Safety in healthcare is an important issue needing sustained concentration and refining. Research estimates that 1 in 10 healthcare users have suffered from some form of harm, resulting in more than 3 million casualties each year (WHO, 2023). In poor to middle-income countries, the fatalities due to inadequate care rise to 4 out of every 100. One safety matter that remains weighty in medical surroundings is medication missteps, which may lead to severe aftermaths for patients. For the highest possible outcome in patient care, doctors, pharmacists, and patients must be mindful of the chance of fault. Taking the wrong medicaments can be deadly, and averting this dilemma is imperative to forestall unwarranted demise. This paper looks at medication errors in hospitals distinctly, examining their effects and postulating techniques for reform.
Medical Errors in Medical Facilities
A medical misstep is any avoidable occasion that could harm patients while the healthcare professional, patient, or patron controls the medicine. Clinical errors plunge across many mistakes, including medication punches, misdiagnoses, surgical fluctuations, and communication breakdowns. Drug errors are earmarked as a distinct area of concern in clinical treatment because of the towering risks to patient well-being and intricacy. A novel John Hopkins examination reveals that more than 250,000 people in the U.S. succumb yearly from medical slips (Jean-Pierre, 2022). Other accounts propose the stats to be as lofty as 440,000. The principal fields of issue that offer the chief hazard to the safety of the patients have their center on the management of antibiotics. The total cost of caring for sufferers with medication-tied mistakes goes beyond $40 billion each annum, with more than 7 million patients affected (Tariq et al., 2018). In addition to the pecuniary expenditure, patients experience psychological and physical suffering due to medication eccentricities.
A critical impact of medication gaffes is that they result in reduced patient satisfaction and a burgeoning lack of belief in the healthcare system. Intensive care units symbolize the most hazardous to patients regarding safety due to the vital nature of the diseases and the probably extreme repercussions of medication deviations. Rodziewicz and Hipskind (2020) state that medication errors are significantly responsible for patient mortality and morbidity rates, making it a perturbing issue for healthcare providers. Incorrect communication among healthcare providers, tiredness, inappropriate training, and taxing healthcare systems are some aspects that add to these misactions.
Causes of Medical Mistakes
Medication blunders can happen at distinctive phases of the medication deployment procedure, and a blend of system-connected factors, human errors, and communication issues can induce them. Deficient communication between healthcare providers, such as bleary handwriting on prescriptions, verbal miscommunication during handoffs, or misinterpreting orders, can lead to medication slips. Healthcare specialists, including nurses and pharmacists, may need to be correctly tutored in medication application techniques, operations, or the usage of advanced technology, thus resulting in mistaken amounts or management. Healthcare providers working for exhaustive hours or in high-stress environments have an increased propensity for drowsiness, damaging their evaluation and concentration and escalating the possibility of medication miscues. The most collective grounds for missteps comprise more communication concerning drug orders, indiscernible handwriting, and incorrect drug selection from a drop-down menu. Medication unevenness may arise from human blunders, but it regularly ensues from a substandard system that does not contain emergency detectors to identify mistakes. Errors take place when medication orders from prescriptions or hi-tech systems to medication management accounts bring about incorrect doses or medications being dispensed. Medication mistakes are most prevalent at the ordering or prescribing stage. Data shows that nurses and pharmacists recognize 30% to 70% of medication-ordering slips (Tariq et al., 2018). It is clear that medication jumps are an extensive dilemma, but the matters are usually preventable. Variegation in medication naming, labeling, packaging, and dosing units can confound healthcare providers and lead to missteps.
Strategies to Improvement
Patient education also plays an essential role. Apprised patients are improved and appareled to be advocates for their safety, ask solicits, and understand their therapy plans. Hospitals and healthcare providers must prioritize transparency, accountability, and indefinite advancement to guarantee patient safety and minimize medical mistakes in healthcare backgrounds. Carver et al. (2023) articulate that the first move in enhancing patient safety involves understanding the distinctive types of medical blunders and the healthcare processes that lead to medical goofs during healthcare administration. Hi-tech health record (EHR) system matters, and inadequate patient education also plays a substantial role in these jumps. Healthcare providers scan the medication and patient’s barcode before organization, permitting the system to scrutinize the medication with the stated dosage, route, and time.
Nurses need to implement established norms, trimming variations in techniques that could result in missteps. Potent communication among healthcare teams is central to preventing slips. Training schemes enhance communication abilities, commending crystalline and summarized advice shifts amidst squad associates and diminishing the peril of misinterpretation. Effective communication among healthcare teams is critical to avert errors. Training schemes concentrate on improving communication aptitudes, commending clear and succinct data exchange amongst team components, and reducing the peril of misinterpretation. Standardized medicament storage, labeling, and packaging in pharmacies lessen the peril of dispensing mistakes—adequate labeling reports key details, counting expiration dates and storage requirements, and ensures medication stability. Through the triumphant utilization of numerous Lean Six Sigma tools, the execution of Lean Six Sigma brought down monthly dispense errors from 29 circumstances to 6 occurrences over 14,000 total inpatients (Trakulsunti et al., 2022). Furthermore, encouraging a civilization of safety, encouraging open communication, and performing perpetual training for healthcare professionals can amplify these pingers.
Conclusion
In conclusion, tending to medication errors calls for a coordinated attempt that brings together innovative technology, progressing education, and patterned practices. By adopting these approaches, healthcare organizations can enhance their safeguard against medication-interrelated problems, safeguarding their patients’ lives and welfare. As we go forward, unswerving attention, variation to novel technologies, and a steady commitment to education will be indispensable in continuously pursuing enhanced healthcare safety.
References
Carver, N., Gupta, V., & Hipskind, J. E. (2023). Medical Errors. In StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK430763/
Jean-Pierre, P. (2022). Medical error and vulnerable communities. BUL Rev., 102, 327. https://heinonline.org/HOL/LandingPage?handle=hein.journals/bulr102&div=9&id=&page=
Rodziewicz, T. L., & Hipskind, J. E. (2020). Medical error prevention. StatPearls. Treasure Island (FL): StatPearls Publishing. https://heinonline.org/HOL/LandingPage?handle=hein.journals/injlolw11&div=637&id=&page=
Tariq, R. A., Vashisht, R., Sinha, A., & Scherbak, Y. (2018). Medication dispensing errors and prevention. https://europepmc.org/article/NBK/nbk519065
Trakulsunti, Y., Antony, J., Edgeman, R., Cudney, B., Dempsey, M., & Brennan, A. (2022). Reducing pharmacy medication errors using Lean Six Sigma: A Thai hospital case study. Total Quality Management & Business Excellence, 33(5-6), 664-682. https://www.tandfonline.com/doi/abs/10.1080/14783363.2021.1885292
World Health Organization (WHO).(2023, September 11). Patient Safety. https://www.who.int/news-room/fact-sheets/detail/patient-safety
APPENDIX
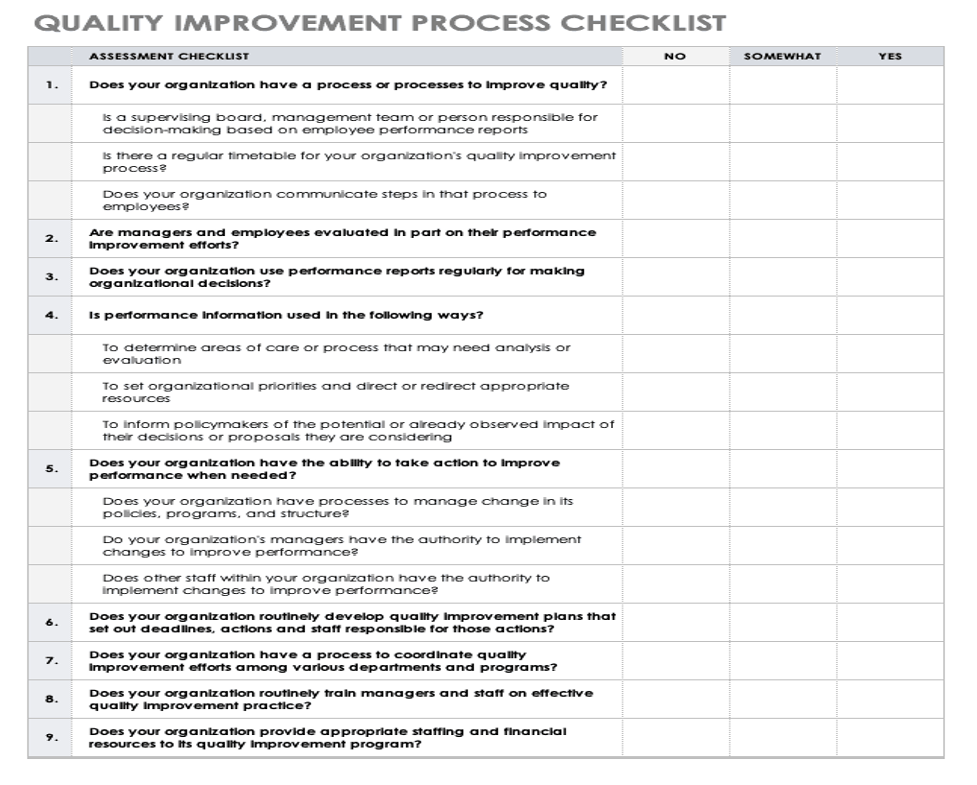
| Checklist For Quality And Performance Improvement | |
| 1. Implement Barcode Medication Administration (BCMA) Systems
o Ensure all pharmaceuticals have barcodes attached for precise scanning. o Educate medical professionals on the correct utilization of BCMA arrangements. o Continually upgrade BCMA programming to tackle potential glitches and enhance capability.
|
|
| 2. Organize routine instruction on medication safety procedures
o Foster communication training to enable superior information exchange between staff members. o Consider offering refresher courses to make sure comprehension and abilities are updated. o Standardize prescription drug protocols.
|
|
| 3. Establish formalized guidelines for prearranging, recording, dispensing, and managing drugs.
o Verify that all medical practitioners adhere to structured steps to avoid puzzlement. o Continually reevaluate and upgrade protocols based on cutting-edge discoveries and adeptness. o Augment Patient Knowledge
|
|
| 4. Patient education materials about drugs.
o Meet with patients to describe their medications, dosage, and probable complications. o Stimulate patients to inquire and resolve any doubts about their medications. o Organize Periodic Medication Safety Checks
|
|
| 5. Periodically audit medication safety protocols to determine compliance
o Identify shortcomings based on audit reports and implement remedies. o Spread the word about audit results and rectification plans among all personnel to create a responsible environment. o Promote the habit of registering near misses and errors. |
|
 write
write