Introduction
In the previous assignments, I outlined the challenge of diabetes care among African American patients at the physician group facility. So far, it is evident that leveraging data is an important strategy for identifying gaps and areas for improvement in our physician group. This proposal aims to outline a plan for collecting comprehensive medical record data over the past 2 years to identify gaps and areas of improvement. The target sources of information for this project include the electronic medical record (EMR) system and pharmacy database at the facility which will provide patient data including demographics diagnosis, laboratory test results, medications, treatment plans, and clinical nots. The EMR is used throughout all departments in healthcare facilities meaning that it will contain data across inpatient outpatient, specialist, and pharmacy settings. The aim of health information collection is to comprehensively evaluate the quality of care delivered by our physician group with evidence-based guidelines. The focus is to identify the gaps and strengths in the management of diabetes among African American populations suffers a disproportionately high burden of diabetes and worse outcomes compared to other demographics. The insights obtained from this information review will help t make decisions and recommendations on the most appropriate targeted initiatives that can be used in enhancing equality in diabetes care while reducing complications and the cost of healthcare.
Data Collection Plan
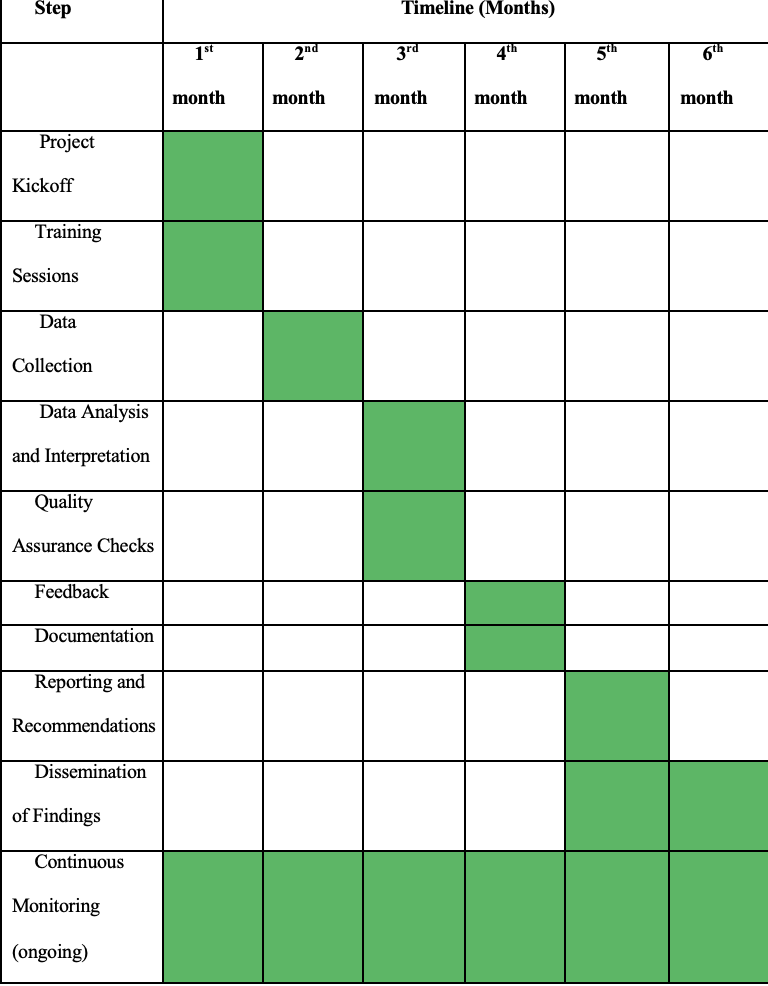
The data review processes will take 6 months where a multidisciplinary team will be involved on gathering, assessing and integrating patient health information for analysis to identify gaps in the delivery of diabetes care services to African American patients. The main sources of information will be the pharmacy management system and the Electronic Medical Record (EMR) system at our physician group. The EMR system comprises of information on patient demographics, treatment histories, diagnosis, treatment plans and outcomes, while the pharmacy management systems provide information about the patient’s prescribed medications.
The sources will be augmented by the regional HIE network, which will support the electronic transfer of patient health information between our facility and other healthcare organizations according to the national standards. The advantage of adopting HIE in the project as a source of information is that it can provide insights on costs of healthcare for patients, and ensures completeness of data being sought for review, by providing insights on patient histories that are not available at the facility’s internal information systems (Menachemi et al., 2018). The data collection process will target patient health data obtained between November 2021 and November 2023.
Information Lifecycle Flow
| Stage | Description |
| Patient Encounter and Documentation | Clinical personnel document details in intake forms, assessments, diagnostic orders, procedure notes, and care plans during patient visits |
| EMR Data Aggregation | Patient data from encounters migrated into a centralized EMR application |
| External Data Retrieval | Leverage regional Health Information Exchange (HIE) to access patient history documentation from external affiliated providers. |
| Clinician Chart Documentation | Physician specialists augment records with subjective/objective findings, treatment adjustments, and follow-up coordination plans. |
| Quality Control Check | Validate the accuracy and consistency of collected data |
| Data Access Monitoring | Ongoing auditing of EMR system access, authorization levels, patient record visibility |
| Archived Storage | Upon reaching the 7-year retention mark, profiles shifted into secured offline systems. |
| Secure Data Destruction | Deploys encryption, shredding, and physical destruction to deidentify residual data fully |
Personnel and Strategies for Implementation
The project will be completed by medical records, data analysis, and IT support professionals. The medical records team monitors patients’ health histories, enters data, audits, and processes data. This project requires them to collect and analyze crucial data. Data analysts will analyze the data to identify diabetes care delivery trends, projections, strengths, and gaps. Two IT specialists will provide technical support during data extraction and processing. Training is essential for project success since Lack of data retrieval skills, time, database searching training, and access limits pose significant challenges to using evidence-based information (Lee et al. (2019). Therefore, hospital administration will provide team members enough time and training to efficiently gather data for evidence-based decisions. The trainings will cover HIPAA compliance, data extraction from EMRs and pharmaceutical management systems, and patient data protection. Effective communication and feedback mechanisms will be implemented to allow the exchange of ideas, problem solving, and data modification approaches.
Data Security Plan
To safeguard protected health information (PHI), data reports will be securely stored on a password-protected work computer accessible only to authorized personnel. Encryption protocols will be applied to all files and directories containing sensitive information, ensuring additional data security (McNary, 2021). The analysis will occur in a private office secured via keycard access, limiting access to designated individuals. System permissions for the project will be granted selectively to generate patient data reports for approved quality improvement initiatives, marking them confidential and accessible only to the Chief Medical Officer and authorized personnel in an oversight role if required. Moreover, legal considerations under the HIPAA Privacy Rule will be strictly adhered to, mandating reasonable safeguards for confidentiality, integrity, and access management when handling identifiable patient data. Compliance authority rests with the designated privacy officer, overseeing the enactment of HIPAA Security Rule standards through staff training, system controls, third-party risk analysis, and mitigation (Edemekong et al., 2022). Robust incident response plans, aligned with federal and state-level breach notification laws, will be in place to address any potential reportable disclosures promptly.
Benchmarking Plan
Benchmarking against the national data on diabetes care is essential for comparison of the care quality. The national data will be obtained from renown databases such as Disease Control and Prevention (CDC), and National Institute of Health (NIH) (CDC, 2023). The sources will provide evidence-based guidelines developed based on research and national healthcare data. They are also undergoing frequent updates to guarantee that the information provided is current and objective, enabling the physician group to adjust to changing standards and best practices.
This data review focuses on patient outcomes, diabetes complications, and clinical guideline adherence. Facility data will be compared to national data, guidelines, and HIE network data. Health Level Seven (HL7) protocols will standardize HIE data from different hospitals and departments that use tailored EMR solutions that fit their needs and clinical operations. Thus, Health Level Seven (HL7) protocols are essential for integrating EMR with patient decision aids and addressing software issues like troubleshooting, data flow security when using third-party solutions, and functionality issues when updating EMRs (AlQudah et al., 2021). The HL7 protocols promote standardization of communication interfaces between applications that use multiple data formats and require data exchange or transfer. They enable the sharing, integration, exchange, and retrieval of electronic healthcare data stored in multiple systems (AlQudah et al., 2021).
Quality and Change Management Strategies
The purpose of this project is to evaluate the efficacy of the medical group’s diabetes care practices and to identify areas that require improvement. The information review study’s findings will direct the development of patient education initiatives, evidence-based diabetic care treatment plans, and prevention initiatives targeted at African American patients (Albright et al., 2022). The outcomes will also inform the refinement of policies, at the facility to align with the latest evidence-based best practices.
Streamlining processes and ensuring efficiency in departmental workflows can be achieved through effective automation and adoption of health information technology. According to Zayas-Cabán et al. (2022), automation helps in processing the ever-expanding data and complex tasks in healthcare that is characterized by interconnected administrative clinical and population-level workflows. The adoption of health information technology creates new opportunities for multidisciplinary interaction and communication. Zayas-Cabán et al. (2022) recommended that establishing confidence in the design and implementation, carrying out continuous testing and assessment, and comprehending the pertinent workflows are the foundations for effective automation. Therefore, establishing standard procedures for gathering, recording, and overseeing health information, fostering collaborative multidisciplinary teams, and providing continuous training to staff members on the most recent developments in diabetes treatment, data gathering methods, and technological advancements can streamline workflows (Albright et al., 2022).
Incorporating Evidence-Based Best Practices
The physician group can help make the necessary changes by using evidence-based best practices. Adopting patient-centered care models can improve patient satisfaction, engagement, and overall health outcomes by customizing care plans to meet the requirements and preferences of each patient (Kuipers et al., 2019). Additional telehealth outreach initiatives are necessary to enable real-time monitoring, patient education, and self-management support, particularly for individuals with mobility or geographical limitations (Abdelhamid, 2018). Ajuwon and Love (2020) also recommend cultural competence training to healthcare practitioners due to social and cultural determinants of diabetes in the African-American community.
Implementation
Conclusion
The aim of this medical information review is to identify gaps in the implementation of evidence-based guidelines for diabetes care at our physician group. The project was informed by the high prevalence of diabetes among African Americans compared to the other races. The data targeted for this project is from the EMRs and pharmacy management systems at the facility which will also be augmented by the local HIE network. The insights obtained from the data analysis will be used to develop targeted interventions for bridging the gap in delivery of quality and up-to-date evidence-based care to underserved patent populations.
References
Albright, K., Navarro, E. I., Jarad, I., Boyd, M. R., Powell, B. J., & Lewis, C. C. (2022). Communication strategies to facilitate the implementation of new clinical practices: a qualitative study of community mental health therapists. Translational Behavioral Medicine, 12(2), 324–334. https://doi.org/10.1093/tbm/ibab139
Abdelhamid, M. (2018). Greater patient health information control to improve the sustainability of health information exchanges. Journal of Biomedical Informatics, 83, 150-158. https://doi.org/10.1016/j.jbi.2018.06.002
Ajuwon, A. M., & Love, R. (2020). Type 2 diabetes and depression in the African American population. Journal of the American Association of Nurse Practitioners, 32(2), 120–127. https://doi.org/10.1097/JXX.0000000000000240
AlQudah, A. A., Al-Emran, M., & Shaalan, K. (2021). Medical data integration using HL7 standards for patient’s early identification. PloS One, 16(12), e0262067. https://doi.org/10.1371/journal.pone.0262067
Centers for Disease Control and Prevention. (2023, November 29). National Diabetes statistics report: Estimates of Diabetes and Its Burden in the United States. https://www.cdc.gov/diabetes/data/statistics-report/index.html#print
Edemekong, P. F., Annamaraju, P., & Haydel, M. J. (2022). Health insurance portability and accountability act. In StatPearls [Internet]. StatPearls Publishing.
Kuipers, S. J., Cramm, J. M., & Nieboer, A. P. (2019). The importance of patient-centered care and co-creation of care for satisfaction with care and physical and social well-being of patients with multi-morbidity in the primary care setting. BMC Health Services Research, 19(1), 13. https://doi.org/10.1186/s12913-018-3818-y
McNary A. L. (2021). Maintenance and destruction of treatment records. Innovations In Clinical Neuroscience, 18(4-6), 44–47. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8667710/
Menachemi, N., Rahurkar, S., Harle, C. A., & Vest, J. R. (2018). The benefits of health information exchange: an updated systematic review. Journal of the American Medical Informatics Association: JAMIA, 25(9), 1259–1265. https://doi.org/10.1093/jamia/ocy035
Zayas-Cabán, T., Okubo, T. H., & Posnack, S. (2022). Priorities to accelerate workflow automation in health care. Journal of the American Medical Informatics Association: JAMIA, 30(1), 195–201. https://doi.org/10.1093/jamia/ocac197
Lee, A., Alving, B. E., Horup, M. B., & Thrysoee, L. (2019). Information retrieval as a part of evidence-based practice: Retrieval skills, behavior and needs among nurses at a large university hospital. Nordic Journal of Nursing Research, 39(4), 201-208. https://doi.org/10.1177/2057158519866612
 write
write