Introduction
The number of diabetic people continues to increase daily, causing devastating health challenges. Millions of people in the United Kingdom are affected by diabetes, which impacts the psychological, physical and material well-being of people and their families Cole and Florez (2020, p.780). Diabetes is a lifelong illness that causes an individual’s blood sugar to become high beyond the normal level. There are two types of diabetes; type 1 diabetes and type 2 diabetes. Type 1 diabetes occurs when the immune system of the body attacks and destroys the insulin-producing cells, thus making the production of insulin difficult (Alshammari et al., 2021, p. 682). Type 2 diabetes occurs when a person’s body does not react to insulin, or the body is unable to produce sufficient insulin. It is studied that a high majority of diabetic patients in the U.K, about 90% of them, have Type 2 diabetes Behzadmehr and Rezaie-Keikhaie (2022, p.60). The socially disadvantaged communities in the U.K and those from the ethnic minority groups continue to be vulnerable to this disease. The report will explore several prevalence data that have been researched in the past years in the United Kingdom and propose new ways to help in the prevention, management and treatment.
Background
Diabetes impairs the body’s ability to process blood sugar; as noted early, there are different types of diabetes. Without careful management of this illness, it can result in a more devastating buildup which can cause dangerous complications for an affected individual (McIntyre et al., 2020, p. 167). In the United Kingdom, several adults have diabetes; the National Health Service (NHS) often offer treatment for patients living with diabetes in the U.K. It provides well-designed medical care for all patients suffering from different types of diabetes at each stage of the development of this condition. Diabetes remains a complex condition to manage NHS diabetes care also has to be complex Conor (2019, p. 1). NHS employs various staff such as nurses; online diabetes peer groups support and collaborate with multidisciplinary teams to offer better care to patients. However, many people are unaware of the NHS diabetes care in their localities. Several challenges continue to be faced in providing treatment for diabetic patients in the U.K; it is costly and costs about 10% of the NHS budget to treat diabetes. The healthcare cost could increase with the increasing number of diabetes patients yearly.
Diabetes prevalence
Public Health England (2016, p.1) established that 3.6 million people had diabetes. The prevalence was also higher for the minority ethnic groups such as the blacks and South Asians as compared to the whites at 15.2% and 8.0%, respectively Bloomgarden (2020, p. 346). Besides, the study also illustrated an increasing number of diabetic people with increasing age. Of those aged 45 to 54 years, 9.0% had diabetes, while for those aged 75 years, 23.8% were diabetic. According to DIABETES UK (2017, p. 1), in 2017, almost 3.7 million people had diabetes. Table 1 shows the prevalence of diabetes across the United Kingdom in 2016 and 2017. England represented the highest 3, 116, 399 patients followed by Scotland with 289, 040, wales with 191, 590 and Northern Ireland with 92, 480.
Table 1.
| Place | 2016 – 2017 |
| England | 3,116,399 |
| Northern Ireland | 92,480 |
| Wales | 191,590 |
| Scotland | 289,040 |
| Total | 3,689,509 |
Data from 2018 and 2019 established that about 3.9 million individuals in the U.K had diabetes, with a high majority being from England at 3.3 million people Diabetes UK (2019, p. 1). Table 2 below shows the prevalence in 2018 and 2019. England recorded 3, 319, 266, Northern Ireland with 99,833, Wales 198,883 and Scotland with 301,159.
Table 2.
| Place | 2018-19 |
| England | 3,319,266 |
| Northern Ireland | 99,833 |
| Wales | 198883 |
| Scotland | 301523 |
| Total | 3,919,505 |
The latest research on diabetes statistics between 2020 to 2022 revealed that about 4.9 million individuals in the U.K have diabetes and 8% have type 1 diabetes, and 90% suffer from Type 2 diabetes Care (2022, p. 17). Besides, around 2% of them suffer from a rarer type of diabetes. About 13.6 million individuals have a higher risk of Type 2 diabetes in the United Kingdom. Individuals with a close family member with type 2 diabetes are likely to have this type of diabetes in later years. There are also about 940 000 adults living with diabetes and have not yet been diagnosed or registered.
Over 1 in 20 people in the United Kingdom has diabetes, and about 24,000 yearly deaths in the U.K result from diabetes (Diguisto et al., 2022, p. 39). There are about 100 amputations that are carried out weekly due to the complications caused by diabetes Forouhi and Wareham (2019, p. 22). In addition, diabetes has been studied to be the leading cause of blindness among the working population in the U.K, more than 1700 individuals have their sight affected.
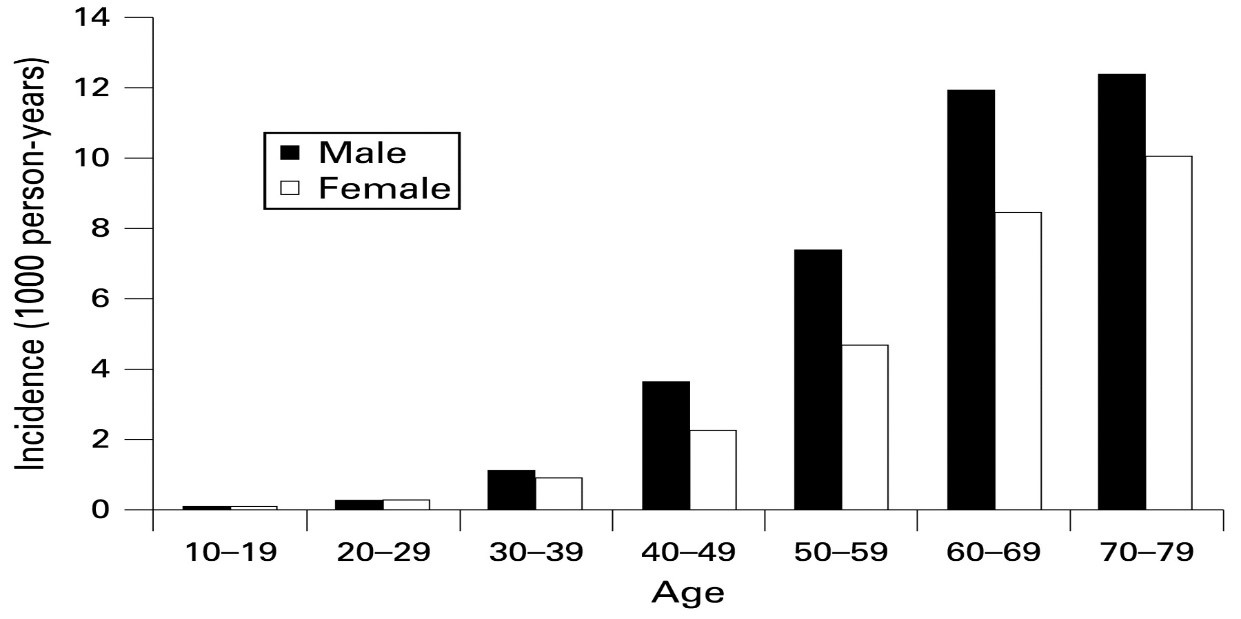
More people are at risk of type 2 diabetes, and if nothing is done, it is predicted that the U.K will have about 5.5 million people who have diabetes by 2030 (Eskenazi et al., 2022, p. 255). Older people have been studied to be the highest population affected by diabetes; as shown in figure 1 below, those between the ages of 60 to 79 with diabetes are high in number. One in 10 people 40 years of age in the U.K has been studied to be suffering from type 2 diabetes.
Figure 1.
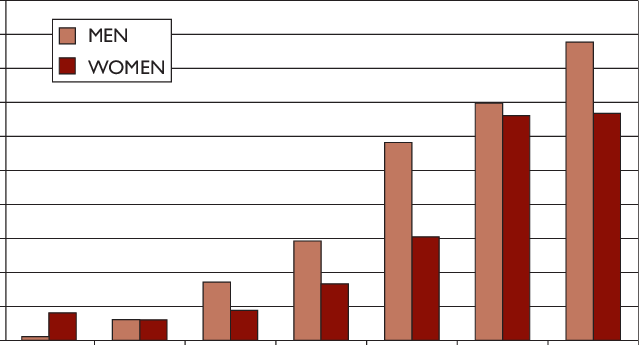
The study also revealed that a high number of individuals with diabetes are men, 9.6% and women, 7.6%. Figure 2 is a representations of diabetes prevalence between men and women, the figure shows that men represents the highest one of those affect.
Figure 2.
The causes of diabetes
Type 1 diabetes
The cause of this type of diabetes is a result of the immune system fighting and attacking insulin in the body. Various researchers have established that genes and environmental factors cause the disease, for example, viruses which trigger the disease.
Type 2 diabetes
This is the most common type of diabetes that affects many people. Some of the common causes of this type of diabetes include;
Genes and family history; Certain family history genes may make an individual likely to develop this type of diabetes (Hill-Briggs et al., 2021, p. 259). Family genes can increase a person’s tendency to be overweight, thus being at higher risk of being affected with type 2 diabetes. Individuals more highly affected are those of Black African, South Asian and African Caribbean descent.
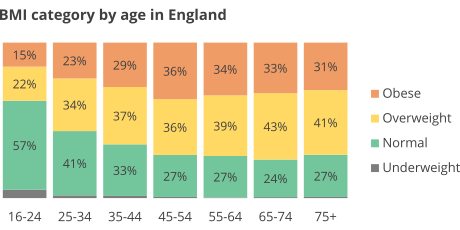
Overweight, obese and physical inactivity; Individuals who are overweight, obese and usually physically inactive are more likely to develop type 2 diabetes. It is studied that extra body weight sometimes can cause insulin resistance which is common in individuals with type 2 diabetes. In addition, extra belly fats have a higher link to insulin resistance, causing this type of diabetes. Overweight individuals are also at a higher risk of being affected by heart diseases (Jiao et al., 2022, p. 45). Three in five adults in England are obese and overweight. Besides, in England, adults who are overweight and obese are more likely to be diagnosed with diabetes than those with a normal weight. About 90% of individuals with type 2 diabetes are overweight and obese; people who are obese and overweight have a higher risk of this type of diabetes. Adults between the age of 45 to 75 years are overweight and obese in England representing a percentage of 36%, 39%, 43% and 41% of overweight. 36%, 34%, 33%, and 31% of the adults in England are obese which is a high percentage.
Figure 3.
Insulin resistance; Type 2 diabetes usually occurs due to insulin resistance, a condition whereby liver, muscle and fat cells in the body do not use insulin appropriately. Thus, the body requires more insulin to help the body cells have more glucose (McIntyre et al., 2020, p. 167). The pancreas at first makes additional insulin to help in the increased demand, but with time the pancreas cannot make more insulin, thus increasing the blood glucose in the body to increase to higher levels.
The current management and cost of diabetes in the U.K
The NHS works with Diabetes UK to manage and offer prevention programs for diabetes in the U.K. NHS has a Healthier You Program that helps identify and refer treatment to individuals at risk of diabetes. The patients are directed into a nine-month lifestyle change program. The program is offered in a face-to-face manner and through digital service care. In 2019 the Healthier You Program recorded 17,000 people who had attended the program and completed the prevention program, and they were able to lose 3.4kgs in each section NHS (2019, p.1). The program is expected to increase and double; those who will join the program will be over 200,000 patients yearly.
Diabetes is an expensive disease to manage and treat, and it is estimated that NHS spends about £10 billion yearly on diabetes NHS (2022, p. 1). The main reason for it being expensive is numerous complications associated with this condition, such as blindness, stroke, kidney failure and amputation, which require a lot of money. Table 3 shows the cost of diabetes treatment in 2012; the pounds are in billions. The inpatient represents a high percentage at 65.8%, with a total cost of £9.045 billion. Patients also spend 15.2% on non-diabetic drugs which is an expenditure on the complications associated with diabetes. A high amount of expenditure was on Type 2 diabetes at £11.718 billion.
Table 3.
| Expenditure area. | Type 1
diabetes |
Type 2
diabetes |
Total. | Percentage. |
| Diabetes drugs | £0.344 | £0.712 | £1.056 | 7.8% |
| Non-diabetes drugs | £0.281 | £1.810 | £2.091 | 15.2% |
| Inpatient | £1.007 | £8.038 | £9.045 | 65.8% |
| Outpatient (excluding drugs) | £0.170 | £1.158 | £1,328 | 9.7% |
| Other (including social service) | – | – | £0.230 | 1.7% |
| Total in billions. | £1.802 | £11.718 | £13.750 | 100% |
10% of the NHS budget is channeled to diabetes, and about 80% of the total costs are mainly for treating diabetic complications Diabetes UK (2019, p. 1). The cost is projected to grow significantly over the next 20 years to about 17% of the total NHS budget. The cost of social care will also increase for individuals who undergo amputations. Diabetes UK (2014, p. 1) projects that the cost of diabetes will be about £16.9 billion by 2035/ 2036 with the assumption that there is no inflation in the U.K.
General changes in the management, prevention, and treatment of diabetes
Lifestyle behavioural changes play a big role in managing and preventing diabetes-related complications Forouhi and Wareham (2019, p.25). The following are important changes that need to be implemented to help manage and treat diabetes in the United Kingdom.
Improving population health.
Focusing on improving the population’s health can play a major role in having better health outcomes for people (Kanumilli et al., 2021, p 35). The care delivery systems need to be appropriate, thus ensuring that diabetes treatment decisions are timely through relying on evidence-based guidelines and the inclusion of community-based support care. All diabetes care management approaches must be aligned to emphasize person-centred team care and incorporate long-term care plans. All teams involved in the collaborative care plan must have an effective communication plan for all members to help facilitate a team-based care system through appropriate decision support tools (Ikomi and Mannan (2022, p. 36). Goal-based behavioural interventions have to be implemented to help in lifestyle changes to improve the population’s health. The following methods can be used in achieving lifestyle changes;
Physical activity goal; Physical activity can play a big role in keeping a person physically active and healthy. People who remain physically inactive are at a high risk of being overweight and obese (McIntyre et al., 2020, p. 167). Participation in various core curriculum activities can help in lifestyle changes. Physical activities such as walking, playing football, riding a bicycle and jogging and playing for about 150 minutes daily can be of significance to the health of a person and can reduce cases of diabetes. People must be encouraged to have a weekly plan of their daily physical activity spread across the week; this can help burn excess calories and keep a person healthy.
Weight loss goal; Encouraging people to have weight management programs can play an important role in promoting health outcomes for the population. Individuals at a high risk of being overweight and obese need to implement the right programs to manage their weight (Ryan et al., 2022, p. 296). Aiming at losing about 0.5 to 1 kg weekly and burning about 500 to 1000 calories have to be the main goals for individuals who are mostly used to living a sedentary lifestyle Tschiedel and Puñales (2022, p.346). Physical activities can play a huge role in long-term weight loss maintenance. Individuals who are overweight and obese have been studied to have increased chances of suffering from diabetes; therefore, necessary to have better weight management to have better health outcomes for the population.
Dietary modification; Unhealthy fats such as chips, fries, and baked foods have high fats and, if taken by a diabetic person, can worsen the condition. People should be encouraged to have modified dietary plans that are healthy (Sun et al., 2022, p. 10). Diabetic individuals must be informed of the appropriate food type and a quality diet to manage their conditions. Nutritional recommendations for diabetic individuals need to be fully focused on to avoid complications that come with diabetes.
Improvement of diabetes technology.
With the continued changes in technology, it is necessary to have more modified diabetes technologies to help diabetic patients to manage their conditions. Improvement in technology includes changes in syringes used in administering insulin and devices used in blood glucose monitoring (Leon et al., 2021, p. 13). Individuals with diabetes need to be assisted with this device, and it should be done from the onset of diagnosis of diabetes Sartorius (2022, p.25). When issuing this device, it should be individualized according to the needs and preferences of each patient. During device prescriptions, it is also necessary that the caregivers receive adequate training on how to use the diabetes technological devices appropriately. Educating patients on properly using diabetes devices can help achieve a better outcome. The need for additional education on the use of the device has to be periodically assessed to help patients manage diabetes better.
Classification and diagnosis of diabetes.
Proper diagnosis and classification need to be keenly done by a professional healthcare to avoid misdiagnosis instances (Whicher et al., 2020, p. 245). The type of diabetes the patient suffers from needs to be clearly stated for appropriate condition measures to be fully implemented. The screening should follow all the necessary steps to avoid mistakes. Also, people must be taught about the symptoms of diabetes and be informed about the importance of early detection to help in early treatment and monitoring.
Diabetes Advocacy
Managing the complications that come with diabetes can be a challenging task for any patient. All patients with diabetes should not be subjected to discrimination, but they must be properly cared for in society (Zhuo et al., 2022, p. 36). Implementing advocacy for the rights of diabetic patients in society will help the patients live healthy and productive life. The advocacy programs must be implemented at workplaces, schools, and care and correction institutions.
Address insulin access and affordability.
Insulin is necessary for patients with diabetes, and it is necessary for various stakeholders in the insulin supply chain to avail in an affordable amount. The high cost of insulin makes patients of low social income have difficulty accessing the commodity, thus having difficulty in having appropriate ways to manage their conditions (Wang et al.,.2020, p. 84). Proper procedures and guidelines need to be implemented by healthcare policymakers to help in ensuring that there is enough and affordable insulin for diabetic patients who require it.
Conclusion
Diabetes continues to be a serious lifestyle disease affecting millions of people in the United Kingdom. Several people are diagnosed yearly with this condition; the prevalence data shows the U.K experiences an increase of diabetic patients by over one hundred thousand individuals yearly. Type 2 diabetes has been studied to affect many people, with 90% of diabetic patients suffering from it. The cause of diabetes involves several factors: insulin resistance, genes and family history and overweight, obesity and physical inactivity. This report establishes that most adults aged 45 to 75 years are overweight and obese; thus, many have diabetes in the United Kingdom. The cost of treating diabetes continues to be expensive. Most patients from low social and economic groups and minority ethnic communities are highly impacted since they cannot afford the cost of treatment. The high cost is due to the complication that comes with diabetes. There needs to be the implementation of appropriate changes such as improving population health, improved diabetes technology, and appropriate classification and diagnosis. Also, diabetes advocacy needs to be done, and stakeholders must address insulin’s affordability.
Recommendations and implications for practice
The following recommendations need to be fully implemented by policymakers in the health sector to help manage and treat diabetes in the United Kingdom.
- Continuous research must be done to ensure that there is available data on the number of patients living with diabetes to help properly plan how to help them.
- Adequate systems must be implemented to ensure that all adults with diabetes are properly monitored to help them manage the lifelong complications that come with diabetes.
- Local guidelines must be reviewed to help individuals with long-term diabetes complications.
- The cost of treatment of diabetes needs to be made affordable to all people to enable those from low social income and minority ethnic communities to receive adequate care.
- Diabetic patients who develop other complications, such as cardiovascular diseases, must be properly cared for.
- People living with diabetes must be involved in decision-making about diabetes care decisions.
- Proper nutritional guidelines should be provided consistently for patients who have diabetes to avoid further complications due to the wrong dietary plan.
- People must be taught the importance of early screening when they suspect a diabetic condition; this will help better manage the disease.
- Diabetic specialist nurses have to be employed to help in overseeing and surveillance of diabetic patients.
- Patients must be educated on the right ways to manage their diabetic conditions and exercise appropriate self-care programs.
- A diabetes liaison team needs to be implemented in places with a high number of diabetic patients; this ensures a team-based approach to managing the disease.
A combination of improving the population’s health through dietary modification, physical activity, and weight loss are essential in managing diabetes and are significant evidence-based models for managing diabetes. The following are analyses of the clinical implications for nursing practice.
Staff shortages.
The number of diabetic patients is projected to increase over the years; this will pose a challenge in implementing diabetes nursing care. If an adequate number of clinicians are not employed, it will be challenging to implement care changes to help diabetic patients in the U.K.
High patient ratios.
As noted in the report, the number of patients is anticipated to increase to over 5.5 million by 2030. This concern must be examined as it will make it difficult for the NHS to offer adequate care to diabetic patients. The care programs need to be modified to involve the community and family members to help provide care to boost the proper care of patients.
Financials problems.
Diabetes treatment is expensive and requires capital to help finance various diabetes care programs. With the increasing number of patients, the healthcare systems will therefore have to increase their expenditures in offering treatment to patients. The government and various charity organisations have to channel funds specifically meant for sponsoring nursing programs for diabetes patients.
References
Alshammari, M., Windle, R., Bowskill, D. and Adams, G., 2021. The role of nurses in diabetes care: a qualitative study. Open Journal of Nursing, 11(8), pp.682-695.
Agarwal, M.M., 2018. Consensus in gestational diabetes mellitus: looking for the holy grail. Journal of clinical medicine, 7(6), p.123.
Bhaskar, S., Rastogi, A., Chattu, V.K., Adisesh, A., Thomas, P., Alvarado, N., Riahi, A.D., Varun, C.N., Pai, A.R., Barsam, S. and Walker, A.H., 2020. Key strategies for clinical management and improvement of healthcare services for cardiovascular disease and diabetes patients in the coronavirus (COVID-19) settings: recommendations from the REPROGRAM consortium. Frontiers in cardiovascular medicine, 7, p.112.
Behzadmehr, R. and Rezaie-Keikhaie, K., 2022. Evaluation of active pulmonary tuberculosis among women with diabetes. Cellular, Molecular and Biomedical Reports, 2(1), pp.56-63.
Bloomgarden, Z.T., 2020. Diabetes and COVID‐19. Journal of Diabetes, 12(4), pp.347-348.
Cole, J.B. and Florez, J.C., 2020. Genetics of diabetes mellitus and diabetes complications. Nature reviews nephrology, 16(7), pp.377-390.
Care, D., 2022. Care in Diabetes—2022. Diabetes Care, 45, p. S17.
Conor S., 2019. NHS and Diabetes. https://www.diabetes.co.uk/nhs/
Diguisto, C., Strachan, M.W., Churchill, D., Ayman, G. and Knight, M., 2022. A study of diabetic ketoacidosis in the pregnant population in the United Kingdom: Investigating the incidence, aetiology, management and outcomes. Diabetic Medicine, 39(4), p.e14743.
Diabetes UK., 2017. Diabetes prevalence 2017 (november 2017). https://www.diabetes.org.uk/professionals/position-statements-reports/statistics/diabetes-prevalence-2017
Diabetes UK., 2019. Cost of Diabetes. https://www.diabetes.co.uk/cost-of-diabetes.html
Eskenazi, B., Rauch, S., Iurlaro, E., Gunier, R.B., Rego, A., Gravett, M.G., Cavoretto, P.I., Deruelle, P., García-May, P.K., Mhatre, M. and Usman, M.A., 2022. Diabetes mellitus, maternal adiposity, and insulin-dependent gestational diabetes are associated with COVID-19 in pregnancy: the INTERCOVID study. American Journal of Obstetrics and Gynecology, 227(1), pp.74-e1.
Forouhi, N.G. and Wareham, N.J., 2019. Epidemiology of diabetes. Medicine, 47(1), pp.22-27.
Hill-Briggs, F., Adler, N.E., Berkowitz, S.A., Chin, M.H., Gary-Webb, T.L., Navas-Acien, A., Thornton, P.L. and Haire-Joshu, D., 2021. Social determinants of health and diabetes: a scientific review. Diabetes care, 44(1), pp.258-279.
Ikomi, A. and Mannan, S., 2022. The GooD Pregnancy Network: An Alternative Approach for Gestational Diabetes. BioMed, 2(1), pp.37-49.
Jiao, T., Platt, R.W., Douros, A. and Filion, K.B., 2022. Prescription patterns for the use of antihypertensive drugs for primary prevention among patients with hypertension in the United Kingdom. American Journal of Hypertension, 35(1), pp.42-53.
Kanumilli, N., Brunton, S., Cos, X., Deed, G., Kushner, P., Lin, P. and Nolte, J., 2021. Global survey investigating causes of treatment inertia in type 2 diabetes cardiorenal risk management. Journal of Diabetes and its Complications, 35(3), p.107813.
Klein, S., Gastaldelli, A., Yki-Järvinen, H. and Scherer, P.E., 2022. Why does obesity cause diabetes?. Cell metabolism, 34(1), pp.11-20.
Leon, N., Namadingo, H., Bobrow, K., Cooper, S., Crampin, A., Pauly, B., Levitt, N. and Farmer, A., 2021. Intervention development of a brief messaging intervention for a randomised controlled trial to improve diabetes treatment adherence in sub-Saharan Africa. BMC Public Health, 21(1), pp.1-14.
Lahoz, R., Fagan, A., McSharry, M., Proudfoot, C., Corda, S. and Studer, R., 2022. Recurrent heart failure hospitalizations increase the risk of mortality in heart failure patients with atrial fibrillation and type 2 diabetes mellitus in the United Kingdom: a retrospective analysis of Clinical Practice Research Datalink database. BMC Cardiovascular Disorders, 22(1), pp.1-11.
McIntyre, H.D., Gibbons, K.S., Ma, R.C., Tam, W.H., Sacks, D.A., Lowe, J., Madsen, L.R. and Catalano, P.M., 2020. Testing for gestational diabetes during the COVID-19 pandemic. An evaluation of proposed protocols for the United Kingdom, Canada and Australia. diabetes research and clinical practice, 167, p.108353.
NHS.,2022. NHS Prevention Programme cuts chances of Type 2 diabetes for thousands. https://www.england.nhs.uk/2022/03/nhs-prevention-programme-cuts-chances-of-type-2-diabetes-for-thousands/#:~:text=Evidence%20has%20shown%20that%20the,effective%20in%20the%20long%2Dterm.
NHS., 2019. NHS Diabetes Prevention Programme (NHS DPP). https://www.england.nhs.uk/diabetes/diabetes-prevention/
Nouhjah, S., Jahanfar, S. and Shahbazian, H., 2020. Temporary changes in clinical guidelines of gestational diabetes screening and management during COVID-19 outbreak: A narrative review. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 14(5), pp.939-942.
Ncube, N., Kulinskaya, E., Steel, N. and Pchejetski, D., 2022. On the survival of individuals diagnosed with type 2 diabetes mellitus in the United Kingdom: a retrospective matched cohort study. Diabetes Epidemiology and Management, 6, p.100065.
Public Health England, (2016). Diabetes Prevalence Model. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/612306/Diabetesprevalencemodelbriefing.pdf
Reifsnider, O., Kansal, A., Pimple, P., Aponte‐Ribero, V., Brand, S. and Shetty, S., 2021. Cost‐effectiveness analysis of empagliflozin versus sitagliptin as second‐line therapy for treatment in patients with type 2 diabetes in the United States. Diabetes, Obesity and Metabolism, 23(3), pp.791-799.
Ryan, D.K., Haddow, L., Ramaesh, A., Kelly, R., Johns, E.C., Denison, F.C., Dover, A.R. and Reynolds, R.M., 2018. Early screening and treatment of gestational diabetes in high-risk women improves maternal and neonatal outcomes: A retrospective clinical audit. Diabetes research and clinical practice, 144, pp.294-301.
Rajput, S.A., Ashraff, S. and Siddiqui, M., 2022. Diet and Management of Type II Diabetes Mellitus in the United Kingdom: A Narrative Review. Diabetology, 3(1), pp.72-78.
Roberts, S.P., Brown, S.J. and Roberts, S.H., 2021. Women’s engagement, views and experiences of postnatal follow-up after gestational diabetes mellitus in pregnancy. Midwifery, 101, p.103043.
Tschiedel, B. and Puñales, M., 2022. Insulin Therapy. In Endocrinology and Diabetes (pp. 345-353). Springer, Cham.
Sun, S., Mao, Z. and Wang, H., 2022. Relationship between periodontitis and diabetes: a bibliometrics analysis. Annals of Translational Medicine, 10(7).
Sartorius, N., 2022. Depression and diabetes. Dialogues in clinical neuroscience.
Teare, H., Argente, J., Dattani, M., Leger, J., Maghnie, M., Sherlock, M., Ali, G.C., Francombe, J. and Marjanovic, S., 2022. Challenges and improvement needs in the care of patients with central diabetes insipidus. Orphanet journal of rare diseases, 17(1), pp.1-12.
Velardo, C., Clifton, D., Hamblin, S., Khan, R., Tarassenko, L. and Mackillop, L., 2021. Toward a multivariate prediction model of pharmacological treatment for women With gestational diabetes mellitus: algorithm development and validation. Journal of medical Internet research, 23(3), p.e21435.
Wang, Y., Min, J., Khuri, J., Xue, H., Xie, B., Kaminsky, L.A. and Cheskin, L.J., 2020. Effectiveness of mobile health interventions on diabetes and obesity treatment and management: systematic review of systematic reviews. JMIR mHealth and uHealth, 8(4), p.e15400.
Whicher, C.A., O’Neill, S. and Holt, R.G., 2020. Diabetes in the UK: 2019. Diabetic Medicine, 37(2), pp.242-247.
Wilding, J., Godec, T., Khunti, K., Pocock, S., Fox, R., Smeeth, L., Clauson, P., Fenici, P., Hammar, N. and Medina, J., 2018. Changes in HbA1c and weight, and treatment persistence, over the 18 months following initiation of second-line therapy in patients with type 2 diabetes: results from the United Kingdom Clinical Practice Research Datalink. BMC medicine, 16(1), pp.1-12.
Zhuo, X., Cohen, C.M., Chen, J., Chodick, G., Alsumali, A. and Cook, J., 2022. Validating the UK prospective diabetes study outcome model 2 using data of 94,946 Israeli patients with type 2 diabetes. Journal of Diabetes and its Complications, 36(1), p.108086.
 write
write