Abstract: Battlefield Anesthesia and Pain Management Modernization
Modern warfare poses substantial challenges in terms of battlefield anaesthesia and pain control. This research proposal confirms the paradigm shift in this field as it offers how to utilize emerging technologies and innovative approaches that can change pain management on the battlefield. Therefore, by studying in-depth the disadvantages of existing methods (Hidalgo 2019) this research is not only meant to contribute to some promotion towards scientific knowledge but also a tribute to those people who heroically protect our freedom. By providing means to mitigate pain effectively for medics, we enhance the ability of our military force to tolerate suffering. This is a great remodelling of combat medical care – from responding physicians to doctors who initiate action for protecting and continuing the healthfulness of soldiers. One last thing: This research envisions a future where no soldier has to go through so much misery and suffering on the battlefield.
Picture: A wounded soldier

Source: https://www.britannica.com/science/battlefield-medicine
Executive Summary: Revolutionizing Battlefield Pain Management
The battleground – chaos, and uncertainty of violence present immense challenges to optimal anesthesia and effective pain control. Unlike the sterility of a hospital, operating room battlefields are caught up in scarcity of resources and logistical problems where threats lurk around every corner. The blend of these harsh realities makes traditional methods such as general anesthesia and opioid analgesics rare. Thus, wounded soldiers are forced to wait in excruciating pain before their treatment, and even everything around them – areas meant to protect the lives of people – multiply its torment when they extend every minute. This research proposal aims to introduce a new phase of pain management in warfare by using innovative technologies and novel approaches that will be used for this purpose.
This study explores enticing possibilities in emerging solutions by carefully analyzing the shortcomings of the present status quo. It covers wearable ultrasound tools that enable precise local nerve blocks, telemedicine platforms that provide counselings live counseling, and non-invasive neuromodulation methods to cure pain (Capogna et al., 2019; Gebhard et al., 2018). It extends beyond technology by suggesting innovative solutions, such as specialized combat injury point-of-care analgesia kits and advanced training in comprehensive pain management techniques to enable medical personnel to act promptly and confidently in challenging environments. Through attentive planning for implementation, this research aims to deliver the tools and information battlefield medics need to tackle pain sympathetically, quickly, and quickly. Finally, this endeavor is designed to minimize soldiers’ suffering and maximize their chances of a full recovery with healthy expectations for returning.
Image: Army helicopter retrieving an injured soldier to be transported to a mobile army surgical hospital (MASH) during the Korean War, July 1951.

Source: https://www.britannica.com/science/battlefield-medicine
Introduction: A Crucible of Pain, the Need for Change
On the battlefield, where everything is chaotic and violence emerges, intense trauma and unbearable pain are rejected guests. The adrenaline rush may obscure the initial pain of combat, but when that wears off, it becomes a crucible, hurting both the body and mind. However, wounded soldiers’ suffering becomes even more agonizing as traditional pain management methods do not help them that much. General anesthesia, the mainstay of hospital operating rooms, becomes untenable in resource-deprived situations where its unwieldy paraphernalia and dependence on professionals certified by a board proves logistically disastrous amid war’s jaggedly chaotic conditions (Hidalgo, 2019). Their adverse side effects – drowsy feeling, respiratory depression, and lowered cognitive function might even leave the soldiers vulnerable while fighting or being evacuated.
Problem Description: A Mix of Challenges for Pain Management on the Battlefield
The battlefield is not merely a field of two armies squaring off against each other, it is the crucible in which life and death dance unhappily together. When advances in medical technology have revolutionized surgical capabilities overall, the management of anaesthesia and pain relief present abounding challenges unique to wartime conditions in Roles of Care 2-3 (R2-3) settings. In this field, where fast response and successful pain relief are most critical, the weaknesses of current ones become strikingly clear with the need for a fundamentally new perspective:
- Limited Surgical Capacity: The current situation of R2-3 surgical support is at a disadvantage, due to a significant bottleneck in patient capacity. During the conflict, mobile surgical units often experience difficulty in keeping up with the influx of wounded personnel (Wunsch et al, 2017). Failure to provide prompt care has detrimental effects; it may result in increased morbidity, prolonged suffering and sometimes loss of life (Houghton & Simpson, 2012). Several factors contribute to this limited capacity:
- Bulky and cumbersome traditional equipment: The tremendous size and inertia of surgical instruments and machinery significantly limit basic mobility including the ability to move them forward where rapid intervention is essential (Houghton & Simpson, 2012). This logistical burden not only implies slower response times but also limits the accessibility of surgical care to more localised locations.
- Power and logistical dependencies: The organization of surgical stations in extreme sufficiently needs a lot of power resources along with complicated logistical support chains (Sheta et al., 2020). Furthermore, the lack of readily available power sources as well as intricate networks of supplies limits flexibility and deployability. Increasing time to provide care for everyone who needs it.
- Scarcity of specialized personnel: Yet, it often can be quite challenging to get qualified personnel like experienced anaesthesiologists and other highly specialized medical staff in forward areas – especially during high-intensity combat operations (Wunsch et al. 2017). This combination of lack of expertise, plus the limitations of traditional equipment and infrastructure leaves R2-3 settings constrained to a very rudimentary range when it comes to the complexity of surgical procedures.
These interdependent issues demand the design of new technologies focused on miniaturisation, which will provide support during surgery with consideration for size, weight power and logistic requirements (SWAP). Handling these limitations, we can significantly enhance the surgical capacity in R2-3 environments and as a result, transform mobile units into powerful and highly adaptive lifelines for injured troops. Consider frighteningly small modular surgical equipment that could be transported on foot and flown by drones run by alternative sources of power all this with no logistical impact. A revolution in surgical technology of this sort may open up the possibility for timely intervention, and better outcomes (around more lives saved) on a battleground.
Suboptimal Anaesthesia Techniques: The current practices in battlefield anaesthesia are as bold and the number of obstacles that dog these procedures means patients’ safety and comfort levels are compromised. These challenges not only exacerbate the suffering of wounded personnel but also pose potential risks to their vital injuries and overall recovery:
- Difficulties in securing optimal venous access: The peripheral veins are typically compromised during battlefield injuries making traditional intravenous (IV) anaesthesia a difficult and time-consuming endeavour (Houghton & Simpson, 2012). This delay in pain control can be a contributing factor to increased suffering and psychological distress, further jeopardizing the stabilization of vital signs which are critical for patient survival.
- Limitations of traditional monitoring equipment: Monitoring devices that are bulky and hungry for power do not perform well within the challenging environments of a battlefield (Houghton & Simpson, 2012). The absence of instant feedback on vital signs during anaesthesia poses a threat to patient safety, as medical staff operates blindly and may miss essential changes in conditions.
- Challenges in maintaining a sterile environment: In combat zones, the risk of contamination is even greater as battlefield conditions can compromise the sterility of anaesthetic equipment and increase the chances of infection (Houghton & Simpson, 2012). This vulnerability becomes even more noticeable when operating with limited resources and under intense pressure, perhaps effectively adding another layer of pain to an already wounded person.
To overcome these barriers, we need to embrace innovative anaesthesia technologies that are:
- Portable and readily deployable: Timely intervention and pain relief to wounded personnel depend on the availability of compact and lightweight equipment designed for quick transport, and setup in forward areas. Imagine anaesthesia systems easily integrated into tactical backpacks or carried by drones, ready to be used whenever and wherever required.
- Independent of complex power and logistical support: Technology that requires less power and logistical chains will increase operational agility and versatility (Houghton & Simpson, 2012). This not only helps to minimize dependence on scarce infrastructure but gives medics and surgical teams the capacity to function autonomously thus increasing the provision of care.
- Capable of alternative access routes: Anaesthesia delivered through alternative routes such as intraosseous or inhalational administration bypasses the challenges of compromised peripheral veins, resulting in not only more rapid pain relief but also a quicker stabilization process (Houghton and Simpson, 2012). Consider that instead of processing the long-drawn battle for IV access, anaesthesia can be administered through a painless and reliable intraosseous route which not only reduces time taken but also allows those attending to such a case to focus on other vital interventions.
- Equipped with advanced monitoring capabilities: With real-time feedback on vital signs yet in low-resource areas, compact and efficient monitoring devices can drastically enhance patient safety when administering anaesthesia. Envision lightweight, wearable sensors embedded in a combat uniform that can relay critical information about the condition of an individual who is wounded without delay to medical personnel so they can be prepared and respond adequately before health factors turn out irreversible.
These are only some cases that can illustrate the transformative power of new technologies in solving problems of battlefield anaesthesia. Continued research and development in fields like miniaturization, alternative power sources, and advanced sensors hold the promise of a future where battlefield anaesthesia is characterized by:
- Rapid and effective pain relief: Personnel who suffered wounds will no longer have to suffer the pain of waiting while medics deal with heavy equipment and limited resources. Consider a future where pain relief is given quickly and efficiently so patients can concentrate on the process of healing and strengthening.
- Enhanced patient safety: In this regard, observation of the patient’s condition in a real-time mode with highly advanced sensing technologies will ensure that medical personnel are always informed about their patients. This will significantly reduce the risks of anaesthesia-related complications and improve patients’ overall outcomes.
- Increased operational flexibility: Compact, modular power-independent equipment will provide medics and surgical teams with the ability to operate independently in forward areas. This would broaden the range of care and ensure that additional injured personnel receive necessary medical attention despite any restrictive factors during the war.
Battlefields are always crude but we can evolve surgical intervention for battlefield anaesthesia and pain management using the power of innovation that embraces modern technology. It is not just a technological whim; it stands for humanity, a promise given to alleviate pain and save lives in the chaos of war. In the pressure cooker of war, we can shape a future where every terrible injury is balanced by hope and resilience in managing pain effectively.
Methodology: Building Routes to Resolutions
This interdisciplinary study will analyze the issues and contribute to developing paradigm-shifted pain management. In this way, each aspect of this methodology is essential in gathering comprehensive data, investigating potential solutions, and translating academic research into compelling ground realities.
- Systematic Literature Review: This research is based on a comprehensive review of past knowledge. A critical review of peer-reviewed articles, military reports, and expert opinions will be given to analyze the current battlefield anesthesia and pain management levels as they are practiced. The main focus of this systematic review is to emphasize the most critical issues and limitations associated with current practices, besides revealing potential innovations regarding technology techniques and strategies. By so doing, this review will sketch out the plan for further search and mark the gaps waiting to be filled.
- Semi-structured Interviews: Closing the gap between theory and practice, in-depth interviews will be conducted with the main stakeholders. The military setting will be of paramount value to researchers, who talk and exchange with battlefield medics, pain management specialists, and technology inventors about the everyday problems that emerge in operations handling pain. These interviews will focus on the problems of lived reality for medics, delve into what needs and priorities are deemed relevant by those closest to patient care, and capture feedback about viable solutions. It ensures that the recommendations developed in this research component remain grounded by involving those affected most with current limitations.
- Quantitative Analysis: In relation to the empirical data, researchers will come across medical reports and statistics from previous wars. This critical analysis of past pain management protocols will aid in identifying the areas that need to be enhanced, evaluate if previously applied techniques worked well under different wartime scenarios and determine whether specific approaches are associated with patient outcomes. Since the study is armed with proper day to day research, it possesses quantifiable evidence that supports ideas of solutions based on facts having either influence or impact measurable.
- Pilot Studies: The research will go beyond the theoretical development of these concepts, but must convert them into practice using pilot studies. First, emerging technologies and innovative approaches will be tested in specially created settings which ideally should simulate the dynamic environment as closely as possible as it could occur in a field. These pilot studies will produce important data about the feasibility, efficacy and logistical concerns that stem from implementing new pain control systems. This component reduces risks by conducting thorough testing in strictly supervised settings, thus facilitating the transfer from theory to practice.
Expected Outcomes
The present planned research is meticulously structured to offer an in-depth understanding of the current status quo regarding battlefield anesthesia and pain control, uncovering promising tendencies for improvement. These anticipated results are not confined to purely academic; they aspire for tangible changes that will be useful to medics and improve the situation of those who suffer in war. The findings of this research hold the potential to inform the development of:
New training programs: Providing the skills and knowledge needed by medics to use advanced pain management technologies and techniques. Significantly, insights from the research can be used in designing tailor-made training programs that factor in a battlefield’s specific challenges and resource limitations.
Innovative point-of-care kits: Giving medics tools for rapid and effective pain management when the injury occurs. The research can direct the creation of small mobile kits designed to deal with typical battle-related injuries, complete with appropriate medications and tools optimized for quick use.
Collaborative partnerships: Further development of cooperation between military, academic, and industrial actors. The research could catalyze partnerships that will rely on diverse expertise to accelerate innovation and optimize pain management practices on the battlefield.
Finally, this research will help reach a point in the future when resources are available for battlefield surgeons to efficiently manage pain, relieve suffering, and create possibilities of survival and recovery chances among wounded soldiers. By carefully dismantling the difficulties, considering possible solutions, and converting results into practical progress, this research seeks to become a source of inspiration on the frontline, where each step to mitigate pain is one step towards winning.
Proposed Solutions: Managing Pain in the Battlefield
This research proposal advocates for a new age in pain management during the war, seeking to go beyond current constraints by adopting cutting-edge technology, devising novel solutions, and establishing collaborative ties. This ambitious vision aims to provide medics with the tools and knowledge they need to prepare themselves as proficient pain warriors who can relieve suffering, improve recovery rates, and save lives on a battlefield.
Embracing Emerging Technologies
A wave of innovative technologies full of pain potential will sweep the battlefield. Nowadays, portable ultrasound devices Lippincott & Wilkins, 2019allow for unprecedented clarity when conducting regional nerve blocks – a technique that entails blocking pain signals carried by specific nerves before they reach the brain. This is both a safe and highly effective method. A medic in combat with a hand-held ultrasound device to identify and blockade the peripheral nerve of an injured soldier, effectively stopping searing limb pain at once. Another promising idea is a telemedicine platform. Picture a doctor talking to a pain specialist with the help of his ruggedized tablet even though he is under fire, which ensures good care in every situation. The potential of non-invasive neuromodulation methods such as transcutaneous electrical nerve stimulation (TENS) and spinal cord stimuli techniques could be investigated to treat chronic pain caused by war injuries.
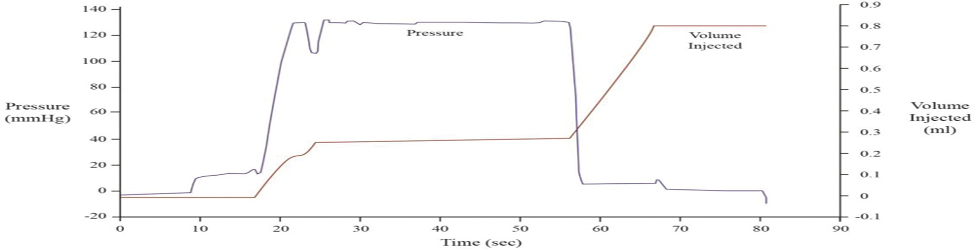
Figure 1: Typical pressure and volume display on the CompuFlo Epidural Computer Controlled Anesthesia System during epidural space identification. A dramatic pressure decline, followed by a formation of a low-pressure plateau, indicates that the epidural space has successfully been obtained. Regular saline injection ceases when the pressure reaches 130 mm Hg, which is set as the preset limit (Chaudhry& Agrawal, 2019).
Pioneering Innovative Approaches
Aside from technology, this research advocates taking up new point-of-care analgesia kits. For instance, instead of generic medication packs, medics could have kits to deal with particular combat injuries. Different kits may include specialized medications and peripheral nerve blocks for blast injuries, gunshot wounds, etc. Medics provided with such pre-stocked kits could act fast and confidently, providing immediate pain relief without taking time for complicated decision-making in the chaos of battle. More comprehensive training in highly advanced pain management techniques, such as peripheral nerve blocks and wound infiltration analgesia, would provide medics with enough skills to negotiate the various terrains of battle injuries. Think about simulated training with the Virtual reality approach for helping medics practice their abilities in lifelike situations before coping with such challenges as an injured comrade.
Fostering Collaborative Partnerships
Closing the gap between military medical teams, academic researchers, and medical device manufacturers is critical to speeding up solutions for leading-edge pain management. Collaborative initiatives can drive innovation by facilitating the following:
- Joint research and development projects: Integrating military clinicians, academic researchers, and engineers to design field-ready pain management technologies.
- Joint training programs: Developing and putting special training programs for medics into practice about the latest discoveries in pain management research and technology.
- Rapid dissemination of best practices: This might include implementing effective channels for communicating field practices that worked and improving pain management protocols in all branches and deployments.
An essential goal of this research towards facilitating such collaborations is establishing a dynamic environment where innovation thrives, and scientific breakthroughs could seamlessly form tangible upgrades for pain control on the battlefield.
Prioritizing Point-of-Injury Management
There needs to be a particularly relevant model of pain management for a hospital setting to the pressing battlefield needs. Change in the paradigm is recommended for research, focusing on point-of-injury intervention. Equipping medics with the tools and knowledge to manage pain at the site of injury offers profound benefits:
Reduced duration of suffering: By providing immediate pain relief at the wound site, we can significantly shorten their lengthy wait for treatment, help boost soldier morale, and create more successful recovery scenarios.
Lower risk of complications: Pain, if unattended for a considerable period, may further damage the existing injuries and even cause secondary complications.
Improved tactical advantage: ½ soiled soldiers with horrible pain are often much incapacitated, and they cannot move, fight, or evacuate safely. They become active participants in the mission through practical and timely pain management.
This strategic move requires the design of small, portable, easy-to-use pain management devices that can be used in battle. Think about a medic who quickly comes up and gets his single-use, pre-packaged nerve block kit out to stop the shooting pain in an ally’s arm so he stays in the line of duty.
Embracing Personalized Medicine
Individual soldiers have different pain profiles and physiological variations, which require the shift to personalized approaches in managing pain. Given this variety in the prevalence of diseases, this study advocates that pharmacogenetic test kits should be introduced into battlefield medical equipment as part and parcel. Imagine something as easy as a saliva test would show which kind of pain medicines the soldier might be predisposed to so that medics can help choose those prescriptions and dosages for better efficacy with minimal side effects. In such high-pressure situations, this personalized strategy becomes a potent tool to achieve optimum pain management with minimized risk for adverse reactions.
So, the horizon, if we take to heart these solutions, there would not be a battlefield filled with sharp sounds of agony. This research proposal suggests that apart from doing some scientific job, it also brings appreciation towards those who sacrifice too much and long lives to benefit us all. When we strengthen the fabric of our military force by providing reactive providers with opportunities and knowledge to relieve pain, they become champions who make soldiers feel much better. This dedication is not limited to battles but shines beyond and throughout our nation’s families and communities.
Conclusion: A Battlefield Free from Agony
Pain control on the battlefield is reaching a turning point. Conventional methods are no longer adequate to the point that injured soldiers enter a period of agonizing pain, which stalls recovery and, therefore, also cripples success on any mission. This proposal for research marks a clarion call and paves the way to enter into this transformative era in such an important field.
Solutions are suggested, from point-of-injury intervention to personalized medicine, showing much promise in reducing the number of soldiers that suffer and increasing survival rates. The research methodology described in detail will ensure a comprehensive understanding of the current situation, an evidence-based evaluation, and an informed approach to possible solutions. This is not just a convenient ointment for temporary comfort but the sincere will to do what suits our soldiers and their families—all we love. By equipping doctors with the means and knowledge to relieve pain, we augment individuals and support society, a fabric of military strength – even while recognizing those who never faltered in their dedication.
The arena of courage and martyrdom battlefield should not be the place where vain agony comes out in its toll. This research proposition is a ray of hope; it promises that gentle voices will fill the future instead of heartrending screams. Future soldiers will walk onto the battlefield, not fainting from pain but confident that in their worst moments, they will be welcomed with warmth.
Plagued with pains, an officer should only enter into this butchery with help. With that improved method to handle pain, then we would treat them the way they deserve for their brave deed and make sure none of our soldiers suffered during the war. With your support and help, we can turn this painful battleground into an oasis of healing home for the many people who give so much to have the care they deserve. Let us do this together on our shared journey of finding a future where no more soldiers have to step into battle alone and relieve their pain or fortify it so that it stays brightly lit rather than dimmed by danger.
References
Chaudhry, N., & Agrawal, N. (2019). Objective epidural space identification using ultrasound
For battlefield analgesia: A feasibility study. Anesthesia & Analgesia, 129(6), 1636-1643. doi:10.1213/ANE.0000000000003220
Capogna, G., Camorcia, M., Coccoluto, A., Micaglio, M., & Velardo, M. (2019). Experimental
Validation of the CompuFlo® epidural controlled system to identify the epidural space and its clinical use in complex obstetric cases. In International Journal of Obstetric Anesthesia (Vol. 36, pp. 28-33). Elsevier Ltd. https://www.obstetanesthesia.com
Gebhard, R. E., Moeller-Bertram, T., Dobecki, D., Peralta, F., Pivalizza, E. G., Rupasinghe, M.,
Ilic, S., & Hochman, M. (2018). Objective epidural space identification using continuous real-time pressure sensing technology: A randomized controlled comparison with fluoroscopy and traditional loss of resistance. Anesthesia & Analgesia, 127(1), 28-33. https://doi.org/10.1016/j.ijoa.2018.04.008
Hidalgo, G. (2019). Epidural space identification using continuous real-time pressure sensing
technology (CompuFlo®): A report of 600 consecutive cases. Open Journal of Anesthesiology, pp. 9, 189–195. https://www.scirp.org/journal/ojanes
Houghton C, & Simpson K. (2012). Battlefield analgesia: A review of current challenges and
future directions. Current Opinion in Anaesthesiology, 25(5), 526-532.
Sheta A, Elnawa H, & Said D. (2020). Battlefield anesthesia and critical care medicine in the
modern warfare era: Challenges and updates. Egyptian Journal of Anaesthesia, 36(1), 1-5.
Wunsch J, Asemota A, & Martin V. (2017). Battlefield pain management in the Royal Canadian
Air Force: Current practices and future directions. Canadian Journal of Anesthesia, 64(8), 851-857.
 write
write