Introduction to the Proposed Problem and its Significance
Sepsis is a life-threatening health condition that needs early detection and prompt patient intervention to avoid any adverse outcomes as it affects the systems of the body, which enhance response to infections (Evans et al., 2021). It occurs when the infection-fighting process turns on the human body causing the organs to work poorly, and may progress to a septic shock whenever there is a late diagnosis. Some of the symptoms associated with the disease involve changes in the patient’s mental status, fast yet shallow breathing, lightheadedness, shivers, and specific symptoms related to a certain type of infection, such as worsening cough due to pneumonia. In the UK, the disease has an incidence of 360 cases per 100,000 individuals annually and a mortality rate of around 20%. The patients who present early have a lower probability of dying from the condition than those who present late. There is also a greater likelihood of saving life since 1 in every 2800 to 1 in every 5000 awareness episodes can save the patients’ lives (Ni et al., 2019). This capstone project aims to develop a new policy that will allow for earlier detection of Sepsis and enhance its management within the intensive care units (ICU). The developed policy will focus on enhancing patient outcomes through early detection, lowering the mortality rates, and optimizing the delivery of healthcare services among patients at a greater risk of Sepsis or those with Sepsis. The new policy will also ensure the safety of the patients and lower the degree of complications resulting from Sepsis.
PICOT
The PICOT, in this case, does the implementation of a new policy for early sepsis detection and management in comparison to the pre-existing standards of practice enhance the patient outcomes, lower the mortality rates and ensure optimization in delivery of care among patients admitted in ICU for Sepsis within a period of six months. From this PICOT, the population is the patients who have been admitted to the ICU as a result of Sepsis; the intervention is the implementation of a new policy to allow for early sepsis detection and management; the aspect of comparison is the pre-existing standards of practice, the outcome involves improved patient outcomes, lower mortality rates and optimized delivery of healthcare services among the patients diagnosed with Sepsis. The timeline for this is six months.
Vulnerable Population
For this project, the vulnerable population involves all the patients who have been admitted to an ICU because of Sepsis, and those who are at a greater risk of being diagnosed with Sepsis since they have a compromised immune system are at a greater risk of rapid clinical deterioration and being diagnosed with other health outcomes.
Effects of the Social Determinants of Health
Even though the social determinants of health influence the development of Sepsis indirectly, the primary focus of this project is the clinical aspects that enhance early detection and management of the condition instead of social factors.
Evidence-Based Interventions
The new policy will be developed based on evidence-based interventions that will inform the policy design, and this will be identified through a review of the existing literature, identified peer-reviewed articles, and other academic journals published within the last five years. Some interventions involve using standardized protocols to enhance sepsis screening, a detailed criterion for early detection, the appropriate labs and imaging investigation, an algorithm of diagnosis, and timely initiation of the interventions related to the health condition.
Proposal
In this case, the proposed intervention involves developing new policies that allow for the early detection of Sepsis and its management among patients in the ICU. This new policy is anticipated to offer clear protocols and guidelines for the assessment, identification, and management of Sepsis among patients who are in the ICU. The elements of the policy will involve a standardized sepsis screening mechanism for identifying patients who are at greater risk, the criteria for early recognition of septic shock and Sepsis among patients, the algorithms for accurate and timely diagnosis, and the recommended labs and imaging investigations. Furthermore, it will incorporate the protocols for the administration of the right antibiotics and fluids as required by the patients, implementation of the interventions of Sepsis, and monitoring and evaluation of the outcomes of sepsis management. This new policy will address the gaps in the present-day treatment approaches involving antibiotics (Martínez et al., 2020). Development of this policy will involve collaboration between various healthcare providers, including the ICU physicians, pharmacists, lab staff, nurses, and pharmacists, among others, and that means they will have to implement a highly effective communication approach for successful policy development and implementation.
Feasibility for Nurses in the Advanced Roles
The advanced practice nurse can play a vital leadership role in implementing and developing the new sepsis policy through collaboration with other healthcare providers. He or She can be at the forefront of ensuring accuracy in a literature review by guiding the other team members, developing the appropriate policy content, and ensuring that the policies are aligned with the existing evidence-based practices (Moran et al., 2023). The nurse may also offer the necessary training and education to the ICU staff, monitor compliance with the policies, and evaluate its overall impact on patient outcomes.
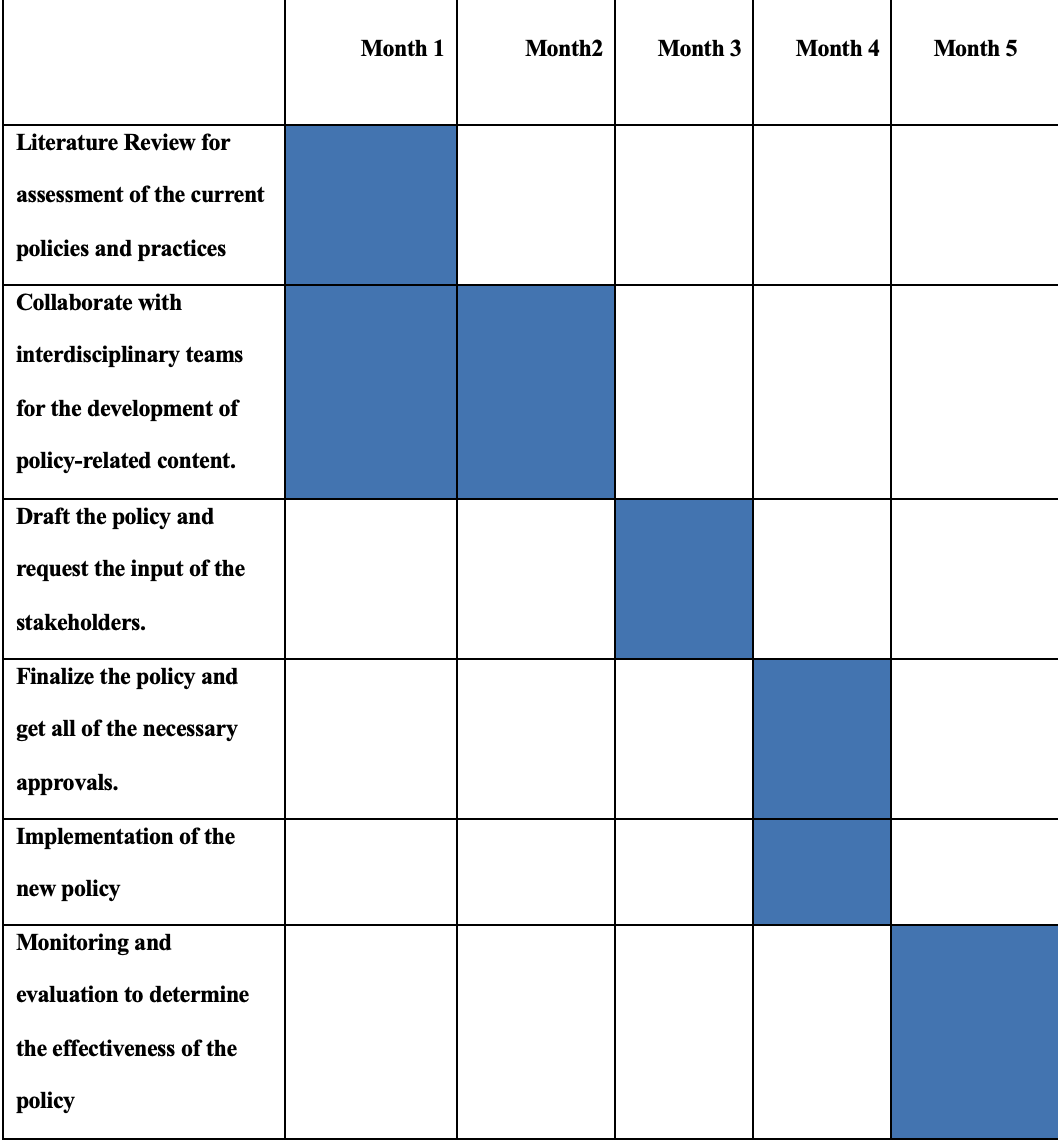
Timeline of Policy Development
Theoretical Framework
This project will adopt the Promoting Action on Research Implementation in Health Services (PARHIS) framework as this framework greatly emphasizes the interactions between the available evidence, facilitation, and context in implementing evidence-based practices. Applying this framework will allow for developing a new sepsis policy tailored to ICU patients (Dryden-Palmer et al., 2020). the policy will also be supported by various effective facilitation strategies and guide the whole policy development, implementation, and evaluation process in the long run. Through the development of a new policy seeking to ensure early detection of Sepsis and its management within the ICU, this project will enhance patient outcomes, lower mortality rates, and optimize the delivery of healthcare services among patients who have Sepsis. This proposed policy is feasible and realistic as it falls within the semester’s dates, allowing for a meaningful exchange in the clinical environment.
References
Dryden-Palmer, K. D., Parshuram, C. S., & Berta, W. B. (2020). Context, complexity, and process in implementing evidence-based innovation: a realist informed review. BMC health services research, 20(1), 1–15. https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-020-4935-y
Evans, L., Rhodes, A., Alhazzani, W., Antonelli, M., Coopersmith, C. M., French, C., … & Levy, M. (2021). Surviving sepsis campaign: international guidelines for managing Sepsis and septic shock 2021. Intensive care medicine, 47(11), 1181–1247. https://doi.org/10.1007/s00134-021-06506-y
Martínez, M. L., Plata-Menchaca, E. P., Ruiz-Rodríguez, J. C., & Ferrer, R. (2020). An approach to antibiotic treatment in patients with Sepsis. Journal of thoracic disease, 12(3), 1007. doi: 10.21037/jtd.2020.01.47
Moran, K. J., Burson, R., & Conrad, D. (2023). The Doctor of nursing practice project: A Framework for success. Jones & Bartlett Learning. https://books.google.co.ke/books?hl=en&lr=&id=0f-pEAAAQBAJ&oi=fnd&pg=PP1&dq=roles+of+advanced+nursing+practice&ots=beKIvxShBL&sig=KyXmgY5sh0sjOyVOjc71miFzmDY&redir_esc=y#v=onepage&q=roles%20of%20advanced%20nursing%20practice&f=false
Ni, J., Wang, H., Li, Y., Shu, Y., & Liu, Y. (2019). Neutrophil to lymphocyte ratio (NLR) as a prognostic marker for in-hospital mortality of patients with Sepsis: A secondary analysis based on a single-center, retrospective, cohort study. Medicine, 98(46). doi: 10.1097/MD.0000000000018029
 write
write