The phenomenon that happens when the presence of another medication alters the effects of one medicine are referred to as a drug-drug interaction (DDI), one of the types of adverse drug reactions. Because of this interaction, the impact of the drug may be altered, increased, or rendered entirely ineffective. Every pharmaceutical interaction may be classified as either pharmacokinetic, pharmacodynamic, or physical-chemical. These are the three overarching categories (Scheme 2021). A physical-chemical or pharmacological interaction describes what happens when two or more drugs interact with one another primarily due to physical or chemical processes. This is a pharmacodynamic interaction when two drugs have opposing or complementary effects. A pharmacokinetic interaction occurs when one medication impacts the pharmacokinetics of another medication, including that medicine’s distribution, excretion, biotransformation, and absorption (Athamneh, 2020).
The patient, doctor, and pharmacologist may have something to do with the association between risk factors and medication interactions. Patients with a higher propensity to have negative responses to medications are also considered patient-related factors. Patients who fall into this group may have impaired immune systems, be of advanced age, or be the end result of a surgical procedure. There is a correlation between the DDI, pharmacological effectiveness, and medicinal therapeutic potential. It has been shown that medications, depending on their strength, may inhibit or increase enzyme activity (Edrees et al., 2020). The therapeutic index of a medication is the ratio of the highest dosage that can be safely tolerated to the lowest dose that produces the desired effect. Patients brought to the hospital with complex clinical illnesses and, as a result, connected risk factors need considerable amounts of drugs, which are included in the medical prescription. This is the case. It is possible for the therapeutic effectiveness of a medicine to be altered or for new undesirable effects to be brought about by interactions between drugs. A drug can increase the symptoms of a medical condition you already have if you take it. For instance, using a nasal decongestant while treating high blood pressure simultaneously can have unforeseen effects. An interaction between two medications may put the patient’s health at risk or reduce a medication’s effectiveness.
Drug Interactions Occurrence
A pharmacodynamic interaction
It happens when two drugs have an additive (or synergistic) impact on one another or a decreasing (or antagonist) effect on another medication that acts at the same or similar receptor site (Weerink et al., 2019). The risk of a life-threatening abnormal heart rhythm may be increased when two drugs like the antipsychotic haloperidol and the antiemetic chlorpromazine, used to treat nausea and vomiting, are taken simultaneously.
A pharmacokinetic interaction
This can happen if one drug changes how another is absorbed, distributed, metabolized, or excreted. These intricate mechanisms can be better understood with the aid of examples:
Absorption:
Taking another can affect the body’s ability to absorb one drug. Calcium, for instance, can interfere with the absorption of certain drugs by binding with them. Dolutegravir (Tivicay) is an antiretroviral medication, but taking it with calcium carbonate (Tums, Maalox, etc.) can reduce the amount of dolutegravir absorbed into the bloodstream, reducing the medication’s efficacy (Hughes et al., 2022). To avoid this interaction, dolutegravir should be taken at least 2 hours before or 6 hours after taking any medication containing calcium or other minerals. Likewise, many medications should not be consumed alongside milk or dairy products due to the calcium-binding with the pharmaceuticals. There can also be interactions between medicines that change how the digestive tract works, such as its motility, pH, and natural flora.
Distribution:
Once two or more drugs, which are already highly protein-bound, try to occupy the same binding sites on plasma proteins, protein-binding interactions can occur. Fenofibric acid (Trilipix), used to reduce cholesterol and triglycerides in the blood, can have an adverse effect when combined with warfarin, a common blood thinner used to avoid clots (Bouchtout, 2022). Fenofibric acid can worsen warfarin’s anticoagulant effects, which can cause too much bleeding.
Metabolism
To be excreted from the body, drugs must typically be unaltered (parent) drugs or metabolites. Before excretion, drugs are metabolized by liver enzymes called cytochrome P450 (CYP450) enzymes. However, changes in the levels of enzymes can change how drugs are broken down.
Excretion:
When taken with lithium, a medication used to treat bipolar disorder, a few nonsteroidal anti-inflammatory drugs (NSAIDs), including indomethacin, may reduce renal function and alter lithium’s excretion. To safely mix the two drugs, your doctor may need to change your dosage or keep a closer eye on you.
Factors Affecting Drug Interactions
Patient-Related Factors
Some patient-related variables include age, genetics, environment, diet, and drug clearance. Other patient-related variables include environmental factors. Those are sufng from chronic illnesses, those with renal or hepatic impairment, and patients using medications for the cardiovascular or central nervous system, as wellandderly, are at a greater risk of experiencing adverse effects as a reduced interaction. In addition, those who have the post-transplant syndrome, AIDS, or other severe illnesses are more likely to be adversely impacted by the interactions between their medications (Naz et al., 2020). There is also a correlation between advanced age and a greater frequency of DDI. This correlation is increased by variables such as the presence of several illnesses, the use of various medicines, and altered drug disposition. As a direct result of this, adverse effects of DDI become apparent, such as a hazy or inaccurate recollection of drug usage. If over-the-counter medications were also involved, the situation could become far more hazardous (Santos et al., 2019). Some of the most commonly given drugs that include patient-related factors are cyclosporine, lithium, amiodarone, verapamil, methotrexate, and itraconazole. Warfarin and itraconazole are also on this list (Athamneh, 2020). Psychomotor symptoms and hallucinations are prevalent in older adults with DDI due to the interaction between propafenone and venlafaxine. Patients who have epilepsy who take lamotrigine and phenobarbital concurrently have a higher risk of developing blood dyscrasia, whilst taking propafenone and venlafaxine combined might lead to adverse psychological effects (Edrees et al., 2020). According to several studies, macrolides pose a greater risk of theophylline poisoning in children than adults. Infectious and other processes may cause enzymes, cytokines, and drug transporters to undergo changes, which can affect how medications interact. Having an illness can also change the way specific drug interactions happen.
Drug Specific Factors
A drug’s distinctive kinetic and dynamic properties are examples of drug-specific characteristics. Nevertheless, this list is not exhaustive. The number of drugs to be given, their dose; time; formulation; route of administration; and order are all additional factors that should be considered. In addition, the use of many prescribers in conjunction with the widespread utilization of alternative therapies all contributes to an increased likelihood of a pharmaceutical interaction. When many medications are administered to a patient at once, there is a more significant potential for unwanted consequences (Scheme 2021). When more than four prescriptions are handed out simultaneously, and when there are ten to twenty drugs taken, the probability of a clinically meaningful drug interaction increases to as high as twenty per cent rises. The use of this requires the simultaneous administration of two medications, both of which have the potential to cause adverse reactions when combined. In particular, antibiotics, nonsteroidal anti-inflammatory drugs (NSAIDs), and rifampin, in particular, were the precipitants suggested to patients most often in primary care. Drugs with a low therapeutic index or a narrow therapeutic range are more likely to produce negative drug interactions. This is because the therapeutic range of these drugs is limited. Oral contraceptives, cisapride, warfarin, fluoroquinolones, antiepileptics, and 3-hydroxy-3-methylglutaryl coenzyme A-reductase inhibitors are some examples of the types of medications that are often used in the role of object pharmaceuticals (Naz et al., 2020). Researchers have found that drug interactions of this size might often serve as warning indicators. Medications such as cyclosporine, erythromycin, azole antifungals, warfarin, HMG CoA reductase inhibitors, and please are examples of those that fall into this group.
Transporters and Pharmacokinetic Interactions
Alterations in the transport of drugs through cell membranes are the cause of variable drug efflux. These same alterations also impact drug absorption, inflow, excretion, and distribution. Transporters have been shown to have an essential role in the pharmacokinetics of drug interactions. Because of this recent development, it is possible that our perspective on pharmacokinetic processes may shift. ABC transporters, also known as ATP-binding cassette transporters, and SLC transporters, also known as solute carrier transporters, are the two most important types of transporters in humans (Liu, 2019). SLC transporters have been demonstrated to play a crucial role in the transcytotic uptake of neurotransmitters, salt, glucose, and other substances across the membranes of nerve terminals.
Additionally, the SLC transporter is responsible for transporting inorganic and organic molecules, including vitamins, proteins, carbohydrates, ions, metals, medications, xenobiotics, and hormones. SLC transporters exemplify that gamma-aminobutyric acid, dopamine, serotonin, and norepinephrine are transported into adrenergic vesicles by these particular transporters. On the other hand, the ATP-binding cassette transporter superfamily makes use of ATP to move molecules. The ATP-dependent transporter family that has been the subject of the most investigation is the P-glycoprotein efflux transporter family (Vellonen et al., 2018). P-glycoprotein is involved in the efflux of chemicals from the cytoplasm to the extracellular fluid or cell organelle in the bile canaliculi, choroidal epithelium, testicular and placental microvessels, renal tubules, and intestinal mucosa. In addition, this process also occurs in the placental microvessels (Shukla et al., 2021). Research has been done to investigate the possible influence genetic variation in the MDR1 transporter might have on therapeutic drug levels. So, P-glycoprotein is very important in how neoplastic cells become resistant to anticancer treatments. The MDR1 gene might be able to classify this resistance.
The Importance of Drug Interactions
Preventing potential complications by checking for drug interactions is highly recommended. Your doctor and pharmacist have most likely already done this for you, but it never hurts to double-check and educate yourself on your medications (Gessner et al., 2019). Be cautious to check for drug interactions between your prescription drugs and any OTC medications, such as vitamins, herbs, or dietary supplements, that you may be taking.
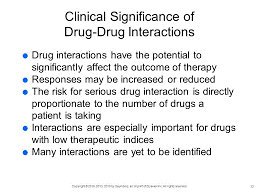
Figure 1: The Clinical Importance of Drug-Drug Interactions
If you need help deciphering medical terminology, speak with your pharmacist or physician. Because of the potential for significant harm, hospitalization, or even death from a medication interaction, drug interactions can also result in a high cost of medical treatment. Not every drug interaction is negative (Brown & Winterstein, 2019). Medications taken with food or other drugs that affect metabolic enzymes may be absorbed better or have better effects on blood levels.
How do you go about checking for drug interactions?
By communicating effectively with your healthcare professional, drug interactions can be avoided. Make sure your list of prescriptions, OTC, vitamins, herbs, and medical problems is current and accurate. You should bring this list to each appointment to share with your physician, pharmacist, and nurse. Before starting any new prescription or over-the-counter medication, read the accompanying Medication Guide, prescription data, warning labels, and Drug Factual Data Label (Maghroudi et al., 2021). New information may be added to labels as it becomes available, so it is essential to check them often.
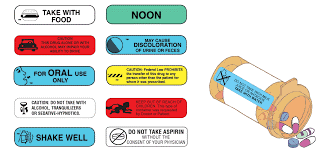
Figure 2. Prescription Drug Label
If you want the most up-to-date information about possible medication interactions, go to your doctor. To understand more about potential drug interactions, you may also use our digital drug interaction checker (Katrin et al., 2018). What the interaction is, how it happens, how serious it is (high, moderate, or low), and what you should do about it are all covered by this handy tool. Moreover, it will show you if there are any negative interactions between your selected drugs and anything you eat, drink, or have to do with your body.
The steps that I should take when I discover a drug interaction
Keep in mind that you may avoid most medication interactions by taking precautions. If you suspect you may be at risk for drug interaction, consult your doctor or pharmacist as soon as possible (Humphrey et al., 2020). They will be aware of the importance of the exchange and be able to advise you on how to proceed. It would be best if you did not stop taking your medicine without first consulting with your doctor.

Figure 3. Talk to your pharmacist to reduce Drug interaction
Drug Anaphylaxis
The mass release of mediators by basophils and mast cells causes the acute, life-threatening multi-system condition known as anaphylaxis. Recent decades appear to have seen a rise in the prevalence of anaphylaxis, even though it is typically undervalued and underfunded. Analgesics and antibiotics are the most commonly cited drugs as the causes of adverse reactions in adults (Regateiro et al., 2020). There are both immune and non-immune processes that can trigger anaphylaxis. In immunology, anaphylaxis can be mediated either by IgE-dependent or IgE-independent mechanisms. In the former, two or more distinct IgE (sIgE) antibodies on the membrane of mast cells or basophils cross-link, activating Th2 cells. IgG can mediate the IgE-independent pathway by triggering the production of platelet-activating factors and activation of the complement system. Some medications can directly stimulate mast cell degranulation, resulting in histamine release and the development of non-immunological anaphylaxis. While a clinical history is essential in investigating possible drug-induced anaphylaxis, it is not always accurate. Substantiated skin tests should be utilized instead.
Anaphylaxis symptoms
When an allergen is encountered, the onset of anaphylactic symptoms often occurs within minutes. However, anaphylaxis can sometimes manifest itself 30 minutes or more after initial contact. The onset of anaphylaxis might be delayed by several hours in highly uncommon circumstances (Christensen et al., 2019). Symptoms and signs. Exercise can aggravate skin reactions such as hives, itching, and redness or pallor of the skin, as well as conditions such as low blood pressure (hypotension) and airway constriction/swelling (leading to wheezing and difficulty breathing). Pulse that is fast and weak, diarrhoea, vomiting, nausea, and a feeling of being dizzy or falling over.
Geller (2018) suggests that quick medical responses, like the one reported by patient sixteen, represent acute hypersensitivity reactions. The hypersensitive reaction known as anaphylaxis may strike in seconds and pose a severe risk to a person’s life. Skin reactions, low blood pressure, problems breathing owing to restricted airways, difficulty breathing, unconsciousness, and tongue or throat swelling are all signs of anaphylaxis. An anaphylactic reaction is potentially fatal. According to Geller (2018), anaphylactic responses are still possible even after taking an antibiotic like amoxicillin, which is contrary to the opinions held by some of the people working with me. In this example, the sufferer had a severe allergic reaction, as shown by symptoms such as trouble breathing, wheezing, and swelling of the lips and face.
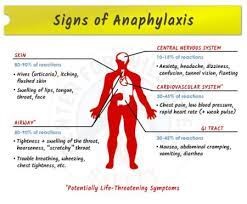
Figure 4: Signs and symptoms of anaphylaxis
Causes of Anaphylaxis
The body’s inherent defence mechanisms overreact to a trigger, causing anaphylaxis. Most likely, you have an allergy to something like this. Almonds, milk, fish, shellfish, eggs, and fruits are common allergens (Poziomkowska-Gsicka & Kurek, 2020). Medications include antibiotics and NSAIDs (such as Aspirin) for pain and inflammation. While allergy symptoms often are not life-threatening, in extreme situations, anaphylaxis may occur. Repeat exposure to the allergen that causes the mild episode of anaphylaxis carries the risk of triggering a full-blown anaphylactic reaction. Children’s most common causes of anaphylaxis are food allergies, especially to peanuts, tree nuts, fish, shellfish, wheat, soy, sesame, and milk. Adults may have anaphylactic reactions to more than only peanuts, almonds, fish, sesame, and shellfish; they can also be triggered by medications, including antibiotics, Aspirin, and other over-the-counter pain relievers, as well as intravenous (IV) contrast, which is used in several imaging procedures. Insect stings, including those from bees, yellow jackets, wasps, hornets, and fire ants. While anaphylaxis is uncommon, it may be triggered by intense exercises, such as jogging, running, or brisk walking. Some people are also more likely to get anaphylaxis if they consume certain foods before exercising or if they exercise in very hot, cold, or humid conditions. Potential anaphylactic triggers include both of these things.
Reducing the Risk of Anaphylaxis
Patients who suffer from idiopathic anaphylaxis may gain something by gaining knowledge about prevention measures. An in-depth dialogue about avoiding anaphylaxis should occur between the patient and the treating physician. There is a danger to customers’ health if they consume contaminated milk since some restaurants utilize residues of peanut, milk, or egg in their recipes. There is a significant occurrence of cross-reactions across foods, such as when someone allergic to parsley also develops intolerance to carrots, celery, and anise. This is just one example of how cross-reactions between foods may occur. Patients at a higher risk for developing anaphylaxis should be provided with in-depth information on how to self-administer epinephrine.
Only individuals with proven anaphylaxis to stinging insects should undergo allergen immunotherapy for hypersensitivity. In patients who are not too stressed, venom immunotherapy has a 90%-98% success rate in preventing reactions, and it comes with just a little risk. Important medications (including penicillin, insulin, sulfa medicines, and vancomycin) may need desensitization. Tolerance may be restored to medications including Aspirin, sulfasalazine, isoniazid, and allopurinol with a combination of continuous dosing and oral graded challenges. This kind of prophylactic treatment is quite successful. Conversely, desensitization is only effective in the short term, so if the treatment becomes essential in the future, the operation will need to be repeated.
To avoid another anaphylactic reaction, it is crucial to take precautions if you have a severe allergy or have had one in the past. One may be directed to an allergy centre for allergy tests to look for anything that might cause anaphylaxis so that one can identify any potential triggers (de Silva et al., 2020). One should exercise caution when grocery shopping and dining out if one suffers from a food allergy. Always have two working adrenaline auto-injectors on you—regardless of whether you are sure you should inject yourself if you suspect anaphylaxis.
Patients who have previously had adverse reactions to radiocontrast medicines may benefit from pharmacologic prophylaxis since it may significantly reduce the chance of repeating such reactions. Pretreatment with glucocorticosteroids and antihistamines may, in many instances, reduce the number of reactions an individual experiences (see the section on Anaphylactoid Reactions to Radiocontrast Media). The same preventative medicine could help both fluorescein-induced idiopathic anaphylaxis and fluorescein-induced anaphylactoid episodes.
Conclusion
A drug-drug interaction may change, amplify, or diminish the effectiveness of the medication. There are three pharmacological interactions: pharmacokinetic, pharmacodynamic, and physical-chemical. DDI is associated with pharmacological effectiveness and medical therapeutic potential. When drugs have opposing or complementary effects, pharmacodynamic interactions may arise. These interactions may enhance or reduce the effectiveness of another drug that acts at the same receptor site. Commonly recommended medications include cyclosporine, amiodarone, verapamil, methotrexate, and itraconazole. Drug Interaction Variables More than four prescriptions increase the likelihood of a clinically relevant drug interaction. DDIs entail the concomitant administration of two medications that may have undesirable interactions. Drugs having a low therapeutic index or narrow therapeutic range are more prone to drug interactions. Transporters are included in the pharmacokinetics of drug interactions.
Drug efflux varies owing to membrane transport variations. The ATP-dependent transporters that transport P-glycoproteins are the most extensively researched. Understanding drug interactions systematically, particularly at absorption, excretion, transport, and drug metabolism, may help reduce adverse side effects. Knowing the underlying processes of an effect is frequently necessary for predicting pharmacodynamic interactions. As rare as it may be, anaphylaxis can be fatal. The lack of cutaneous characteristics does not rule out the diagnosis, but they are the most prevalent. Drugs are the most common cause, and anti-allergic epinephrine is not always used to treat the symptoms. Every pharmaceutical interaction may be classified as either pharmacokinetic, pharmacodynamic, or physical-chemical. A drug can increase the symptoms of a medical condition you already have if you take it. Age, genetics, environment, diet, and drug clearance are some patient-related factors that can cause drug interactions (DI). Children’s most common cause of anaphylaxis is food allergies, especially peanuts, tree nuts, fish, shellfish, wheat, soy, sesame, and milk. Antibiotics and antibiotics are the most commonly cited drugs as the cause of adverse reactions in adults. Exercise can aggravate skin reactions such as hives, itching, and low blood pressure (hypotension). There is a significant occurrence of cross-reactions across foods, such as when someone allergic to parsley also develops intolerance to carrots, celery, and anise.
References
Athamneh, S. (2020). Evaluation of Potential Drug-drug Interactions among Medications Prescribed in Primary Health-Care Centers for Type 2 Diabetes Mellitus Patients: A Cross-Sectional Study From Palestine (Doctoral dissertation, جامعة النجاح الوطنية).
Bouchtout, M. N. (2022). Acknowledgment of Medicine Intercourses and Details. Farmacologia Y Toxicology, 12(3), 1–2. https://doi.org/10.36648/2174-8365.12.3.111
Brown, J. D., & Winterstein, A. G. (2019). Potential Adverse Drug Events and Drug-Drug Interactions with Medical and Consumer Cannabidiol (CBD) Use. Journal of Clinical Medicine, 8(7), 989. https://doi.org/10.3390/jcm8070989
Christensen, M. J., Eller, E., Kjaer, H. F., Broesby-Olsen, S., Mortz, C. G., & Bindslev-Jensen, C. (2019). Exercise-induced anaphylaxis: causes, consequences, and management recommendations. Expert Review of Clinical Immunology, 15(3), 265–273. https://doi.org/10.1080/1744666x.2019.1562904
de Silva, D., Singh, C., Muraro, A., Worm, M., Alviani, C., Cardona, V., DunnGlvin, A., Garvey, L. H., Riggioni, C., Angier, E., Arasi, S., Bellou, A., Beyer, K., Bijlhout, D., Bilo, M. B., Brockow, K., Fernandez‐Rivas, M., Halken, S., Jensen, B., & Khaleva, E. (2020). Diagnosing, managing and preventing anaphylaxis: Systematic review. Allergy, 76(5), 1493–1506. https://doi.org/10.1111/all.14580
Edrees, H., Amato, M. G., Wong, A., Seger, D. L., & Bates, D. W. (2020). High-priority drug-drug interaction clinical decision support overrides in a newly implemented commercial computerized provider order-entry system: override appropriateness and adverse drug events. Journal of the American Medical Informatics Association, 27(6), 893-900.
Geller, M. (2013). As múltiplas faces da anafilaxia: anafilaxia induzida por exercício e anafilaxia idiopática. Arquivos de Asma, Alergia e Imunologia, 1(1), 8-13. http://aaai-asbai.org.br/detalhe_artigo.asp?id=8
Gessner, A., König, J., & Fromm, M. F. (2019). Clinical Aspects of Transporter‐Mediated Drug-Drug Interactions. Clinical Pharmacology & Therapeutics, 105(6), 1386–1394. https://doi.org/10.1002/cpt.1360
Hughes, Y., Tomlins, L., & Usherwood, T. (2022). Prescribing for patients taking antiretroviral therapy. Australian Prescriber, 45(3), 80–87. https://doi.org/10.18773/austprescr.2022.026
Humphrey, K. E., Mirica, M., Phansalkar, S., Ozonoff, A., & Harper, M. B. (2020). Clinician Perceptions of Timing and Presentation of Drug-Drug Interaction Alerts. Applied Clinical Informatics, 11(03), 487–496. https://doi.org/10.1055/s-0040-1714276
Kastrin, A., Ferk, P., & Leskošek, B. (2018). Predicting potential drug-drug interactions on topological and semantic similarity features using statistical learning. PLOS ONE, 13(5), e0196865. https://doi.org/10.1371/journal.pone.0196865
Liu, X. (2019). Overview: Role of drug transporters in drug disposition and its clinical significance. Drug Transporters in Drug Disposition, Effects and Toxicity, 1-12.
Maghroudi, E., van Hooijdonk, C. M. J., van de Bruinhorst, H., van Dijk, L., Rademakers, J., & Borgsteede, S. D. (2021). The impact of textual elements on the comprehensibility of drug label instructions (DLIs): A systematic review. PLOS ONE, 16(5), e0250238. https://doi.org/10.1371/journal.pone.0250238
Naz, T., Akhtar, M., Shahzad, S. K., Fasli, M., Iqbal, M. W., & Naqvi, M. R. (2020). Ontology-driven advanced drug-drug interaction. Computers & Electrical Engineering, 86, 106695.
Poziomkowska-Gęsicka, I., & Kurek, M. (2020). Clinical Manifestations and Causes of Anaphylaxis. Analysis of 382 Cases from the Anaphylaxis Registry in West Pomerania Province in Poland. International Journal of Environmental Research and Public Health, 17(8). https://doi.org/10.3390/ijerph17082787
Regateiro, F. S., Marques, M. L., & Gomes, E. R. (2020). Drug-Induced Anaphylaxis: An Update on Epidemiology and Risk Factors. International Archives of Allergy and Immunology, 181(7), 481–487. https://doi.org/10.1159/000507445
Santos, T. O. D., Nascimento, M. M. G. D., Nascimento, Y. A., Oliveira, G. C. B. D., Martins, U. C. D. M., Silva, D. F. D., & Oliveira, D. R. D. (2019). Drug interactions among older adults followed up in a comprehensive medication management service at Primary Care. Einstein (São Paulo), 17.
Scheme, T. (2021). Clinical Pharmacokinetics of Metformin. In Metformin-Pharmacology and Drug Interactions. IntechOpen.
Shukla, A., Choudhury, S., Yadav, V. P., Akash, R., & Singh, S. P. (2021). Solute Carrier Transporter (SLC): A naive entity in drug development. Journal Of Veterinary Pharmacology And Toxicology, 20(1), 1-4.
Vellonen, K. S., Hellinen, L., Mannermaa, E., Ruponen, M., Urtti, A., & Kidron, H. (2018). Expression, activity and pharmacokinetic impact of ocular transporters. Advanced Drug Delivery Reviews, 126, 3-22.
Weerink, M. A. S., Barends, C. R. M., Muskiet, E. R. R., Reyntjens, K. M. E. M., Knotnerus, F. H., Oostra, M., van Bocxlaer, J. F. P., Struys, M. M. R. F., & Colin, P. J. (2019). Pharmacodynamic Interaction of Remifentanil and Dexmedetomidine on Depth of Sedation and Tolerance of Laryngoscopy. Anesthesiology, 131(5), 1004–1017. https://doi.org/10.1097/aln.0000000000002882
 write
write