20-34 years old. At the same time, research shows that young people face multiple barriers to accessing and engaging with mental health services and psychotherapy, including stigma, lack of motivation, and practical obstacles around the availability and cost of care (Memon et al., 2016). This disengagement from professional support places young people at an even higher risk of self-harm and suicide (Leavey et al., 2011).
There is growing evidence that telehealth solutions utilizing video, phone, and online communication can significantly enhance access to psychotherapy, overcoming many traditional barriers that prevent young people from obtaining help (Hilty et al., 2020). Nurse-led telehealth interventions also align with more comprehensive policies to modernize mental health services, promote prevention and early intervention, and capitalize on technology to provide patient-centered care.
This assignment aims to critically evaluate the literature regarding youth engagement in psychotherapy and propose a realistic, evidence-based telehealth program led by mental health nurses to encourage young people to access counseling support. The intended outcome is to increase service uptake and continuity of care, thereby reducing suicide risk among this vulnerable population. Background drivers, appraisal methodology, and key themes from selected literature will be discussed. Conclusions will summarize evidence gaps and recommendations for practice, research, and policy to support future implementation of youth telehealth.
Background
Youths at risk of suicide often fail to access essential mental health services due to barriers like stigma, lack of awareness, cost, and availability of local services (Memon et al., 2016). With suicide remaining the biggest killer of young people aged 20-34 in the UK, there is an urgent need for evidence-based, youth-friendly interventions aimed at encouraging psychotherapy engagement and continuity of care to mitigate suicide risk.
National policy directives strongly mandate developing telehealth solutions to enhance access to psychotherapies. NHS Long Term Plan (2019) aims to accelerate the expansion of digital and remote healthcare while noting that currently, only 3% of mental health interactions occur online. Youth mental health frameworks specifically promote technology-enabled care models to overcome traditional barriers around self-stigma, motivation, and service availability for this group. Clinical guidelines equally endorse tele-mental health for its capacity to increase service uptake and adherence when used appropriately.
The COVID-19 pandemic lent further impetus to the rapid adoption of telehealth, necessitating a shift to remote consultations while limiting in-person interactions. What began as an emergency response yielded valuable learning about the viability of virtual models. Evidence indicates that the telepsychiatry uptake increased exponentially during COVID-19 while retaining comparable satisfaction and outcomes to face-to-face therapy for many patients (Pierce et al., 2022). Patients cited enhanced convenience and feelings of safety in their environment. For marginalized young people facing access inequities, there are calls to sustain telehealth options post-pandemic to support inclusion in care.
Nurses are ideally positioned to lead telehealth services supporting mental health and suicide prevention among vulnerable young people in the community. Specialist mental health nurses have the clinical knowledge to assess suicide risk and deliver psychotherapy via digital platforms. Their holistic focus suits the psychosocial needs of young populations while nursing informatic skills enable safe and ethical virtual care provision. Introducing nurse-led telehealth aligns with more comprehensive recommendations for nurses to assume enhanced roles in youth mental healthcare. Advanced nurse practitioners equally have the decision-making autonomy to manage patient e-consultations, referrals, and interdisciplinary collaboration required for integrated telehealth programs.
Generally, introducing a telehealth psychotherapy consult and follow-up service for at-risk youths led by specialty mental health nurses could provide an evidence-based pathway to:
- Increase accessibility, engagement, and continuity of mental health support by overcoming traditional barriers of stigma, location, cost, and motivation
- Enable early suicide risk detection and timely crisis response through continuous digital monitoring
- Promote self-management and peer support options key to youth independence
- Yield cost and resource efficiencies to a strained mental health system through appropriate task shifting to nurse-led teleconsultations.
- Retain pandemic-driven momentum for inclusive virtual care that elevates patient preferences.
Literature Review and Discussion
Barriers and Facilitators to Psychotherapy Engagement Among Young People
Young people face multifaceted barriers to engaging in mental health treatment and psychotherapy. A prevalent obstacle is stigma, encompassing self-stigma and perceived public stigma, which generates fears of judgment or discrimination for seeking help (Clement et al., 2015). Confidentiality concerns also deter openness regarding emotions or symptoms. Young men especially exhibit stigma influenced by masculine norms around self-reliance and avoidance of vulnerability, equating help-seeking to weakness (Seidler et al., 2016). Getting support clashes with male gender role expectations. Relatedly, young people across genders who endorse autonomy values are less inclined to seek care, according to research by Mo and colleagues (2022), desiring to handle emotional issues independently first before reaching out.
The above stigma barriers disproportionately impact marginalized youth like racial, ethnic, and sexual minorities who may encounter layered stereotypes within health services. Minority stress compounds stigma effects in deterring disclosure of mental health struggles or suicide ideation to providers. Structural stigma also reduces service availability in lower socioeconomic regions, with health disparities frequently overlapping areas of deprivation (Burton et al., 2020). This exacerbates barriers to getting to appointments with limited transport options. Stigma erodes many youths’ capability to navigate complex systems to find appropriate evidence-based therapies.
Practical access obstacles impede youth mental healthcare, including cost constraints, transport issues, limited local services, and appointment availability not aligning with school or work schedules (Burns & Birrell, 2014). Competing priorities like education, relationships, and employment may be prioritized over therapy. Uncertainty navigating health systems further hampers help-seeking capabilities for adolescents still developing health literacy skills (Leavey et al., 2011). Parents may resist therapy referrals linked to perceptions of lousy parenting if children require support. With guardians’ facilitation, young people can access specialist services.
Conversely, dedicated services facilitate engagement by accommodating young people’s developmental needs for autonomy, identity formation, and independence (NHSE, 2018). Trained youth health coordinators in community settings like schools and youth centers enable informal drop-in consultations, alleviating many access barriers around stigma, travel, or scheduling. Here, adolescents can explore therapy options privately before consenting parents. Explicit opt-out consent processes also boost uptake for school-based mental health programs.
Targeted outreach like online messaging, text reminders, or helplines with extended hours suit youth’s inclination to self-manage issues using informal support before seeking professional interventions. Positive social support plus modeled examples of therapy effectiveness through peer champion testimonials encourage uptake when incorporated into engagement campaigns (Xu et al., 2018). Financial incentives for attending initial sessions may assist, alongside measures to enhance youth readiness contemplating help-seeking (Mellor, 2014). Intake adaptations to enable joint peer referrals reduce solitary onus.
Stigma-reduction strategies remain vital; seeing one-third of teenagers reporting self-judgment would prevent seeking care for suicidal thoughts or self-harm behaviors. School partnerships are well-placed to address beliefs using validated contact-based education, correcting myths around therapy effectiveness. Curriculums co-designedco-designedco-designed alongside youth ensure anti-stigma content reflects lived experience. Simultaneously securing private digital access points via school portals fosters help-seeking intentions by bypassing public-facing services. Sensitive engagement training for frontline staff builds trust in answering adolescent queries.
Technology-Based Mental Health Interventions for Young People
Digital platforms present new modalities for youth mental healthcare provision, matching young cohorts’ pronounced technological preferences and digital fluency. Online portals designed in partnership with youth offer alternative self-referral pathways to guide appropriate therapy selection while bypassing common access barriers like in-person intake appointments (Kauer et al., 2017). Webchat functions mimic the informal support adolescents often leverage from peers, with availability outside school hours. This extends help-seeking opportunities. Portals may link to specialized services like substance misuse or sexual health, integrating overlapping support.
Messaging interventions build continuous connections via non-intrusive check-ins to monitor youth well-being, utilizing preferred communication mediums like texts or instant messaging (Agyapong et al., 2016). Two-way crisis response protocols enable distress disclosure via simple help messages with swift specialist nurse triaging to contain situations or dispatch assistance. Daily motivational messages or goal-setting prompts equally assist behavior modifications, while information texts deliver helpful psychoeducation and mental health literacy.
Mobile apps provide convenient self-monitoring of moods plus personalized coping strategies like positive affirmations or distraction techniques directly through adolescents’ smartphones, fostering independence (Tighe et al., 2017). Gamification elements enhance enjoyment while tracking lifestyle stability indicators like sleep and diet, which influence mental health. Data visualization tools illustrate personal triggers and stability patterns. Apps may passively link users to crisis helplines based on usage data indicative of heightened risk or offer peer support through moderated forums, allowing anonymous interactions with other youths sharing mental health experiences. While apps vary significantly in quality evidence, collaborative youth-centered design with adolescent focus group input during development and evaluation stages is widely advocated to enable tailored functionality that adolescents find engaging (Ben-Yehuda et al., 2022). Co-designCo-designCo-design also suits youths’ need for autonomy.
Video interventions expand access options by leveraging familiar platforms like Skype or Zoom that young people use for everyday communication. Simulated skills training delivers targeted mental health education modeled on video games young people play through avatars enacting supportive peer dynamics (Bul, 2016). This interactive format increased perceived connection and care continuity intentions versus static e-learning when trialed with depressed adolescents. Avatar consultations enable relatable therapy introduction in a less intimidating way than confronting specialist appointments. The option to change avatar appearance and form self-representational images additionally empowers identity exploration beneficial before disclosing to providers.
Complete telepsychiatry platforms offer flexible appointment timing from preferred locations, mitigating common barriers for marginalized youth around cost, transport access, and the inconvenience of taking time away from school or work. Video communication increases perceived support versus phone calls, attributed partially to enabling observation of nonverbal cues and visual rapport development between parties. Seeing clinician’s facial expressions fosters openness in teenagers. For those less comfortable verbally expressing emotions, platforms incorporating text chat and image sharing widen participation channels (Ahs et al., 2023). This flexibility improves experience ratings consistently associated with telemedicine adherence.
Telecounseling sessions furthermore allow convenient family group therapy, maintaining collaborative support while overcoming logistical difficulties in getting all members in one location during traditional in-person interventions. This format is equally effective in treating numerous youth mental disorders, maximizing available expertise through teleconferencing between generalist community providers like school counselors with specialized psychiatrists otherwise inaccessible to rural areas. Care coordination is streamlined across the group.
Augmenting therapy provision through youth digital fluency relies on accessible design principles tailoring tools for neurodiverse conditions or literacy barriers facing disadvantaged students (Burton et al., 2020). Ensuring website compatibility with screen-readers and offering subtitles on videos boosts inclusion. Apps require clinical oversight, checking symptom monitoring algorithms against escalation protocols to contain digitization risks from over-reliance on automated bot responses. Development frameworks emphasizing youth participatory design plus independent user testing harness firsthand feedback, optimizing relatability and safety.
Effectiveness Of Telehealth for Psychotherapy and Suicide Prevention
A growing evidence base demonstrates that telepsychiatry is comparable to in-person psychotherapy across mental health conditions frequently encountered among at-risk young people. High satisfaction rates indicate teletherapy helps overcome traditional access obstacles by being more convenient while offering privacy benefits and providing openness for teenagers hesitant to discuss emotions or suicidal thoughts face-to-face (Ahs et al., 2023). Video platforms enable observation of non-verbal cues and relationship building cited as equivalent to physical presence, overcoming early concerns that technology could impede therapeutic connections for this age group. Customization features like choosing the video background improve one university’s youth telepsychotherapy program.
For common adolescent conditions like depression and anxiety, which escalate suicide risk if left untreated, systematic reviews establish that teletherapy achieves parallel outcomes to traditional therapy for symptom remission and emotional functioning (Etzelmueller et al., 2022). Non-inferiority indicates remote options could expand service capacity without compromising care standards while enhancing continuity through mitigating disruption from youth mobility associated with transitional ages (Connolly et al., 2021). School-linked telemental health furthermore increased help-seeking behaviors among teenagers exhibiting internalizing psychological distress in one US secondary school program.
Qualitative feedback from young people in rural areas indicates enhanced continuity compared to traveling outside local areas to access external specialized services during unwell periods (Allison et al., 2021). The absence of disruptive transit alleviated stress around appointments. Local care, therefore, facilitated willingness for future care re-engagement as needed to manage recurring conditions or quickly re-enter treatment during crises, thereby preventing deterioration. Maintaining community connections is a recognized protective factor as youth transition to independence, so local system integration applies these protective elements to clinical services.
For suicidal young people, some research indicates potential advantages of elemental healthcare linked to quick virtual access from home, enabling faster containment compared to lengthy waiting and travel necessitated within traditional services. This mitigates risk during periods of ambivalence about living experienced by some suicidal youths. Others highlight the ease of disclosing suicidal ideation online due to enhanced anonymity, facilitating intervention (Memon et al., 2018). However, legal and ethical complexities persist around remote risk assessment and upholding emergency response protocols across jurisdictions. Global positioning systems tracking youth locations contain risk when not physically present with providers, but tools require robust testing.
Collaborative cross-sector efforts continue evolving national standards for telehealth-enabled youth suicide prevention and technology-augmented aftercare. School partnerships show promise, with protocols to swiftly share risk information and coordinate multidisciplinary containment plans with community services enabled through secure digital networks. Terminology standardization also assists in appropriate triaging between crisis lines, online counseling platforms, and acute telepsychiatry based on suicidal severity markers.
Youths highlight that social components like peer discussion forums reduce isolation in video interventions but need moderation to ensure positive exchanges. This prevents online harassment seen in some digital spaces. Structured messaging tools are being designed to capture lived experience narratives youth develop together, which clinicians integrate guiding therapeutic reflections on past resilience (Allison et al., 2021). Building continuity infrastructure around transitional ages as adolescents exit child services remains imperative but needs to be improved in systems focused on early intervention endpoints.
Nursing Role in Telehealth And Youth Mental Healthcare
Nurses are poised to coordinate expanded access to tele-mental health support, aligning with their psychosocial focus and central role in navigating multidisciplinary systems of care (Koivunen et al., 2016). Core nursing training equips nurses in holistic biopsychosocial assessment, compassionate client relationships, and evidence-based care provision – skillsets transferable for delivery across telehealth platforms. Informatics capabilities gained through contemporary curriculums ensure nursing graduates are conversant in applying digital technologies to augment healthcare access and outcomes. This enables a comfortable transition into text consultation roles, the development of supportive mobile app services, and advanced telepsychiatry and telecounseling programs incorporating video and audio connections. Therapeutic communication foundations emphasize person-centered interactions equally applicable to virtual delivery, where seeing the young person on camera reinforces individualized support.
Advanced nurse practitioners possess advanced knowledge that is ideal for telehealth leadership, enabling robust clinical application of technology-assisted therapies while gathering practice-based evidence through robust evaluation frameworks (National Institute of Mental Health, 2019). Youth mental health nursing specialization equips practitioners for roles like teleprimary therapy, remote psychiatric assessment, collaborative care planning, and medication management – all adaptable for integrated virtual models (Kolovos et al., 2022). ANPs are qualified to screen tools like text algorithms or mood apps appropriately to determine when digital self-help interventions require escalation to direct therapist guidance. This supports stepped care principles and optimizes resource use. ANPs additionally understand youth-specific crisis response needs and can provide intensive tele-case management to frequently hospitalized young patients as part of the continuity of care initiatives (Salazar de Pablo et al., 2022).
Expanding nursing duties across telehealth modes necessitates updated training to uphold competence in delivering evidence-based virtual practice. Simulated learning dealing with digital risk assessment scenarios or telephone de-escalation are examples. Core ethical principles around therapeutic boundaries must be re-considered regarding electronic interactions where over-disclosure might increase due to online disinhibition effects. Nurses require a greater understanding of jurisdictions’ civil liability laws related to duty of care in telehealth.
The broader adoption of remote care prompts policy modernization, including updates to nursing regulatory standards and ethical codes reflecting telehealth-focused competencies, consent precedents, and emergency response pathways for technology-based therapies (ANA, 2021). National nursing agencies actively seek clinician input on draft telehealth codes, considering balances between risks like confidentiality breaches and the benefits of increased mental health service access for disadvantaged groups. Employers must provide adequate vicarious trauma support, given increased exposure to distressing situations in which nurses cannot directly intervene physically through a screen.
At service planning stages, individualized determinations of telehealth suitability should be made collaboratively with young patients considering needs, preferences, risks, and home environment. Cultural factors influencing family involvement require attention and securing private spaces conducive to video therapies. Nursing advocacy is fundamental across policy levels to progress equitable access for marginalized young people reliant on remote options (Cobo, 2022). Many pandemic-initiated telehealth expansions risk being rolled back without vocal nursing champions. Sustaining flexible youth access to dedicated nurse-led virtual mental health teams could provide lifesaving continuity.
Standardized terminologies ensure appropriate triaging between modalities like crisis chat, counseling platforms, and acute telepsychiatry based on symptom severity markers. As nurses coordinate escalations, training in leading efficient interdisciplinary handovers mitigates risks of sharing responsibility between providers. Simulation exercises prepare nurses for legal duties, delivering care across geographic boundaries (Mitchell et al., 2016). While telemental health promises expanded service access, complex needs youth still require focused support guided by cultural safety principles rather than one-size-fits-all virtual solutions.
Comparison of findings across studies
Comparing research on barriers facing youths accessing psychotherapy indicates certain common obstacles like stigma, scheduling conflicts, and cost issues recur frequently as deterrents to initial or sustained treatment engagement (Leavey et al., 2011). Self-stigma triggers are remarkably consistent across cultural contexts, although some differentiation is observable between more individualistic versus collectivist communities in how youth interpret stigma implications.
Technology-based interventions demonstrate broadly consistent acceptability, indicating channels matching youths’ digital preferences and fluent usage hold the promise of expanding care access (Ben-Yehuda et al., 2022). However, variability in effectiveness data signals a need to homogenize reporting metrics and comparisons within trial designs to gauge impacts conclusively. Widely differing mobile app design components confuse aggregating usability results, weakening generalizability. Researchers acknowledge that more multicenter collaborative trials are needed rather than isolated small studies underway presently.
On telehealth psychotherapy outcomes for ordinary youth mental illnesses, data homogenously shows comparable symptom and functional results to in-person services while improving attendance rates (Etzelmueller et al., 2022). Universal feedback from young people using teletherapy includes favorable convenience/access and privacy themes. However, individuals’ relative weight on each benefit alters slightly by geography, whether rural versus urban, hypothetically linked to baseline variability in local system access or infrastructure development. Some cultural variability detected in therapy alliance development rates suggests further cultural competence enhancement is needed to attune telepsychiatry provision for minority groups.
The COVID-19 shift eliciting telehealth integration nationally allows valuable comparative assessment between regions at different adoption phases. Spikes in video consult utilization during lockdowns consistently maintained mental healthcare access despite reduced in-person availability. Nevertheless, sites with historically limited telemedicine capacity pre-pandemic saw more significant care continuity challenges, and rural areas with technology infrastructure limitations experienced variable effectiveness, partly overcoming traditional access barriers. These learnings reaffirm that implementation success relies on a combination of service readiness, community-centered co-designco-designco-design, and network planning.
The gaps in evidence
Despite accelerating evidence assessing youth telepsychiatry, research gaps still need to be addressed, particularly in examining long-term adherence and engagement beyond initial uptake facilitators. While studies consistently evidence strong acceptance and comparable clinical outcomes to established services during early phases, data regarding retention patterns for youths utilizing exclusive teletherapy with no treatment escalation to in-person modalities is scarce. Retention predictors like continuity and emergency planning for digitally managed patients also need elucidation.
Additionally, further research should explore evolving best practices for crisis response conducted entirely remotely for suicidal youths requiring containment without the availability of in-person admission units due to location barriers facing rural groups. Legal and ethical precedents combined with care protocols have uncertain evidence foundations despite the high need to uphold youth safety through virtual networks when maintaining community connections. Exploring tools like home safety risk assessment questionnaires and GPS tracking systems could strengthen guardians’ capability to support adolescents remotely where imagining risks persists.
Finally, continued investigation of relevant competencies for nurses stepping into telehealth coordinator roles focused on whole-system youth pathways is recommended, such as ideal training frameworks balancing core therapeutic skills, risk literacy, digital ethics, and cross-sector care navigation capabilities needed for seamless integration (National Institute of Mental Health, 2019). Refining relevant evaluation frameworks offers another gap benefiting from attention. Determining meaningful metrics suited to diverse telehealth modalities, from text exchanges to avatars through videoconferencing, allows balanced comparisons and aggregated quantitative syntheses that are currently lacking.
Ethical, legal, and political perspectives
Ethics
Delivering youth telepsychiatry prompts multidimensional ethical considerations regarding privacy, duty of care, emergency planning, ensuring accountable use of public data systems, and respecting young patients’ confidentiality while communicating risk information across providers or services nuanced consent balancing (McLennan, 2016). Teenagers deemed competent for autonomous healthcare choices require involvement in collaborative decision-making regarding data sharing and therapy modalities. Transparent digital usage policies outlining access procedures reinforce ethical practice. Additional consent adaptations suiting youth developmental stages may empower choices, like opt-out processes enabling more straightforward engagement with school services while upholding voluntary participation (Robards et al., 2019).
However, determining adolescents’ mental capacity around healthcare decisions remains complex, potentially impeding awareness of teletherapy risks like parental discovery of sessions. Screening tools assessing comprehension of technology-based therapy processes require investigation, given that eHealth literacy varies greatly across young demographics. Individualized discussion of online versus offline suitability factors could tailor suitability while respecting youth autonomy (Wang et al., 2022). This equilibrium enables support accessibility.
Protecting vulnerable youth also warrants consideration where intersectional attributes like homelessness or domestic issues increase surveillance threats if digital therapy engagement is traceable at personal risk (Burton et al., 2020). Here, nurses are ethically bound to advocate policy solutions enabling safe youth participation. Similarly, digital exclusion factors facing disadvantaged groups call for equitable telehealth access provisions suited to diverse needs.
Legal
Delivering telemental health prompts extensive legal analysis regarding professional liability, cross-border practice allowances, and medico-legal frameworks enabling digital crisis response. Youth telepsychiatry frequently involves interdisciplinary collaboration between nurses, counselors, schools, and guardians, detailing each provider type’s supervised scope of practice. Participating in integrated networks boosts care quality by reducing risks of overstepping practitioner competencies (Dobson et al., 2020). Statutory college documentation should provide clear disciplinary authority guidance, including differentiating acts considered controlled digital practice versus informational resource sharing permitted across roles.
For suicidal youths, the nurse’s legal duty varies based on patient proximity during virtual consultations. Rapidly evolving legislation tries to delineate reasonable crisis response expectations for nurses unable to physically attend and transport patients directly when risk is identified through the screen. Tracking geo-located youth until first responders’ arrival is an emerging alternative, although it places responsibility strains on individual nurses. Clear position statements boost consistency.
Considering youth legal rights for consent also warrants alignment to telehealth contexts, balancing confidential therapeutic alliances with guardian rights accessing children’s health information. Nuances around competence determination principles and data transparency protocols adapted for digital systems enable equitable youth access while respecting caregiver protection roles, preventing unilateral exclusion that could deter engagement.
Political
Youths’ rightful access to responsive mental healthcare free from service inequities or social marginalization should frame political advocacy around telepsychiatry policies. Telehealth legislation lifting geographic restrictions on virtual practice may enhance support continuity for mobile youth groups like college students or military families. However, critics argue that digital cost-efficiency narratives promote decentralized models lacking holistic care coordination, risking fragmented youth pathways through streamlined virtual services.
Political commitments sustaining pandemic-initiated telepsychiatry funding despite shifting priorities also remain uncertain, jeopardizing recently expanded community access points now easily retracted unless mobilized nurse advocacy convinces decision-makers of lifesaving impacts from consistent digitally enabled self-help and peer support openings for marginalized teenagers (Cobo, 2022). Telehealth utilization metrics demonstrating success in engaging challenging cohorts like homeless youths or gang-affiliated populations equally build political will for sustained investments in innovative models. Communicating protective cost-offsets from prevented crisis interventions strengthens economic arguments given limited budgets.
Literature Search Process
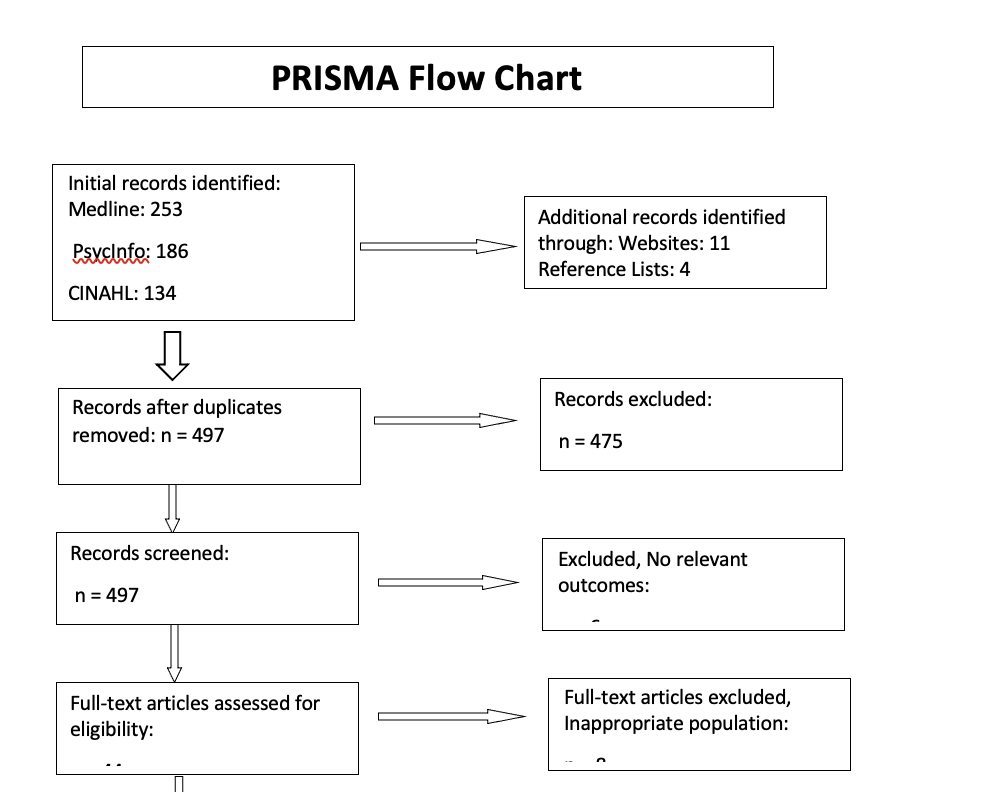
A comprehensive literature review explored research into barriers and enablers influencing youth engagement with psychotherapy, existing technology-supported mental health interventions tailored for young people, effectiveness evidence regarding telehealth-enabled psychotherapy and suicide prevention, and evolving nursing roles in virtual therapeutic delivery.
Searches utilized Medline, PubMed, CINAHL, PsycINFO, and Embase databases, given the focus on psychosocial and health systems, which are pertinent to selected themes. Initial search terms covered concept areas of “youth OR adolescent,” AND “mental health OR psychotherapy,” AND “access OR engagement,” AND “technology OR mhealth OR telehealth OR telepsychiatry OR digital,” AND “nurs*”. Age filters were applied consistent with literature cutoffs for youth population definitions, alongside English language and timeline specifications restricting evidence to the last ten years, ensuring contemporary relevance.
As searches yielded over 5000 articles, additional filters were added to refine results aligned with assignment aims. Inclusion criteria encompassed 1) youth aged 10-24 years, 2) community care settings, and 3) UK or comparably developed nations. Exclusion criteria removed 1) proprietary digital products lacking peer review 2) multifaceted organizational interventions without discrete telehealth elements 3) complex needs groups (i.e., justice systems, severe disability, homelessness) given tailored considerations.
Recognizing rapid evidence generation in nascent digital health fields, hand searching additionally captured more salient reports from national health agencies and a 2022 systematic review. Recent texts provided supplementary perspectives regarding cross-disciplinary competencies for nurse telepractitioners, ethical processes for virtual healthcare, and advocacy priorities sustaining pandemic-initiated telepsychiatry gains.
Figure 1: Search Terms Table
| Concept 1 | Concept 2 | Concept 3 | Concept 4 |
| youth OR adolescent OR teenagers OR “young people” OR “young adults” OR students | psychotherapy* OR counseling OR “mental health service” OR “mental healthcare.” | telehealth OR telepsychiatry OR telemental OR technology OR “mobile health” OR digital OR online OR virtual OR app OR application | access OR engage* OR facilitate* OR barrier* OR deter* OR prevent OR hinder |
| help-seek* OR “service uptake” OR adherence OR compliance OR usage OR continuity OR retention OR motivation | therapy OR intervention OR treatment OR program* | video OR avatar OR text OR messaging OR “social media” | nurse OR nursing OR “mental health nurse” OR “psychiatric nurse” |
| CBT OR “cognitive behavior?oral therapy” | platform OR portal OR “online community” OR “support group” | competent* OR qualification* OR training OR education OR skills OR standards OR protocol* | |
| counsel* OR “school counselor” OR psychologist | smartphone OR phone OR computer OR laptop OR tablet OR “mobile device” | guideline* OR framework OR legislation OR mandate OR policy | |
| “mental health disorder” OR depression OR anxiety OR PTSD OR “self-harm” OR suicide* OR “suicidal ideation” |
Literature Appraisal Method
CASP (Critical Appraisal Skills Programme) checklists were utilized given applicability for appraising varied research methodologies, including qualitative inquiries that yielded youth perceptual data on access barriers and telehealth experiences complementing clinical trials evaluating efficacy. CASP tools align with principles valuing methodological coherence between research goals and design while ensuring ethical dimensions are considered (Aveyard et al., 2016). The mixed-methods feature enables unified appraisal.
CASP criteria additionally encompass detailed considerations regarding recruitment and data handling procedures, enabling reviewers to assess biases and generalizability. These facets were particularly relevant given that telepsychiatry research spanned community therapy trials and exploratory pilot studies testing nursing-led prototypes at single sites. The risk of coverage error was heightened for geographically confined digitally based interventions often trialed among specific university cohorts. Reviewing sampling techniques and disclosures of trial limitations mitigated this.
Summary
This literature review analyzing components for a nurse-led telehealth intervention aimed at boosting youth psychotherapy engagement reveals multifaceted considerations spanning barriers deterring initial access to outcomes evaluating retention. Stigma consistently emerges as an obstacle across studies, aligning with broader evidence that self-judgment deters care-seeking behaviors crucial for suicide prevention among at-risk adolescents in the community. Parental misconceptions around therapy necessity also require addressing to enable uptake and continued participation through guardian support like transport provision. Meanwhile, practical barriers exacerbate stigma, especially for rural or lower-income youths facing compounding access inequities (Xu et al., 2018). Here, outreach answering common questions and financial incentives temporarily overcoming cost impediments may assist in connecting marginalized teenagers to lifesaving services at critical junctures.
Transitioning evidence-based psychotherapies to digital platforms shows promising indications of equivalent efficacy to in-person modalities while enhancing youth convenience, privacy, and accessibility values, which could lead to sustained engagement patterns. Tempering this optimism, long-term retention data in exclusively virtual models still needs to be explored, warranting further research. Explorations of how digitally enabled care coordination across stepped platforms balancing self-guided tools like text messages and apps with escalation pathways to acute telepsychiatry require additional testing to optimize resource allocation supporting whole journey needs. As adolescents transition to independence, continuity between modalities prevents care breakdowns during life changes. Clear emergency protocols for telehealth providers to activate local crisis networks for at-risk youth equally deserve elucidation so nurses can uphold safety standards in digital environments.
Advanced practice nurses possess suitable capabilities to coordinate multifaceted system access, clinical therapy, and networked psychosocial wellness resources to enable integrated youth telepsychiatry centered around individual preferences while containing risk (National Institute of Mental Health, 2019). Optimizing this potential relies on updated regulatory and ethical guidance delineating supervised responsibilities across telehealth network roles to reinforce coordinated practice. Additionally, refined accreditation processes and simulation-based training will further strengthen nursing competencies, managing virtual care teams and mitigating digitally enabled risks like confidentiality breaches (Sullivan et al., 2022).
Key learnings indicate that nurse-led telepsychiatry teams overseeing diverse modalities, from supportive check-ins to video therapy, provide robust infrastructure boosting youth access and engagement with vital mental health interventions to prevent suicide. Capitalizing on adolescent digital fluency and enhancing choice/self-management foster service uptake plus perceived continuity intentions that promisingly overflow into sustainable help-seeking patterns. Considering flexible combinations, maximizing individual preference retains engagement, while staged intensity aligns limited expertise. Centering youth participatory design in ongoing optimization sustains responsiveness, ensuring models evolve alongside future technological disruption and generational preferences retain relevance.
Sustaining recent progress nevertheless requires policy vigilance and advocacy countering real risks that pandemic-catalyzed telepsychiatry investments quickly retract before reaching full potential in helping vulnerable youths without vocal nursing champions evidencing lifesaving applications. Research limitations around long-term youth adherence patterns in digitally mediated therapies warrant acknowledgment, alongside legal and ethical uncertainties facing nurses duty-bound upholding safety virtually. Addressing these complexities through exploratory scholarship strengthens foundations enabling nationwide implementation at scale. Evaluative data continuously input into clinical guidance and nursing competency frameworks will further consolidate gains, delivering streamlined crisis pathways and saving young lives.
References
Advanced clinical practice. (2019, June 28). Advanced clinical practice. Health Education England. https://www.hee.nhs.uk/our-work/advanced-clinical-practice
Agyapong, V. I. O., Mrklas, K., Juhás, M., Omeje, J., Ohinmaa, A., Dursun, S. M., & Greenshaw, A. J. (2016). A cross-sectional survey evaluating Text4Mood: a mobile health program to reduce psychological treatment gap in mental healthcare in Alberta through daily supportive text messages. BMC Psychiatry, 16(1). https://doi.org/10.1186/s12888-016-1104-2
Ahs, J. W., Ranheim, A., Eriksson, H., & Mazaheri, M. (2023). Encountering suffering in digital care: a qualitative study of providers’ experiences in telemental health care. BMC Health Services Research, 23(1). https://doi.org/10.1186/s12913-023-09367-x
Allison, B. A., Rea, S., Mikesell, L., & Perry, M. F. (2021). Adolescent and parent perceptions of telehealth visits: A mixed-methods study. Journal of Adolescent Health, 70(3). https://doi.org/10.1016/j.jadohealth.2021.09.028
ANA. (2021, February 4). Telehealth Information for Healthcare Professionals. ANA. https://www.nursingworld.org/practice-policy/telehealth/
Aveyard, H., Payne, S., & Preston, N. (2016). A Post-graduate’s Guide to Doing a Literature Review in Health and Social Care. In Google Books. McGraw-Hill Education. https://books.google.com/books/about/A_Post_Graduate_s_Guide_to_Doing_a_Liter.html?id=b_sZswEACAAJ
Ben-Yehuda, O., Dreazen, E., Koren, D., & Peleg, M. (2022). Participatory Design of a Mobile App to Safeguard Mental Resilience in the Context of Drug Use in Young Adults: Multi-Method Study. JMIR Formative Research, 6(2), e34477. https://doi.org/10.2196/34477
Bryant, W., Cordingley, K., Sims, K., Dokal-Marandi, J., Pritchard, H., Stannard, V., & Adamako, E. (2016). Collaborative research exploring mental health service user perspectives on acute inpatient occupational therapy. British Journal of Occupational Therapy, 79(10), 607–613. https://doi.org/10.1177/0308022616650899
Bul, K. C. M., Franken, I. H. A., Van der Oord, S., Kato, P. M., Danckaerts, M., Vreeke, L. J., Willems, A., van Oers, H. J. J., van den Heuvel, R., van Slagmaat, R., & Maras, A. (2016). Development and User Satisfaction of “Plan-It Commander,” a Serious Game for Children with ADHD. Games for Health Journal, 4(6), 502–512. https://doi.org/10.1089/g4h.2015.0021
Burns, J., & Birrell, E. (2014). Enhancing early engagement with mental health services by young people. Psychology Research and Behavior Management, 7(14), 303–312. https://doi.org/10.2147/prbm.s49151
Burton, A. (2020). Social prescribing for mental health: a guide to commissioning and delivery. https://citizen-network.org/uploads/attachment/339/social-prescribing-for-mental-health.pdf
CASP. (2022). CASP – Critical Appraisal Skills Programme. Critical Appraisal Skills Programme. https://casp-uk.net/
Clement, S., Schauman, O., Graham, T., Maggioni, F., Evans-Lacko, S., Bezborodovs, N., Morgan, C., Rüsch, N., Brown, J. S. L., & Thornicroft, G. (2015). What Is the Impact of Mental Health-related Stigma on Help-seeking? A Systematic Review of Quantitative and Qualitative Studies. Psychological Medicine, 45(01), 11–27. https://doi.org/10.1017/s0033291714000129
Cobo, C. S. (2022). Rethinking leadership and nursing care in the post-pandemic era. Revista Científica de La Sociedad de Enfermería Neurológica (English Ed.), 55(21), 2–4. https://doi.org/10.1016/j.sedeng.2022.03.001
Connolly, S. L., Miller, C. J., Lindsay, J. A., & Bauer, M. S. (2020). A systematic review of providers’ attitudes toward telemental health via videoconferencing. Clinical Psychology: Science and Practice, 27(2). https://doi.org/10.1111/cpsp.12311
Department of Health. (2012). Compassion in practice (p. 13). https://www.england.nhs.uk/wp-content/uploads/2012/12/compassion-in-practice.pdf
Dobson, H., Malpas, C. B., Burrell, A. J., Gurvich, C., Chen, L., Kulkarni, J., & Winton-Brown, T. (2020). Burnout and psychological distress amongst Australian healthcare workers during the COVID-19 pandemic. Australasian Psychiatry, 29(1), 103985622096504. https://doi.org/10.1177/1039856220965045
Etzelmueller, A., Vis, C., Karyotaki, E., Baumeister, H., Titov, N., Berking, M., Cuijpers, P., Riper, H., & Ebert, D. D. (2020). Effects of Internet-Based Cognitive Behavioral Therapy in Routine Care for Adults in Treatment for Depression and Anxiety: Systematic Review and Meta-Analysis. Journal of Medical Internet Research, 22(8), e18100. https://doi.org/10.2196/18100
Explorable. (2019). Sample Size – The Number of Observations in Research. Explorable.com. https://explorable.com/sample-size
Giesbrecht, E., Major, M. E., Fricke, M., Wener, P., van Egmond, M., Aarden, J. J., Brown, C. L., Pol, M., & van der Schaaf, M. (2023). Telerehabilitation Delivery in Canada and the Netherlands: Results of a Survey Study. JMIR Rehabilitation and Assistive Technologies, 10(14), e45448. https://doi.org/10.2196/45448
Hilty, D., Chan, S., Torous, J., Luo, J., & Boland, R. (2020). A Framework for Competencies for the Use of Mobile Technologies in Psychiatry and Medicine: Scoping Review. JMIR MHealth and UHealth, 8(2), e12229. https://doi.org/10.2196/12229
Kauer, S. D., Mangan, C., & Sanci, L. (2014). Do Online Mental Health Services Improve Help-Seeking for Young People? A Systematic Review. Journal of Medical Internet Research, 16(3), e66. https://doi.org/10.2196/jmir.3103
Keenan, A. J., Tsourtos, G., & Tieman, J. (2022). Promise and peril-defining ethical telehealth practice from the clinician and patient perspective: A qualitative study. DIGITAL HEALTH, 8(22), 205520762110703. https://doi.org/10.1177/20552076211070394
Koivunen, M., Anttila, M., Kuosmanen, L., Katajisto, J., & Välimäki, M. (2016). Team climate and attitudes toward information and communication technology among nurses on acute psychiatric wards. Informatics for Health and Social Care, 40(1), 79–90. https://doi.org/10.3109/17538157.2013.872112
Kolovos, S., van Dongen, J. M., Riper, H., Buntrock, C., Cuijpers, P., Ebert, D. D., Geraedts, A. S., Kenter, R. M., Nobis, S., Smith, A., Warmerdam, L., Hayden, J. A., van Tulder, M. W., & Bosmans, J. E. (2018). Cost-effectiveness of guided Internet-based interventions for depression in comparison with control conditions: An individual-participant data meta-analysis. Depression and Anxiety, 35(3), 209–219. https://doi.org/10.1002/da.22714
Leavey, G., Rothi, D., & Paul, R. (2011). Trust, autonomy, and relationships: The help-seeking preferences of young people in secondary level schools in London (UK). Journal of Adolescence, 34(4), 685–693. https://doi.org/10.1016/j.adolescence.2010.09.004
Mellor, C. (2014). School-based interventions targeting stigma of mental illness: a systematic review. The Psychiatric Bulletin, 38(4), 164–171. https://doi.org/10.1192/pb.bp.112.041723
Memon, A. M., Sharma, S. G., Mohite, S. S., & Jain, S. (2018). The role of online social networking on deliberate self-harm and suicidality in adolescents: A systematized review of literature. Indian Journal of Psychiatry, 60(4), 384–392. https://doi.org/10.4103/psychiatry.IndianJPsychiatry_414_17
Mitchell, C., McMillan, B., & Hagan, T. (2016). Mental health help-seeking behaviors in young adults. British Journal of General Practice, 67(654), 8–9. https://doi.org/10.3399/bjgp17x688453
National Institute of Mental Health. (2019). Technology and the future of mental health treatment. Www.nimh.nih.gov. https://www.nimh.nih.gov/health/topics/technology-and-the-future-of-mental-health-treatment
Plan, N. L. T. (2019). NHS Long Term Plan. NHS Long Term Plan. http://www.longtermplan.nhs.uk/
Robards, F., Kang, M., Usherwood, T., & Sanci, L. (2018). How Marginalized Young People Access, Engage With, and Navigate Healthcare Systems in the Digital Age: Systematic Review. Journal of Adolescent Health, 62(4), 365–381. https://doi.org/10.1016/j.jadohealth.2017.10.018
Salazar de Pablo, G., Soardo, L., Cabras, A., Pereira, J., Kaur, S., Besana, F., Arienti, V., Coronelli, F., Shin, J. I., Solmi, M., Petros, N., Carvalho, A. F., McGuire, P., & Fusar-Poli, P. (2022). Clinical outcomes in individuals at clinical high risk of psychosis who do not transition to psychosis: a meta-analysis. Epidemiology and Psychiatric Sciences, 31(33). https://doi.org/10.1017/s2045796021000639
Seidler, Z. E., Dawes, A. J., Rice, S. M., Oliffe, J. L., & Dhillon, H. M. (2016). The role of masculinity in men’s help-seeking for depression: A systematic review. Clinical Psychology Review, 49(1), 106–118. https://doi.org/10.1016/j.cpr.2016.09.002
Tighe, J., Shand, F., Ridani, R., Mackinnon, A., De La Mata, N., & Christensen, H. (2017). Ibobbly mobile health intervention for suicide prevention in Australian Indigenous youth: a pilot randomized controlled trial. BMJ Open, 7(1), e013518. https://doi.org/10.1136/bmjopen-2016-013518
Xu, Z., Huang, F., Kösters, M., Staiger, T., Becker, T., Thornicroft, G., & Rüsch, N. (2018). Effectiveness of interventions to promote help-seeking for mental health problems: systematic review and meta-analysis. Psychological Medicine, 48(16), 2658–2667. https://doi.org/10.1017/s0033291718001265
 write
write