Our healthcare approach relies on the Clinical Decision Support (CDS) system for Clostridium difficile infection (CDI) Quality and Patient Safety (QPS). This approach uses advanced technology and clinical knowledge to help professionals diagnose, treat, and manage CDI. It promotes CDI patient safety and high-quality care.
Our CDS system for CDI aims to improve clinical outcomes by giving healthcare practitioners evidence-based recommendations. It helps detect CDI early, diagnose it accurately, and treat it. Clinical expertise, patient-specific data, and best practices are used to provide real-time decision assistance to healthcare providers, minimizing CDI complications and enhancing patient safety (Korpela et al., 2020). The CDS system in CDI affects diverse stakeholders like physicians, nurses, pharmacists, hospital administrators, infection control teams, laboratory workers, and patients. These stakeholders are crucial to the CDI care continuum, and the CDS system gives them the tools and knowledge to make educated decisions, improving patient safety and care quality.
The CDS system for CDI uses certain decision-support parameters and criteria. To diagnose CDI, inclusion criteria include patient age, symptoms, recent antibiotic usage, and laboratory results. Exclusion criteria reduce unnecessary CDI testing by identifying illnesses that may mimic CDI symptoms or lower CDI risk. The CDS system for CDI processes patient-specific data using rules and logic engines. It compares the patient’s clinical data to CDI diagnosis and management standards and best practices using algorithms (D’Agata et al., 2021). The principles and logic evaluate CDI severity, offer diagnostic tests, and recommend patient-specific treatment regimens, ensuring patient-centered care.
The CDS system for CDI is updated with the latest evidence-based research, clinical guidelines, and expert suggestions. CDS integrates easily with healthcare practitioners’ clinical procedures. It interacts with EHRs and lab information systems. A healthcare provider can access the CDS system in the EHR for suspected CDI patients. It delivers real-time CDI diagnosis, test recommendations, treatment options, and antibiotic stewardship (Feuerstadt et al., 2023). The CDS system guarantees that CDI-related choices follow best practices by functioning within the clinical workflow, helping us reach our QPS aim of improving patient safety and CDI care.
Critical Evaluation of the Existing CDS System for CDI
Existing CDS for CDI has many benefits. It helps professionals recognize and treat CDI early with evidence-based recommendations. This reduces CDI complications and improves patient safety. The system’s overreliance may impair clinical judgment, and it must be updated to meet changing CDI guidelines and practices. The CDS system for CDI helps healthcare practitioners provide high-quality treatment while following CDI requirements. The system requires proper input data and cannot substitute clinical competence. It may not adapt to unusual or atypical CDI cases (Chandrasekaran et al., 2017). Physicians, nurses, and pharmacists utilize CDS for CDI most. The system’s evidence-based recommendations improve diagnosis accuracy and therapy choices, influencing their decisions. In CDI clinical settings, the CDS system helps healthcare professionals give the best treatment to patients. CDS integrates efficiently into clinical workflows, saving decision-making time and standardizing CDI diagnosis and care. It simplifies CDI testing, treatment initiation, and antibiotic stewardship, improving efficiency and patient care (Gerding et al., 2016). The existing CDS system requires frequent changes to reflect new evidence and risks user overreliance. Improved adaptation to unusual CDI cases, user trust, and clinical workflow integration could improve the system.
Design Improvement Proposal for CDI
After critically evaluating the CDS system for CDI, numerous design adjustments can be made to improve its efficacy and align it with the changing CDI management landscape.
- Real-time Data Integration: The CDS system should integrate real-time data from electronic health records, test results, and patient history to overcome the problem of relying on reliable input data.
- Adaptive Algorithm: The system should have an adaptable algorithm that adapts to user interactions and healthcare guidelines. This allows the system to adjust to unusual or atypical CDI cases, keeping it relevant and effective.
- User Training and Support: The CDS system should incorporate extensive user training and support to reduce overreliance and user discomfort. Healthcare providers can use the system’s recommendations as a supplement to their clinical experience with training courses and expert guidance.
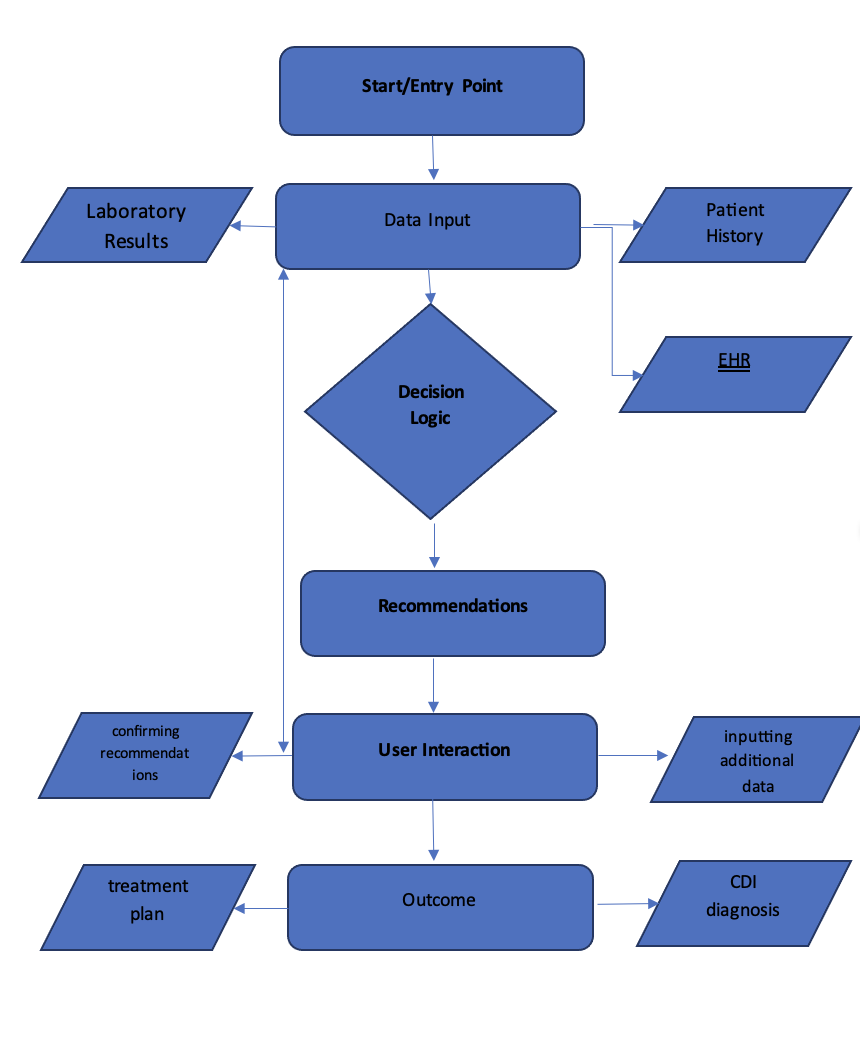
Current State of CDI CDS Tool
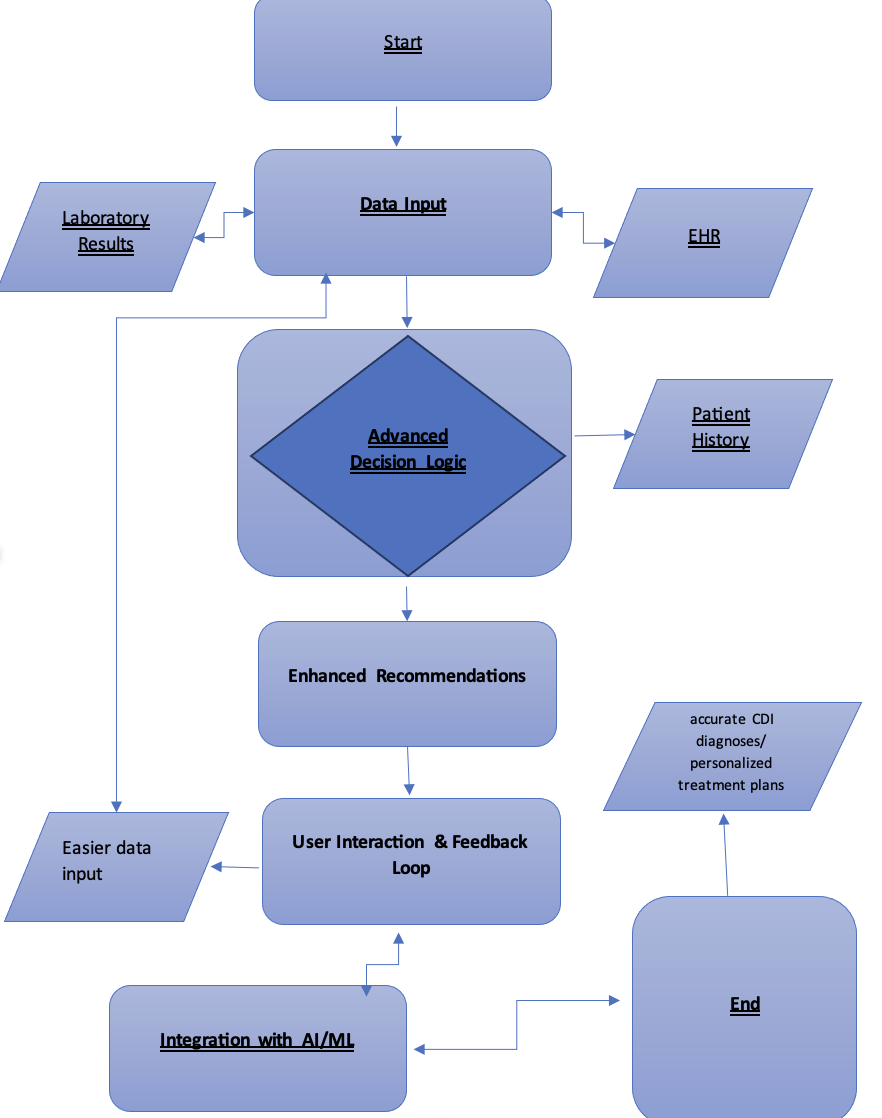
Future State of CDI CDS Tool with Design Improvements
Reflection on CDS System’s Role in CDI
The Clinical Decision Support (CDS) system improves Clostridium difficile infection patient safety and healthcare quality. CDI is a difficult healthcare issue that can harm individuals, healthcare facilities, and care quality (White et al., 2017). The CDS system, as part of the Quality and Patient Safety (QPS) initiatives, provides several crucial contributions:
- Early Detection and Diagnosis: Healthcare providers can quickly and accurately detect CDI cases using the CDS system. Integrating patient data, clinical recommendations, and real-time information helps detect CDI symptoms and risk factors early.
- Individualized Treatment: Patients’ unique clinical profiles are used to provide CDS therapy recommendations, which improves patient safety. Treatment is adjusted for each patient by considering history, comorbidities, and antibiotic exposure.
- Infection Control Measures: In addition to patient care, the CDS system guides institutional infection control. It helps track CDI trends, identify outbreaks, and adopt preventive measures. Protecting patients and healthcare staff from CDI transmission requires this proactive strategy.
- Clinical Workflows: Clinical workflows are streamlined by CDS’s evidence-based suggestions and real-time notifications. This streamlines decision-making and ensures CDI management best practices are followed, eliminating errors.
The suggested Clinical Decision Support (CDS) system design improvements for Clostridium difficile infection (CDI) could significantly benefit healthcare quality and patient safety. Enhancements in important areas will improve healthcare across various dimensions. The enhancements prioritize CDI diagnosis and treatment accuracy and efficiency. Doing so helps CDI patients receive timely and precise care, minimizing the risk of serious consequences. This increased precision improves patient well-being and healthcare quality by streamlining CDI management. The design improvements will also help fight antibiotic resistance, a rising healthcare issue. Optimizing antibiotic dosing and adapting CDI therapies to case characteristics may reduce antibiotic resistance.
References
Chandrasekaran, Ramyavardhanee, and D. Borden Lacy. “The Role of Toxins in Clostridium Difficile Infection.” FEMS Microbiology Reviews, vol. 41, no. 6, 18 Oct. 2017, pp. 723–750, https://doi.org/10.1093/femsre/fux048.
D’Agata, E. M. C., Apata, I. W., Booth, S., Boyce, J. M., Deaver, K., Gualandi, N., Neu, A., Nguyen, D., Novosad, S., Palevsky, P. M., & Rodgers, D. (2021). Suggestions for the prevention of Clostridioides difficile spread within outpatient hemodialysis facilities. Kidney International, 99(5), 1045–1053. https://doi.org/10.1016/j.kint.2021.02.028
Feuerstadt, Paul, et al. “The Burden of CDI in the United States: A Multifactorial Challenge.” BMC Infectious Diseases, vol. 23, no. 1, 7 Mar. 2023, https://doi.org/10.1186/s12879-023-08096-0. Accessed 5 Sept. 2023.
Gerding, D. N., File Jr, T. M., & McDonald, L. C. (2016). Diagnosis and treatment of Clostridium difficile infection (CDI). Infectious diseases in clinical practice (Baltimore, Md.), 24(1), 3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5769958/
Korpela, K., Renko, M., Vänni, P., Paalanne, N., Salo, J., Tejesvi, M. V., Koivusaari, P., Ojaniemi, M., Pokka, T., Kaukola, T., Pirttilä, A. M., & Tapiainen, T. (2020). Microbiome of the first stool and overweight at age 3 years: A prospective cohort study. Pediatric Obesity, 15(11), e12680. https://doi.org/10.1111/ijpo.12680
White, D. R., Hamilton, K. W., Pegues, D. A., Hanish, A., & Umscheid, C. A. (2017). The impact of a computerized clinical decision support tool on inappropriate Clostridium difficile testing. infection control & hospital epidemiology, 38(10), 1204-1208. https://www.cambridge.org/core/journals/infection-control-and-hospital-epidemiology/article/impact-of-a-computerized-clinical-decision-support-tool-on-inappropriate-clostridium-difficile-testing/A01C48C834E1C8C97745829DB814BE65
 write
write