Significance of the Study
The importance of studies researching Vasoplegic syndrome in post-cardiac arrest patients is not debatable. This condition is a mainstream complication after cardiac surgery that affects numerous patients. Vasoplegia leads to high vasodilation levels, hypotension, and inadequate tissue perfusion. These outcomes affect the patients adversely, affecting their quality of life. The patients also stand a higher risk of increased morbidity, mortality, and prolonged hospital stays, with a significantly high combination of challenges in managing Vasoplegia and its consequences. These challenges result from the uniqueness of the conditions, such as their unresponsiveness to conventional treatment, such as fluids and vasopressors. Moreover, a poor understanding of the condition can facilitate maltreatment, leading to refractory hypotension. As a result, medical professionals would be required to administer higher vasopressor doses whose impacts would be undesirable, noting the condition’s ineffectiveness with conventional treatments. In these regards, the condition challenges post-operative care, necessitating research to explore intervention approaches.
This study will help determine effective preventive and interventional measures to improve the outcomes of Vasoplegic syndrome patients. The data collected will facilitate an objective research basis for determining the best ways to improve the patient’s quality of life. Implementing improved interventions to manage Vasoplegia will also reduce hospital readmissions and prevent post-operative complications. This outcome will also reduce the possibility of nosocomial infections, improving long-term patients’ health (Nash, 2021). Besides, evidence-based research will facilitate the implementation of effective strategies that promotes efficiency and resource allocation of healthcare systems. Notably, Kram et al. (2022) and Maurin et al. (2022) demonstrate that methylene blue effectively improves Vasoplegia in adults’ cardiothoracic surgery patients, requiring the identification of the best administration and other intervention approaches. Kram et al. (2022) also demonstrated that methylene blue offers dose-dependent responses, making it a viable therapeutic option. The cohort study by Maurin et al. (2022) further showed that methylene blue positively affected post-operative microcirculatory alterations, supporting its interventional importance. As such, this study will reveal effective ways that can be used to promote patient care by improving Vasoplegic syndrome symptoms.
Theoretical Framework
The theoretical framework serves a crucial purpose in identifying key concepts and establishing interrelationships among them to determine a stable foundation for incorporating the “Prevention as Intervention” theory when finding ways to implement the application of methylene blue for post-cardiac surgery Vasoplegia prevention. This theoretical framework uses the Neuman Systems Model, which August-Brady (2000) used to contextualize patients, viewing them as dynamic and interactive systems that set certain boundaries and internal lines of defence to maintain stability. This theory’s relevance in nursing practice has been increasing, and its application in post-cardiac surgery care informs the necessary post-operative care measures. By treating patients and associated stakeholders as dynamic and interactive systems, nurses establish frameworks that consider the interplay between patients’ physiological, psychological, and environmental factors. In this respect, this Neuman Systems model helps nurses account for patients’ health journey’s physical, mental, and environmental dimensions. This way, nurses can implement holistic intervention measures to help Vasoplegic syndrome patients.
The “Prevention as Intervention” theory is a middle-range theory whose application in Vasoplegic syndrome patient care is significant. August-Brady (2000) explains that the theory is derived from the Neuman System Model and focuses on the proactive measures that help maintain a patient’s stability by improving desirable outcomes and preventing adverse effects. Kram et al. (2022) note that the theory emphasizes timely intervention through proactive administration of methylene blue. As such, in the context of post-cardiac surgery Vasoplegia prevention, medical professionals must intervene during the initial days of post-operative care to address potential stressors, which would help the patient enjoy improved hemodynamic stability. This proactivity helps nurses avoid this nosocomial condition, optimizing patient outcomes.
The framework uses numerous concepts that are interlinked to interact in ways that promote effective interventions. A common concept is primary and secondary care that promotes and maintains patients’ well-being, system stability, and alignment with proactive intervention strategies using methylene blue (August-Brady, 2000). The tertiary intervention focuses on interventions that eliminate further complications due to unrelated issues, such as poor nursing care or a patient’s demographic factors, such as age. Considering these concepts, the theoretical framework should facilitate methylene blue administration to reduce Vasoplegia occurrence. The study will consider that the patient’s risk profile and the surgical procedure’s complexity affect the probability that patients will develop the condition. The research will also examine the possibility of the mediating role of nitric oxide pathways in promoting vasodilation with methylene blue as the inhibitor.
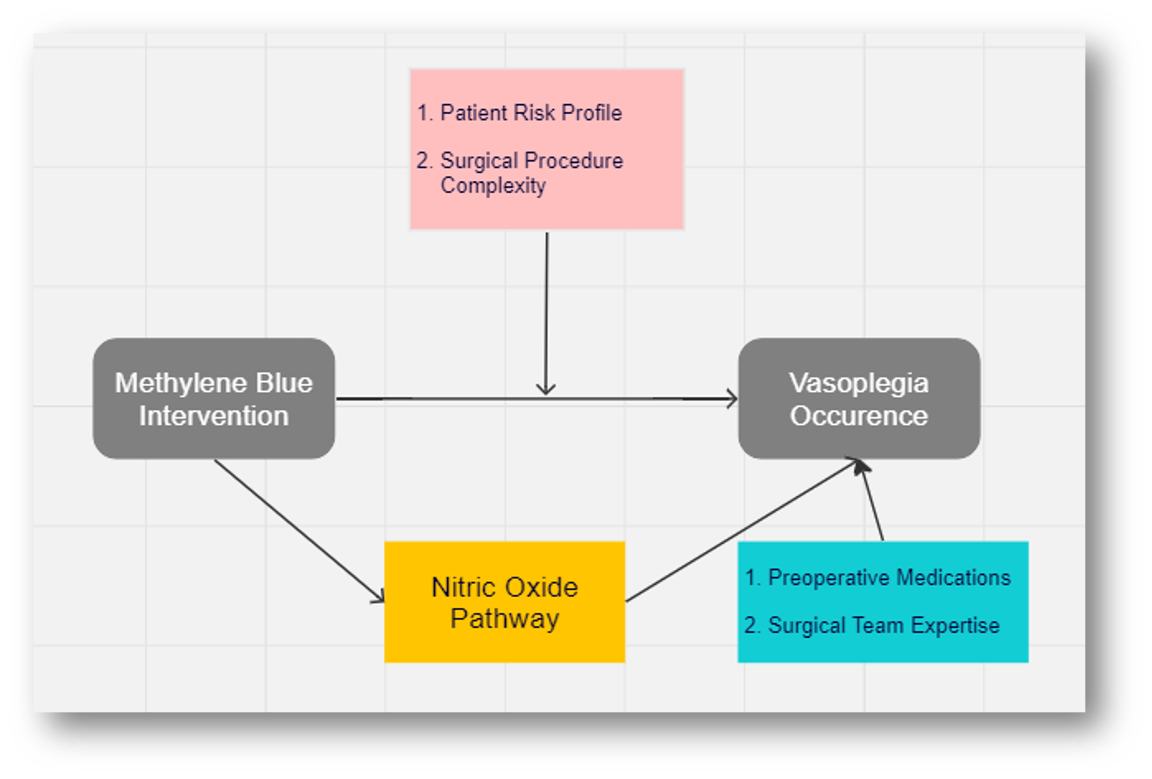
Figure 1: Theoretical Framework
The “Prevention as Intervention” framework has been studied and applied before. August-Brady (2000) demonstrated that implementing the framework improved patient outcomes in ways that reduced post-operative complications. Kram et al. (2022) also revealed that this theory helped nurses establish measures that guided post-cardiac surgery care with admirable degrees of effectiveness. The nurses proactively administered methylene blue to prevent Vasoplegic syndrome, improving patient recovery and outcomes. This administration also aligns with the need for early intervention to mitigate the effects of stressors and maintain system stability. Such literature review offers essential insights into the successful application of methylene blue in varying clinical contexts.
Application of Theoretical Framework
Methylene blue can be incorporated into post-cardiac surgery care as a primary intervention mechanism. By understanding the influence of the moderating effect of high-risk patients, nurses can proactively identify these individuals by establishing a patient risk profile. This profile can inform the intervention, prioritizing such patients and developing a tailored individualized care plan based on the risk factors (Shah et al., 2022). The tailoring also accounts for the surgical procedure complexity revealed in the medical reports, which the surgeons should avail. Such patients would benefit significantly from the primary intervention of methylene blue to prevent the development of the condition. Essentially, the framework’s emphasis on proactivity implies that nurses must be ready with methylene blue to administer to eligible patients timely. This aspect requires collaboration with the pharmacy department for the timely availability of the product.
The theoretical framework will help establish guidelines for applying methylene blue over fluids and vasopressors. The literature review reveals the various ways the intervention has been used, showing the challenges and other takeaways that can help determine the best ways to improve patient outcomes. This information will offer an objective basis for the involvement of experts who can develop consensus guidelines for using methylene blue. These experts can include professors, nurses, and other stakeholders, such as surgeons, anesthesiologists, and critical care specialists. This framework can also facilitate the development of a protocol and influence the definition of best practices around the condition. With support from literature and experts, the framework can help nurses develop clear and standardized ways to approach the administration of methylene blue in eligible post-cardiac surgery patients. This protocol can include approaches to dosing, timing, and patient selection criteria. These guidelines can promote the effectiveness of nurse interventions.
Nurses need ways to help them adopt the “Prevention as Intervention” theory when managing Vasoplegia. These ways can help them apply the framework in clinical settings. They can begin by exploring the nitric oxide pathway to understand its mediating role in the development of Vasoplegia. This exercise would help them contextualize methylene blue’s inhibition role in preventing vasodilation and hypotension. The nurses also find the best shot at adopting the theory by integrating methylene blue as a primary preventative measure based on the theoretical framework. Adaptation forms the conceptual basis guiding nurses when integrating methylene blue into their interventions, which are incorporated into nursing practice. Furthermore, training and education on the working of the theoretical framework can help nurses understand the influence of the theory of Vasoplegia management. Overall, the theoretical model can be applied to promote adapting the “Prevention as Intervention” theory.
Overall, the theoretical framework has desirable implications for improving outcomes and preventing post-operative complications. The framework supports the development of monitoring and evaluation systems that track patient outcomes during primary care. Nurses proactively keep assessing the incidence of Vasoplegia to evaluate the effectiveness of the intervention. It also supports clinical practice integration of methylene blue to ensure its availability and routine application, owing to its effectiveness. Moreover, the framework helps nurses evaluate outcomes to determine the achievement of intended outcomes, such as reduced Vasoplegia incidence, improved hemodynamic stability and decreased morbidity and mortality rates. Overall, the framework’s effectiveness is adequately verifiable due to validating the implications after the outcome assessment.
References
August‐Brady, M. (2000). Prevention as intervention. Journal of Advanced Nursing, 31(6), 1304-1308.
Kram, S., Kram, B., Cook, J., Ohman, K., & Ghadimi, K. (2022). 409: Methylene Blue Dose Response for Vasoplegic Syndrome in Adult Cardiothoracic Surgery. Critical Care Medicine, 50(1), 193.
Maurin, C., Portran, P., Schweizer, R., Allaouchiche, B., Junot, S., Jacquet-Lagrèze, M., & Fellahi, J. L. (2022). Effects of methylene blue on microcirculatory alterations following cardiac surgery: A prospective cohort study. European Journal of Anaesthesiology| EJA, 39(4), 333-341.
Nash, C. M. (2021). Vasoplegic Syndrome in Patients Undergoing Cardiac Surgery: A Literature Review. AACN Advanced Critical Care, 32(2), 137-145.
Shah, A., Patel, A., Bhatt, H., Apigo, A., Huang, K., Friedman, S., … & Puskas, J. (2022). 408: Perioperative Pregabalin Implementation in an Enhanced Recovery After Cardiac Surgery Protocol. Critical Care Medicine, 50(1), 193.
 write
write