Introduction
Diabetes is one of the most common global health challenge. Diabetes is a non-contagious disease characterized by impaired insulin production or the body’s inability to respond to insulin. Diabetes is becoming a global health challenge as its prevalence and incidence rise (Bandy et al., 2020). According to research conducted by Saeedi et al., the prevalence of diabetes at 9.3% in 2019 was projected to rise to about 10% by the year 2045. United kingdom has the highest burden of patients living with diabetes. Type two diabetes Mellitus is the most typical type of diabetes, attributing to 90% of people affected by diabetes globally. In the United Kingdom, diabetes is managed using a multidisciplinary approach involving physicians, nurses, and other healthcare professionals such as dieticians and podiatrists. Compared to the individual patient-provider care model, an interdisciplinary approach is thought to improve diabetes care quality (Saed et al., 2019). In this article, I will explore the prevention of illness and health promotion of diabetes. I will also discuss the epidemiology of diabetes, the assessment of diabetes on the population, the model to be used in health promotion, the goals of preventing illness, interventions, and evaluation of the interventions in health promotion. The interventions will involve the role of various groups in health promotion and prevention of diabetes as a significant health challenge.
Background
Diabetes is a disorder of metabolism clinically characterized by episodes of elevated blood glucose in the serum. Anomalies contribute to high serum glucose levels in insulin secretion or impaired insulin function, resulting in abnormal fat and carbohydrate and protein metabolism (Care, 2018). The most commonly affected organs include the eyes, which results in diabetic retinopathy neuropathy in the central nervous synthesis. Nephropathy in the kidneys results from damage of the microvascular of the nephrons (Care, 2018). The heart is also affected, and cardiovascular complications cause diabetes-associated mortality and morbidity (Egan &Dinneen, 2019).
Various types of diabetes affect the population; diabetes type 1, type 2, and gestational diabetes (Whicher et al., 2019). Type 1 diabetes is characterized by autoimmune destruction of the beta cells in the pancreas that secret insulin by autoantibodies. These diabetes account for only 5-10 % of all diabetic cases (Kahlyi & Hansen, 2016). In type 2 diabetes, the insulin production is average, but significant insulin resistance and insulin insufficiency (Care, 2018). Hyperinsulinemia prevents hyperglycemia (Galicia- Garcia et al., 20200. Diabetes type 2 is the most common and accounts for 90-95% of all cases.
Gestational diabetes occurs in pregnancy, especially in the second or third trimester. Both fasting and post-prandial blood glucose levels usually are lower than usual during early pregnancy. Still, blood glucose levels rise during the third trimester, and when this blood glucose level exceeds diabetic levels (McIntyre et al., 2019).
Epidemiology of diabetes in the United Kingdom
In the United Kingdom, about a 4.7 million people are living with diabetes, of whom 90% have diabetes type 2, 8% have type 1 diabetes, and the other type of diabetes account for 2 %. The number of people living with diabetes has been steadily on the rise for the past two centuries, and it is projected that the number of diabetic patients will be at 5.5 million by the year 2030 (Forouhi & Wareham, 2019). The number of people living with diabetes accounts for 7% of the population in the United Kingdom. In the United Kingdom, about 12.3 million people are at risk of developing type 2 diabetes. South Asian and African- the Caribbean having likely to develop diabetes four times compared to the whites.
Some of the risk factors include; overweight and obesity among the population, lack of exercise and physical activity, poor dietary habits, family history of diabetes, and inequalities in accessing healthcare services for the South Asian and African-Caribbean (Forouhi & Wareham, 2019). Preexisting comorbidities such as hypertension and chronic kidney disease also increase the risk of developing diabetes in the United Kingdom. About 40000 children aged between 10- 14 years are living with diabetes. And 90% of this is type 1 diabetes.
Diabetes is characterized by polyuria, polydipsia, and polyphagia. The patients can also present with weight loss, poor skin turgor due to dehydration, fruity odour due to ketosis, blurred vision, and acanthosis nigricans due to insulin resistance. Diabetic patients may present with numbness, neuropathic pain, and frequent infections of the yeasts (Audit, 2017).
Assessment
Diabetes is assessed and evaluated using various methods. One of the most significant assessments in diabetes is comprehensive history taken from the patient. This includes glucose levels for a period of time measured by fasting glucose levels more than 126mg/dl, random blood glucose of more than 200mg/dl, glycated haemoglobin greater than 6.5%, and antibodies such as glutamic decarboxylase and insulin (Care, 2018)).
HbA1c and fasting blood glucose levels are very useful in detecting diabetic episodes, especially type 2 diabetes. An oral glucose tolerance test evaluates the fasting blood glucose and serum glucose levels. According to Egan & Dinneem 2019, type 2 diabetes is diagnosed when the glycated haemoglobin is more than 6.5%, fasting blood glucose levels of more than 126mg/dl with 8 hours fasting, a random blood glucose level of more than 11.1 mmol, and an oral glucose tolerance test of 180, 155 and 145mg/dl for fasting within one, two and three hours. In type one diabetes, autoantibodies such as glutamic decarboxylase (Care, 2018).
A fasting blood glucose challenge is done for gestational diabetes, especially in 24-28 weeks of gestation. If the blood glucose levels are above 140mg/dl, the confirmatory test is done at an interval of three hours fasting. If the test shows atleast one abnormal level of greater than; 180, 155, and 140mg/dl, it is confirmed (Bandy et al., 2020). Other tests are done to ensure the stage and extent of the disease, such as serum lipid profile, urine albumin test, and thyroid-stimulating hormones.
Health Promotion Model
In healthcare, various health promotion models are used to ensure and support the prevention of illness and promotion of health. The health promotion models are helpful in healthcare as they are used in planning the programs to help understand and explain health behaviour to aid in identifying and developing goals and interventions. It’s essential to consider various approaches when choosing a theory or model to guide health promotion or disease prevention initiatives, including the specific health problem being addressed, the population(s) served, and the circumstances in which the program is being implemented (Green et al., 2020). In health promotion, I will employ the health belief model to help address the challenge of diabetes in the United Kingdom.
Figure 1: Diabetes prevention behaviour conceptual framework
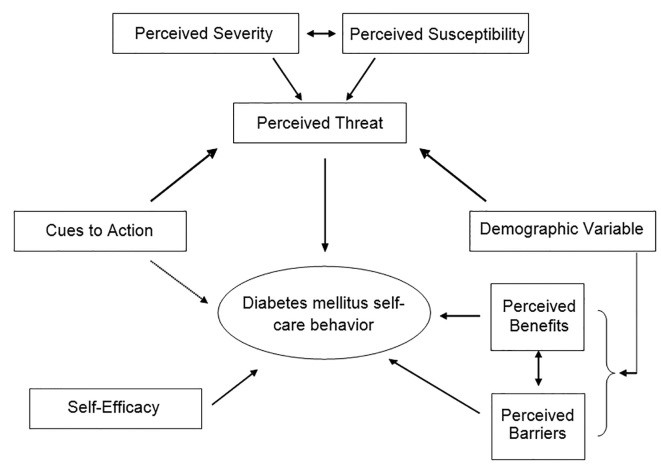
The health belief model is a model used in health promotion to explain and predict the behaviour of individuals (Green et al., 2020). Using the model to address diabetes as a global challenge, the model defines various approaches used while promoting health, such as the perceived threat of diabetes, patients’ belief on the consequences of the behaviour, perceived benefits, patients barriers to actions on diabetes prevention, cues of actions and patients ability to succeed in promotion of health and diabetes prevention (Sahbibi et al., 2017). The health belief model is very significant in health promotion related to diabetes. It mainly focuses on preventing diabetes and adopting behaviours that will enable th population to avoid diabetes and promote a healthy population.
Health Promotion Goals
While promoting health in diabetes and prevention of illness, my goals include reducing the incidence of type 2 diabetes among the population. My aim is to ensure that the incidence of new diagnoses of diabetes cases is reduced in a community. This will be enhanced by providing that the community adapt to healthy lifestyles and eradicate the lousy lifestyle habit such as lack of exercise, sedentary life, and inactivity, poor dietary habits. My second goal in a health promotion program includes the reduction of incidence of complications associated with diabetes, such as diabetic retinopathy, nephropathy, neuropathy, cardiovascular diseases, and foot ulcers (Banday et al., 2020). Many patients diagnosed with diabetes die from diabetic complications encouraging early mortality and morbidity. This is evidenced by research that showed about 70000 to 90000 people in the United Kingdom have a foot ulcer, and diabetes contributes to 175 amputations every week. The study showed that diabetic patients are at a higher risk of experiencing amputation than healthy people without diabetes (Graz et al., 2018). Diabetes, also in the United Kingdom, is the leading cause of preventable blindness, which accounts for 5% of all sight loss. About 1700 people have diabetes-related eye problems (Denniston et al., 2019).
The other health promotion goal in diabetes prevention and promotion is to reduce the health inequalities associated with diabetes type 2 and enhance behavioural intervention in patients to encourage the population to maintain a healthy weight and be more active. This will be achieved by achieving a healthy weight, dietary recommendations, and chief medical officers’ physical activity recommendations. In the United kingdom, overweight and obesity are responsible for 80-85% of individual risk of developing diabetes. In Europe and Scotland, a study done by Ng M et al. showed only 67% of men and 55% of women met recommended physical activities such as swimming and cycling (Inoue et al., 2018).
Interventions
In order to realize our health promotion goals, various actions and strategies must be put in place to ensure the realization of health promotion goals. Healthcare must work as a multidisciplinary team to enhance the completion of goals. In the United Kingdom, the National Health Service Diabetes Prevention Program has been established to provide evidence-based behavioural interventions to populations vulnerable of developing diabetes. To lower the number of new cases of diabetes in the population, interventions include educating the public and increasing awareness of diabetes (McGough et al., 2019). Educating the patients on ways to prevent diabetes includes adopting healthy lifestyle habits such as exercising daily, dietary intake and caloric intake, maintaining a healthy weight, and avoiding alcohol consumption. For instance, in United Nations, the government can enhance the National Health Service Diabetes Prevention Program through the clinical commissioning groups to enhance the uptake of the program. This will encourage community involvement in the prevention of diabetes, identify the population vulnerable of developing diabetes and promote the creation of awareness and lifestyle interventions. Through community involvement, NICE guidelines can be enhanced as they provide ways of avoiding type 2 diabetes in high-risk adult populations and communities. Its goal is to encourage a balanced diet and physical activity in communities and populations, as well as give recommendations for service adaptations for persons in ethnic communities and other groups at high risk of type 2 diabetes..
To reduce the mortality and morbidity associated with diabetes complications, interventions include increasing the awareness of the importance of screening diabetes in the population. Screening of diabetes enables early identification of diabetes. Early identification enhances controlled management of diabetes. It also helps in avoiding cases of undiagnosed diabetes in the population. Regular check-up of diabetic patients in eye clinics, neuro clinics, and kidney reduces complications arising from diabetes. Incorporating technology in diabetic management can reduce the mortalities associated with diabetes. The use of telemedicine enables the monitoring of diabetes patients in remote areas. Telemedicine is critical in lowering mortalities and incidences of diabetes as it allows in self-management of diabetes such as self-monitoring of blood glucose levels, providing diabetic education, and drug adherence, enabling online consultation, which improves care and management of the disease, thus, reducing complications (Lee & Lee, 2018).
To reduce health inequalities associated with diabetes patients in the United Kingdom, especially the South Asian and African-Caribbean, interventions such as enhancing equality in providing care to the population will reduce the disparities. In the United Kingdom, according to Farouhi and Wareham, 2019 there are inequalities in accessing healthcare services for the South Asian and African-Caribbean. South Asian and African-Caribbean persons are two to four times more likely than white Europeans to have type 2 diabetes(Farouhi & Wareham, 2019). Deprivation of quality care of patients impacts the incidence and prevalence of diabetes. Enhancing quality care to socially disadvantaged people is critical in counteracting the detrimental effects of diabetes.
The National Health Service has also put long-term strategies to reduce and prevent diabetes in the United Kingdom. This includes population-level interventions. This is significant in addressing obesity reducing the risk of developing diabetes type 2. Population-level involves multidisciplinary collaboration between various community, local and voluntary sectors in implementing population-level approaches. The NICE guidance also provides strategies for helping the population adapt to new lifestyles that promote behaviour change. This includes achieving and maintaining a healthy weight to reduce risk factors of obesity and overweight associated with diabetes. This includes adopting a low-fat diet, reducing caloric fat intake, taking more starchy food such as potatoes, bread and rice, eating a fibre-rich diet, minimizing alcohol consumption, and engaging in swimming and cycling aerobics routine activities such as climbing stairs (Whicher et al., 2019).
They are increasing awareness in the community, especially in the minority groups, to increase access by using local media platforms to develop communication strategies inclusive of literacy levels. For instance, the use of pictorials. To enhance the prevention strategies of diabetes, identifying and addressing barriers to access such as improving affordability and subsidizing funds will enhance prevention strategies. Encourage local, regional, and national monitoring of diabetes and other non-communicable illnesses risk factors. Encourage the tracking of type 2 diabetes and different non-communicable disease incidence rates by age. Encourage all new policies to be evaluated for their potential health impact on the primary risk factors for type 2 diabetes and other non-communicable illnesses by local and national decision-makers. Ascertain that they are in favour of any national preventative approach (White, 2016).
Evaluation
Evaluation of diabetic prevention strategies is critical in determining the success of interventions employed and assessing if the goals have been achieved. The measures to identify interventions’ success include evaluating the patient satisfaction levels. Were the customers satisfied with the care delivered to them? This is helpful, especially to the marginalized and minority groups in Europe. Reducing the healthcare inequalities such as limited access to care can be evaluated by assessing the level of patient satisfaction to care given, resources available, and barriers that are in place that prevents them from accessing quality care (Stokes et al., 2019).
To evaluate the success of interventions on reducing comorbidity and mortality associated with diabetes complications, checking patient readmission and admission can be helpful. Were the interventions on close monitoring of patients using telemedicine effective? Did the healthcare reach out to the patients in a remote area? Was there a provision of awareness and education given to the patients? To understand this, patient readmission to the hospital due to diabetes complications should be reduced. Checking the national data on mortalities associated with diabetes complications can help determine the success of the interventions. Reduction of emergency services related to diabetes complications also is a crucial indicator of the success of the interventions. As a result of the interventions, there should be an overall reduction in diabetes complication-related deaths.
Increasing the diabetes screening program is another indicator of the success of the interventions. The National Health service should utilize its outreach program by enhancing regular screening of diabetes. Early screening of diabetes enables detecting the disease at early stages, prevents the development of complications, and improves the patient’s overall outcomes and prognosis. This can be enhanced by utilizing the National Health service Diabetes Prevention Program through local authorities and Clinical commissioning groups (Milne, 2018). This can also be used by reducing the number of people living with undiagnosed diabetes. This indicates success in the outreach program of diabetes screening.
Evaluating the success of the interventions can also be noted by checking on the adoption of healthy lifestyle habits such as alcohol consumption, caloric intake, sugar reduction, achieving a healthy weight, and adoption of chief medical officer recommendations (Valabhir et al., 2020). After the interventions, the percentage of obese and overweight patients should reduce from 68% in men and 59% in women to a lesser percentage in the United Kingdom. The statistics on the population that meets recommended physical activities levels in the United Kingdom and Scotland should increase from 67% and 55% in men and women, respectively. This will be indicated by increased cycling, swimming, and walking activities.
The National Health Service Diabetes Prevention program roll-out began in June 2016. The NHS Diabetes Prevention Programme (DPP) was launched, and it is now in its third year available all around the country. The DPP registered 103 000 people between 2017 and 2018, and the
According to the program model, 18 000 cases of type 2 diabetes will be diagnosed by the fifth year of the Programme. The diabetes incidence among the 5-year cohort will have been avoided or postponed. This is a crucial indicator of the success of the interventions. The program was first rolled out in June 2016, with the first wave of 27 districts involving 26 million people, making up to 20,000 spaces available. In April 2017, the Programme expanded to 13 new sustainability and transformation partnerships, covering 75 percent of England’s population. The program was developed for all remaining clinical commissioning groups and local authorities in England that had not previously been enrolled, achieving full coverage in April 2018, with referrals expected to begin in July 2018. The programe has been able to refer more than 185000 patients (Penn et al., 2018).
Recommendations
Community outreach and screening should be enhanced to effectively prevent diabetes and promote a healthy population, especially minorities and vulnerable groups. This can be achieved by incorporating telehealth in reaching more people. The use of telemedicine is cost-effective for patients. They are increasing awareness through mass media and the use of community and local authorities to improve patient education. Multidisciplinary collaboration with various stakeholders such as private and voluntary sectors will encourage the prevention of diabetes and health promotion.
Conclusion
Every year, 100,000 people in the UK are diagnosed with diabetes, but in 2009, that number jumped to 150,000. Many others are completely unaware that they have the disease. It can cause long-term vision problems, kidney disease, foot ulcers, and heart disease. Patients with diabetes type 2 have a life expectancy of five to seven years less compared to ordinary people. This has attributed to the increased cost of healthcare services and has called for action to prevent and reduce diabetes prevalence and incidence. Strategies to promote health include reducing the new incidence of diabetes in the United Kingdom, reducing diabetes-related complications, reducing healthcare inequalities related to diabetes, and enhancing behavioural modifications such as adopting a healthy diet with high fibre intake, low-fat diet, reducing caloric intake, engaging in physical activities such as cycling, swimming, and reducing weight and maintaining a healthy weight to reduce obese. The incorporation of telehealth helps enhance screening and promote health. Therefore enhancing interventions such as patient education, increased screening, reducing healthcare inequalities, provision of quality care for all enhance diabetes health promotion.
References
Audit, D., 2017. NPDA.
Banday, M.Z., Sameer, A.S. and Nissar, S., 2020. Pathophysiology of diabetes: An overview. Avicenna Journal of Medicine, 10(04), pp.174-188.
Care, D., 2018. Medical Care in Diabetes 2018. Diabetes Care, 41(1), pp.S105-S118.
Denniston, A.K., Lee, A.Y., Lee, C.S., Crabb, D.P., Bailey, C., Lip, P.L., Taylor, P., Pikoula, M., Cook, E., Akerele, T. and Antcliff, R., 2019. United Kingdom Diabetic Retinopathy Electronic Medical Record (UK DR EMR) Users Group: report 4, real-world data on the impact of deprivation on the presentation of diabetic eye disease at hospital services. British Journal of Ophthalmology, 103(6), 837-843.
Egan, A.M. and Dinneen, S.F., 2019. What is diabetes?. Medicine, 47(1), pp.1-4.
Forouhi, N.G. and Wareham, N.J., 2019. Epidemiology of diabetes. Medicine, 47(1), pp.22-27.
Galicia-Garcia, U., Benito-Vicente, A., Jebari, S., Larrea-Sebal, A., Siddiqi, H., Uribe, K.B., Ostolaza, H. and Martín, C., 2020. Pathophysiology of type 2 diabetes mellitus. International journal of molecular sciences, 21(17), p.6275.
Graz, H., D’Souza, V.K., Alderson, D.E. and Graz, M., 2018. Diabetes-related amputations create considerable public health burden in the UK. Diabetes research and clinical practice, 135, pp.158-165.
Green, E.C., Murphy, E.M. and Gryboski, K., 2020. The health belief model. The Wiley encyclopedia of health psychology, pp.211-214.
Hod, M., Jovanovic, L.G., Di Renzo, G.C., De Leiva, A. and Langer, O. eds., 2018. Textbook of diabetes and pregnancy.
Inoue, Y., Qin, B., Poti, J., Sokol, R., and Gordon-Larsen, P., 2018. Epidemiology of obesity in adults: latest trends. Current obesity reports, 7(4), pp.276-288.
Kahaly, G.J., and Hansen, M.P., 2016. Type 1 diabetes-associated autoimmunity. Autoimmunity Reviews, 15(7), pp.644-648.
Lee, J.Y. and Lee, S.W.H., 2018. Telemedicine cost-effectiveness for diabetes management: a systematic review. Diabetes technology & therapeutics, 20(7), pp.492-500.
McGough, B., Murray, E., Brownlee, L., Barron, E., Smith, J. and Valabhji, J., 2019. The healthier you: NHS Diabetes Prevention Programme: digital modes of delivery engage younger people. Diabetic Medicine, 36(11), p.1510.
McIntyre, H.D., Catalano, P., Zhang, C., Desoye, G., Mathiesen, E.R., and Damm, P., 2019. Gestational diabetes mellitus. Nature reviews Disease primers, 5(1), pp.1-19.
Milne, E., 2018. The transfer of public health to local authorities suggests alternatives are possible. BMJ: British Medical Journal (Online), 361.
National Institute of Health and Care Excellence. Diabetic Foot Care in England: An Economic Study; 2017. Available at https://www.evidence.nhs.uk/document?id=1915227&returnUrl=Search%3Fq%3DDi abetic%2BAmputation&q=Diabetic+Amputation Last accessed ? ?? 201?.
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C et al. Global prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013
Penn, L., Rodrigues, A., Haste, A., Marques, M.M., Budig, K., Sainsbury, K., Bell, R., Araújo-Soares, V., White, M., Summerbell, C. and Goyder, E., 2018. NHS Diabetes Prevention Programme in England: formative evaluation of the Programme in early phase implementation. BMJ Open, 8(2), p.e019467.
Saeedi, P., Petersohn, I., Salpea, P., Malanda, B., Karuranga, S., Unwin, N., Colagiuri, S., Guariguata, L., Motala, A.A., Ogurtsova, K. and Shaw, J.E., 2019. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas. Diabetes research and clinical practice, 157, p.107843.
Shabibi, P., Zavareh, M.S.A., Sayehmiri, K., Qorbani, M., Safari, O., Rastegarimehr, B. and Mansourian, M., 2017. Effect of educational intervention based on the Health Belief Model on promoting self-care behaviors of type-2 diabetes patients. Electronic physician, 9(12), p.5960.
Stokes, J., Gellatly, J., Bower, P., Meacock, R., Cotterill, S., Sutton, M. and Wilson, P., 2019. Implementing a national diabetes prevention programme in England: lessons learned. BMC health services research, 19(1), pp.1-12.
Valabhji, J., Barron, E., Bradley, D., Bakhai, C., Fagg, J., O’Neill, S., Young, B., Wareham, N., Khunti, K., Jebb, S. and Smith, J., 2020. Early outcomes from the English National health service diabetes prevention programme. Diabetes Care, 43(1), pp.152-160.
Walsh, J.W., Hoffstad, O.J., Sullivan, M.O. and Margolis, D.J., 2016. Association of diabetic foot ulcer and death in a population‐based cohort from the United Kingdom. Diabetic Medicine, 33(11), pp.1493-1498.
Whicher, C.A., O’Neill, S. and Holt, R.G., 2020. Diabetes in the UK: 2019. Diabetic Medicine, 37(2), pp.242-247.
White, M., 2016. Population approaches to prevention of type 2 diabetes. PLoS medicine, 13(7), p.e1002080.
 write
write