GENESIS
Physician-assisted suicide and euthanasia refers to intentional or deliberate measures taken intending to end a life, for the purpose of relieving persistent suffering. It’s mainly applied among patients whose “natural death has become reasonably foreseeable” (Ezekiel, p.793-802). It suggests that solitary the patient with critical health stage with a low probability of survival remain appropriate for Euthanasia. Euthanasia is illegal in most countries and may lead to imprisonment, with American laws regarding euthanasia varying between states.
Physician-assisted suicide has been a topic of debate for a long time; therefore, it is regarded as emotive and controversial topic. The controversies and debate about the topic dates as early as 1800s, when the first law against euthanasia was passed in the state of New York in the United States (Ezekiel, p.793-802). Other American states followed suit in time. A bioethicist known as Ezekiel Emanual, of the (NHI) American National Institutes of Health in the 20th century, argued that the contemporary euthanasia era commenced by the accessibility of anesthesia. Around 1938 a society of euthanasia was started in America to campaign for assisted-suicide. Euthanasia became legalized in 1937 in Switzerland, with the condition that the health care profession ending the life of the patient gains nothing in return. In the 1960s, the process of approval for the right-to-die appeal to euthanasia heightened (Ezekiel, p.793-802). In the year 2002 the Netherlands legalized physician-assisted suicide and lifted some rules/restrictions. During the same year, approval of physician-assisted suicide happened in Belgium.
Today, certified ethics committees exist in American hospitals, nursing homes and other treatment centers, and living wills, or advance health directives are common worldwide. These was legalized in the California state in 1977, legalization in other states happened later (Baruch). The living will mainly entail an individual stating their wishes in terms of treatment/medical care, in case they are unable to make choices/decisions in the future. Approval of non-active euthanasia use by the supreme court happened in 1990. In addition, voters based in Oregon in 1994 approved/passed the Death with Dignity Act, permitting medical professionals to help terminal patients with low chances of survival, that is patients not expected to live for more than 6 months (Baruch). The Supreme Court of the US put such laws in place in 1997, and in 1999 Texas legalized non-active euthanasia. Around 57.91% of voters in the state of Washington in 2008 voted favoring the act of Death with Dignity which was passed as a law in the year 2009.
DENOTATION
- Active Euthanasia- This involves a person deliberately and directly causing a patient’s death.
- Assisted suicide- In assisted-suicide, the patient who desires to die requires assistance to end their life, therefore they ask for the help and gets it (Paul, p.1699-1705).
- Competence- a patient who understands their medical condition, the likely subsequent course of their illness, and the benefits and risks connected with the condition’s treatment; and who is able to talk about their wish is referred to as a competent patient.
- Dignity- This refers to the value accorded to a human being for their existence, which is not connected to any action or property of the person.
- DNR- These abbreviations stand for Do Not Resuscitate. They instruct a healthcare professional not to try resuscitating the patient, in case of a heart attack.
- Indirect euthanasia- This is whereby treatment is provided to a patient (mainly to decrease pain) which has a predictable intricacy of bring about the patient’s death sooner
- Involuntary euthanasia- In this case, patient who dies is killed without their consent. Involuntary euthanasia is classified as murder (Paul, p.1699-1705).
- Non-voluntary euthanasia- This happens when the patient is unable to request for euthanasia (probably due to being unconscious or incapable of communicating), or making a meaningful decision between dying and living, and an appropriate person takes the decision on their behalf, perhaps in accordance with their living will, or previously expressed wishes (Jmaes).
- Palliative care- This term refers to emotional, medical, spiritual or psychosocial care offered to a terminally ill person, which aims at decreasing suffering instead of curing.
- Passive euthanasia- In this kind of euthanasia death occurs through an omission, for example, by withholding or withdrawing treatment with the aim of letting the patient die.
- PAS- The abbreviation stands for Physician-assisted Suicide.
- Voluntary euthanasia- This refers to a situation whereby the patient who dies voluntarily requested a physician-assisted suicide to be conducted on them.
CONNOTATION
Assisted suicide and euthanasia are worth discussing today, because the topic is faced by many controversies and arguments, and a solid stand either for or against the practice that cuts through the religion, authority, science and medicine and human values and morals need to be drawn. The topic has become popularized through debates by the government officials and also involving citizens in taking part in voting for or against the practice. News and stories on the media concerning assisted suicide or euthanasia have become more common, for example; an Australian scientist known as David Goodall, recently ended his life in the country of Switzerland under the assisted-suicide law of the country (Payne, Daniel & USA TODAY). Goodall’s suicide path was assisted by an organization that helps people end their lives called Exit International.
Euthanasia is currently gaining more popularity in most countries of the developed world. The parliament of the New Zealand is presently discussing about its legalization. In Guernsey in the United Kingdom, a proposal for legalization was voted down recently, but in bordering Jersey most of the politicians looking to be voted in support legalization. Outright euthanasia and assisted suicide are legal in majority of the countries in the Western Europe: Belgium, Switzerland, the Netherlands, Luxembourg. In the United States, meanwhile, euthanasia is legal in the District of Columbia and several states.
OPPOSING / DIVERGENT VIEWS
Physician-assisted suicide and euthanasia is surrounded by major arguments both for and against the practice.
ARGUMENTS FOR
- Freedom to make a choice; supporters pass arguments that the ill individual should be given a chance to make a decision for their life.
- Life quality: It’s only the ailing person that clearly knows how the sickness makes them feel, and ways in which the emotional and physical pain of the disease and lengthened death impact their life quality (James).
- Resources: It is more sensible to focus the available resources of equipment, highly-skilled staff, medications and hospital beds towards life-saving care/treatments for patients/individuals willing to live, instead of those who do not wish to continue living.
- Humane: It is considered more humane allowing an individual having an unmanageable suffering to choose to do away with the suffering, through death (Samia & Mauron p.271-273).
- Loved ones: Physician assisted suicide or euthanasia helps in shortening the suffering and grief of people around the patient or those that care about the patient.
ARGUMENTS AGAINST
- The role of the doctor: Physicians, doctors and other medics might be not willing to compromise the roles of their profession, mainly if there is an oath involved for example, Hippocratic Oath (Daniel, p. 246-257).
- Religious and mora arguments: Most religions classify physician-assisted suicide as murder and thus, term it as morally unacceptable. Committing suicide, is also seen to be “illegal” in almost all religions. In line with human values and morals, people argue that physician-assisted suicide will lead to the weakening of life’s sanctity by the society.
- Patient competence: Physician-assisted suicide is only considered voluntary if the ailing individual is said to be mentally competent, and has a strong understanding of the available alternatives and their results and the capability to show that comprehension and their desire to end their life. Defining or determining competence in most cases is complicated or rather not straight forward (Manne, p. 225-230.)
- Guilt: Ailing individuals may feel that they are burdening their loved ones or the resources, and therefore feel psychologically forced into consenting. Mostly, they tend to feel like the mental, emotional and financial burden is too great on their family/loved ones. Even in situations where the treatment cost is catered for by the government, there is usually a risk that the hospital personnel/ healthcare professionals might have/initiate an economic reason to motivate euthanasia consent.
- Mental illness: An individual with depression for example, has high chances of asking for euthanasia, making the decision complicated (Daniel, p. 246-257).
- Slippery slope: There is the likelihood of a risk that euthanasia will begin with the terminally ill people and those who wish to end their lives due to intractable suffering, and later begin to encompass other individuals.
- Palliative care: availability of professional and excellent palliative care renders euthanasia unnecessary (Manne, p. 225-230).
- Regulation: Proper regulation of euthanasia is close to impossible.
SYSTEMS / MODEL / THEORIES:
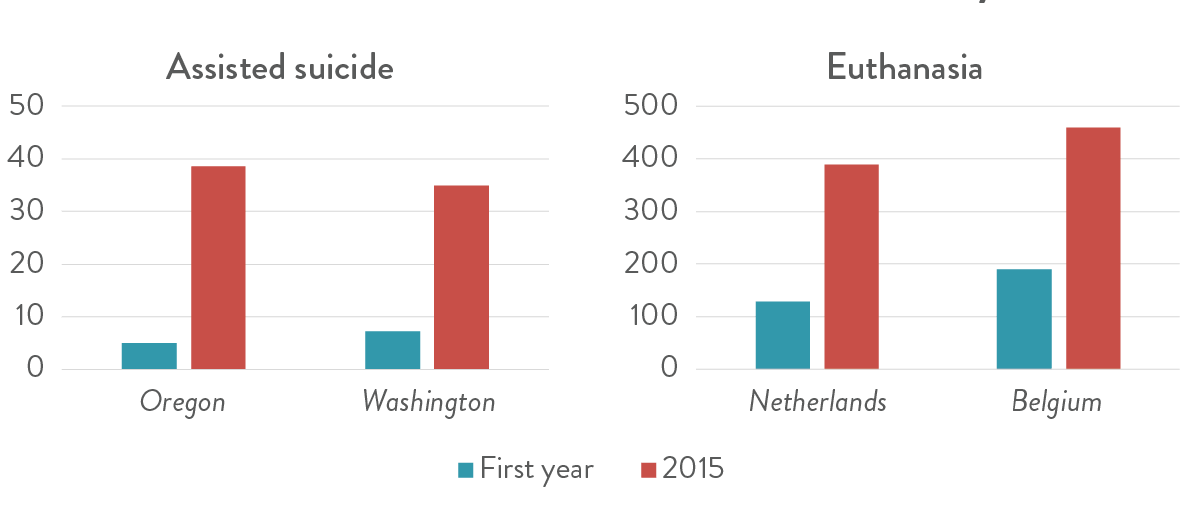
The graph above shows that since the first year of legalization of assisted suicide and Euthanasia to 2015 in Oregon, Washington, Northlands and Belgium numbers of the cases have been increasing, although at different rates for each country.

The image shows a campaigner known as Noel Conway who challenged the UK government against the ban of assisted suicide after he was diagnosed with motor neuron disease.
Works Cited
Brody, Baruch A., ed. Suicide and euthanasia: historical and contemporary themes. Vol. 35. Springer Science & Business Media, 2013.
Emanuel, Ezekiel J. “The history of euthanasia debates in the United States and Britain.” Annals of internal medicine 121.10 (1994): 793-802.
Hurst, Samia A., and Alex Mauron. “Assisted suicide and euthanasia in Switzerland: allowing a role for non-physicians.” Bmj 326.7383 (2003): 271-273.
Payne, Daniel, and USA TODAY. “Assisted Suicide is Not About Autonomy. It’s a Tragedy That We Shouldn’t Allow.” USA TODAY, 1 June 2018, www.usatoday.com/story/opinion/2018/06/01/assisted-suicide-tragedy-devalues-life-euthanasia-column/652290002/.
Rachels, James. “The end of life: euthanasia and morality.” (1986).
Sjöstrand, Manne, et al. “Autonomy-based arguments against physician-assisted suicide and euthanasia: a critique.” Medicine, Health Care and Philosophy 16.2 (2013): 225-230.
Sulmasy, Daniel P., et al. “Non-faith-based arguments against physician-assisted suicide and euthanasia.” The Linacre Quarterly 83.3 (2016): 246-257.
Van der Maas, Paul J., et al. “Euthanasia, physician-assisted suicide, and other medical practices involving the end of life in the Netherlands, 1990–1995.” New England Journal of Medicine 335.22 (1996): 1699-1705.
 write
write