The evidence-based project (EBP) in nursing is critical because it assimilates patient preferences, clinical expertise, and research evidence toward a patient’s enhanced outcomes. Through EBP, the nurses provide individualized patient care specific to treatment goals. The EBP is significant because registered clinicians are mandated to provide patient care through validated interventions that have been tried and tested. Such strategies have proven essential, which is why different nursing programs incorporate EBP into their coursework. The EBP is also significant because the concept assists medical practitioners in pinpointing specific care strategies. Evidence-based project interventions are not only applicable in nursing but in other areas of the medical profession as well.
How EBP gets Integrated into Nursing
The EBPs are vital because they enable nurse practitioners to identify ways or a practical course of action to be administered in care delivery (Horntvedt et al., 2018). As a result, EBP entails five key phases that can be summarized as follows:
- Problem identification
- Acquiring the best evidence
- Analyzing the evidence
- Using evidence in clinical practice
- Assessment of the results
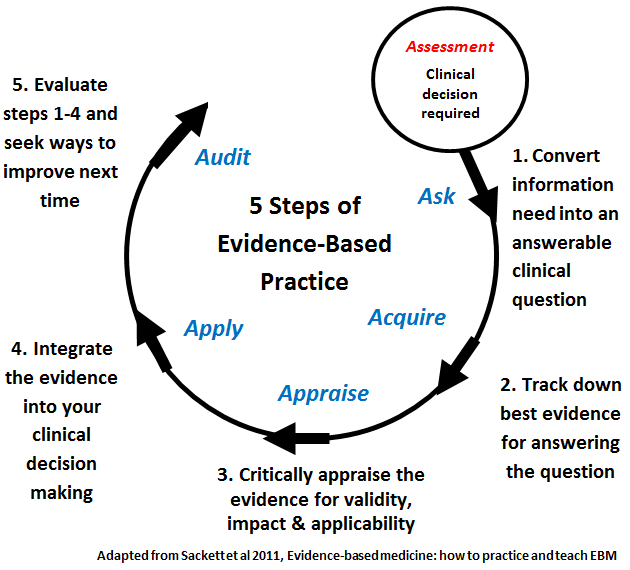
Fig 1.0: Illustration of the phases of evidence-based practices
The Benefits of EBP to Nurses and Patients
There are a lot of significant advantages that both the patients and nurses tend to benefit from when they apply EBP. To begin with, EBP provides the medical fraternity with scientific-backed research integrated with real-time and data-driven insights to make an informed clinical decision (Valizadeh et al., 2020). Through the EBP, the medical fraternity can be constantly updated regarding novel medical protocols that can be applied for enhanced patient care. Through queries involving documented interventions resonating with patient-specific profiles, it is easier for the nurses to enhance the chances of their patient’s recovery with minimal effort (Stannard, 2019). The EBP also enables the nurses to assess different research works to review some of the potential risks or effectiveness regarding treatments or even diagnostic procedures. Using the EBP concept enables medical practitioners to include the patient’s needs in their nursing care plans. The patient is accorded a proactive role in their healthcare due to the ability to voice concerns, and preferences, share values or even input their suggestions on how best they think they should be treated.
One notable advantage with EBP, especially to healthcare organizations, is that there are more enhanced patient outcomes, a situation likely to decrease demand for healthcare resources. As a result, the healthcare entities directly streamline operational expenditures (Mathieson et al., 2019). For instance, previous bureaucratic processes may involve supplies or ordering unnecessary medication, but with EBP, such agony is eliminated.
Components of Evidence-Based Practices
Three components are used in evidence-based practices (EBPs), and they include:
- Best external evidence: It is always prudent to utilize the most updated and clinically relevant scientific research works whenever seeking clinical interventions
- Individual clinical expertise: The nursing practitioner must utilize their clinical work experiences regarding issues that have previously worked and failed
- Patient values and expectations: The individual patients’ preferences must be valued and prioritized
Besides, the nursing expert must also be alert so that despite an intervention appearing to be feasible, they should also be inculcating their sixth sense, common sense (Peñataro-Pintado et al., 2021).
Key Examples of EBP in Nursing
Several clinical procedures have adopted evidence-based practices to enhance overall patient care. Some of the critical examples of EBP include:
- Providing oxygen to patients with chronic obstructive pulmonary diseases (COPD): A nursing expert can use evidence to review the best approaches on how the patients can best be provided with oxygen
- Measuring blood pressure noninvasively, The clinician may apply an auscultatory technique and evaluate the results against the data acquired through the oscillometric method, following the evidence.
- Applying the most appropriate intravenous catheter size: The clinicians must integrate the application of smaller gauge catheters to enhance the patient’s comfort hence improving their overall clinical experience.
PICOT and its Significance in EBP
The PICOT is an acronym for the patient-oriented clinical question and is widely utilized in EBP. The justification for using the concept in EBP is that it can be used as a mechanism that identifies the search jargon used to retrieve the only evidence of a burning issue.
One PICOT query we need to investigate is the search strategy leading to an unbiased and practical search criterion. In a typical case, the concept starts with a case scenario, whereby a query gets phrased to elicit a response to a contentious issue (Boswell & Cannon, 2022). The framework is significant in EBP because it enhances clinical issues’ specificity and conceptual vividness. Besides, the technique also tends to produce more information and ideas during the pre-search phases, generating more search strategies with precise results. The framework is also essential in guiding the nurse practitioner on what needs to be done or not, including the latest research regarding the subject matter.
For the EBP, the picot questions are as follows;
P- what is the population of the patient? In terms of age, gender, or health status.
I-What is the plan to help the patient? It will include the EBP medication and therapies.
C-What is the available alternative for treatment? It includes other forms of treatments like holistic counseling of the patients.
O- What is the outcome expected from the intervention? The expectations are typically reduced symptoms and recovery.
T-What is the expected time frame-It is the timeframe for the effects of the treatment to be realized?
Conclusion
Conclusively, when nurses apply scientific evidence to their nursing practice, they are likelier to provide exceptional quality levels regarding self-care by enhancing patient outcomes while improving their overall career prospects. As a result, the nurses must understand the best approaches they may apply in evaluating different researches, making more informed decisions, and delivering an optimum care experience. Such attainment is only possible through evidence-based practice in nursing.
References
Boswell, C., & Cannon, S. (2022). Introduction to nursing research: Incorporating evidence-based practice. Jones & Bartlett Learning.
Horntvedt, M. E. T., Nordsteien, A., Fermann, T., & Severinsson, E. (2018). Strategies for teaching evidence-based practice in nursing education: a thematic literature review. BMC medical education, 18(1), 1-11.
Mathieson, A., Grande, G., & Luker, K. (2019). Strategies, facilitators, and barriers to implementing evidence-based practice in community nursing: a systematic mixed-studies review and qualitative synthesis. Primary health care research & development, 20.
Peñataro-Pintado, E., Díaz-Agea, J. L., Castillo, I., Leal-Costa, C., Ramos-Morcillo, A. J., Ruzafa-Martínez, M., & Rodríguez-Higueras, E. (2021). Self-learning methodology in simulated environments (MAES©) as a learning tool in perioperative nursing. An evidence-based practice model for acquiring clinical safety competencies. International Journal of Environmental Research and Public Health, 18(15), 7893.
Stannard, D. (2019). A practical definition of evidence-based practice for nursing. Journal of PeriAnesthesia Nursing, 34(5), 1080-1084.
Valizadeh, L., Zamanzadeh, V., Babaei, N., & Avazeh, M. (2020). Challenges and strategies for implementing evidence-based practice in nursing: a systematic review. Research in Medical Education, 12(3), 55-67.
 write
write