Abstract
Metabolic Bone Disease fundamentally refers to the disparate umbrella of diversified complications resulting from abnormalities in bone cell physiology or calcium metabolism. Consequently, the result causes an alteration in serum calcium concentration or an eventual skeletal failure. Various elements such as phosphorus, calcium, vitamin D, and magnesium are useful in forming human bones. The lack of enough minerals causes metabolic bone diseases. Some of the metabolic bone diseases include Osteomalacia, tumor-induced Osteomalacia, Osteopenia, Osteoporosis, Osteogenesis Imperfecta, Paget’s disease, and melorheostosis. In developed countries, Osteoporosis is one of the most common metabolic bone diseases, which affects mainly the elderly. The prevalence of Osteoporosis is on a steady rise as the number of elderly populations in developed countries increases. Metabolic bone diseases are characterized by various signs and symptoms, including chronic and muscular pain, weight loss, and neurological problems. Various methods are used for diagnosing and treating different metabolic bone diseases. Some of the main methods used in diagnosing metabolic bone diseases include radiograph and X-ray tests, MR and CT scans, and laboratory tests.
Common Metabolic Bone Diseases
Introduction
Metabolic Bone Diseases (MBD) encompasses a widened spectrum of clinically diverse diseases that have standard foundations in terms of bone chemical compositions and formulations that ultimately lead to skeletal and born defects and abnormalities. Most characteristics exhibited by these bone diseases are commonly reversible and can be clinically treated. Minerals such as phosphorus, calcium, vitamin D, and magnesium are common causatives of these abnormalities and result in malfunctions. Minerals are fundamental because they are the key controllers of mineral homeostasis. As a result of insufficient minerals, various bone diseases such as Osteomalacia, tumor-induced Osteomalacia, Osteopenia, Osteoporosis, Osteogenesis Imperfecta, Paget’s disease, and melorheostosis.
Different types of bone diseases
Osteopenia
Osteopenia is a bone infection depicted by body mass reduction, which causes economic and social burdens. Osteopenia enhances increased chances of having a fracture and bone fragility. Osteopenia is caused by various factors, including smoking, eating disorders, excess consumption of alcohol, lack of physical activity, and calcium and vitamin D deficiency [7]. Women are the most affected by Osteopenia due to increased estrogen hormone levels. Small-boned Caucasians and Asians have a higher risk of developing Osteopenia. A past family history of the bone disease also puts one at the chance of being affected by Osteopenia [7]. Chronic inflammatory diseases also increase the risk of having Osteopenia due to weak bones. Osteopenia develops into Osteoporosis when it is not treated accordingly.
Osteoporosis
In highlight, Osteoporosis primarily develops when bone mass and mineral density decrease or when bone quality or structure is altered. This leads to bone weakening or decline in bone strength, predisposing the individual to fracture risks [4]. Orthopedic practitioners claim that Osteoporosis does not show significant symptoms; hence, a person is less likely to know if they have the disease unless they break a bone. Furthermore, this disease is identified to cause most bone fractures in women and older males. The mainly affected parts of the body are the hips, wrists, and spine.
Osteomalacia
Osteomalacia is depicted by softening of bones where its core causative element is a lack of vitamin D. Osteomalacia occurs in children and adults. The softening of bones may lead to gradual bowing as an individual grows, especially on the leg area and other weight-bearing bones [6]. Older adults suffering from the illness are likely to have bone fractures, while those children born with or developing the complication in infancy develop fuzzy skulls and brittle bones.
In its initial stages, Osteomalacia might not show any severe symptoms but can be detected through X-ray scans and other compatible diagnostic methodologies and tests. Clinical features of the disease are equally similar across most patients. Common features are muscles weaknesses and pain in the bone. Patients suffering from the diseases often complain of generalized mild bone pains that become adverse during bedtime. The pains are typically associated with bone tenderness [6]. Notably, the bone pains have been clinically attributed to rheumatoid arthritis and osteoarthritis, which may lead to late detection of the disease. Muscle weaknesses are most common in the pelvis region, making the patient have difficulties climbing stairs or getting out of their bed without the physical support of the forelimbs. The muscles are weak, although there is no neurological sign of actual damage. Cumulatively, these signs and symptoms cause slowness in walking and mobility difficulties.
Paget’s Disease
Paget’s disease, also called osteitis deformans or Paget’s disease (PDB) of the bone, is a slowly progressing chronic bone condition that causes rapid bone destruction and reformation (osteoblastic). A typical bone is formed through the remodeling process and replaces the older or worn-out parts of the bone with new and stronger bones [1]. Paget’s disease alters the process of bone remodeling and formation, making the holistic approach shift out of balance, thus causing an abnormality in the new bone. The abnormalities can occur in different body parts, leading to deformities and osseous abnormalities.
Historically, the disease’s evidence dates to the neolithic era. Today, it is prevalent in most parts of the world, mainly the UK, Australia, North America, New Zealand, and France [1]. The complication is less common in Norway, Sweden, Finland, Iceland, Japan, China, and Africa. In the United States, more prevalence is noted in the northern parts, and New York demonstrates higher occurrences closely similar to that of the UK. A key highlight of the disease is that it mainly affects people from the country than those in urban areas. In rare occurrences, the disease appears before the age of 40 [1]. Moreover, most patients diagnosed with Paget’s disease admit various histories of their families being affected by the infection.
PDB is predominantly an asymptomatic disease. However, symptomatic patients usually manifest deep bone pains that are persistent during the daytime and get adverse at night. In most cases, the condition is monostotic (involving a single bone), and at times it may involve several bones (polyostotic) [1]. After a bone is affected, growth does not proceed. While all bones in the skeleton can be affected, some bones such as the sacrum and pelvis, spine, humeri, thigh bones, tibias, and the skull stand higher chances of impact. Facial bones, hands, and feet are the least affected bones in the skeleton. Pain mainly emanates from bone deformations that include skull enlargements, increased skin temperatures around the affected regions, and bending of long bones. The appearance of Paget’s disease is shown in figure 3 [1].
Melorheostosis
Melorheostosis is a peculiar and rare disease of bones that causes new abnormal growth of tissues around the already existing bones. Melorheostosis is depicted when a new bone is viewed through an X-ray scan. Unique formations in the forms of “flowing” or dripping candle wax-like structures characterize melorheostosis [5]. Most excess bone growths are found around arms and leg bones and rarely on the sternum, ribs, and pelvis, although these bones can be affected. The abnormalities exhibit non-cancerous properties, which do not spread from one bone to another.
Early signs and symptoms of Melorheostosis usually emerge during childhood and puberty. The signs and symptoms include chronic pain, limiting an individual’s body motion and flexibility, and causing permanent joint and bone deformities [5]. Some people may show symptoms such as thickened swellings and reddening of the skin around the affected area.
The disease affects about one person in a population of 1 million. So far, close to 400 cases have been reported [5]. Estimations show that half of Melorheostosis cases are caused by the mutation in the MAP2K1 gene. The MAP2K1 coordinates the production of protein Kinase MEK1, which is available in various types of cells, including bone cells. MEK1 kinase plays a significant role in the signaling pathways facilitating cell division and development. In essence, the RAS signaling is essential in the normative cellular division and growth and the formation of bones. Such gene mutations occur in bone cells leading to the production of a version of MEK1 protein kinase that has an overreactive nature that causes RAS/MAPK induced signals in the bones. The increased signaling in the bone cells causes abnormal growth in existing bones. Eventually, the process leads to overdevelopment of the bone that causes compression and damage to the nerves causing pain, muscles weakness, and in fewer instances, hearing complications.
Tumor-induced Osteomalacia
Tumour-induced Osteomalacia (TIO) is one of the rare bone diseases whose clinical presentations/ features include bone pains, fractures, muscular pains, and minimal height and weight loss cases. The identified medical cause of the disease is high concentrations of phosphates, vitamin D- regulating hormones, and FGF23 in blood [3]. FGF23 secretions from the mesenchymal tumors are normally harmless, less aggressive, and small in size, hence challenging to locate. FGF23 mainly function in the renal tubes where they impair absorption of phosphates and some forms of vitamins D, a state that leads to hypophosphatemia and decreased 1,25-dihydroxy vitamin D levels. The combination of these activities leads to improper bone metabolism. The disease’s prevalence is yet to be accounted for. Most literature on TIO reveals that since the relationships between tumors and reabsorption of phosphates were made, a little above 300 cases of the disease have been recorded. Tumour-induced Osteomalacia is shown in figure 1 [3].
Osteogenesis Imperfecta
Osteogenesis Imperfecta (OI), also popularly identified as brittle bone disease, is a more common heritable complication affecting the connective tissue. This group of genetic disorders centrally affects bones. People suffering from this condition can easily break their bones. Severe cases of these complications occur especially before a child is born, and common milder cases entail few or multiple fractures throughout a person’s lifetime [8]. For early detection of bone disease, health care practitioners usually conduct ultrasounds when a mother is pregnant. More than 19 forms of Osteogenesis Imperfecta are clinically recognized and designated as type 1 through type XIX. The different types of complications are commonly identifiable via their signs and symptoms. However, some signs and symptoms between the types might overlap. Including type 1, milder forms of the complications bear features such as bone fractures, especially during childhood and adolescence. Similar fractures are minimal as an individual graduates to adulthood. Additional features of Osteogenesis Imperfecta are a blue or gray tint patch on the sclera. Figure 2 shows a radiograph of an infant diagnosed with Osteogenesis Imperfecta [8].
In adults, Osteogenesis Imperfecta is mainly characterized by bone weakness and easy bone breakage. The fragility of their bones may or not originate from minor injuries during childhood. The bone fragility renders an adult individual at risk of breaking bones, especially when older than 40 years of age [8]. Another notable characteristic of this disease is the genetic defection that alters with the production of Type 1 collagen that facilitates collective tissues such as tendons, skin, and ligaments [8]. Due to the genetic defection, individuals are predicted to develop lower bone and mineral density. Other secondary features of Adult Osteogenesis Imperfecta may include dentinogenesis imperfecta, height loss, and even hearing loss. The condition affects individuals at a ratio of 1:10,000-20,000 globally. Up to 25000 to approximately 50000 people live with this condition.
Discussion
Bones are among the essential endoskeleton compositions and metabolically sensitive organs whose roles entail storing minerals, producing proteins, and catabolizing proteins under specific enzymes and hormones. The bone is responsible for producing the Fibroblast Growth Factor 23 (FGF 23), which plays a massive role in mineral metabolism. When mineral metabolism is dysregulated, it may lead to a range of skeletal complications mainly characterized by joint pains and internal discomfort, bone fragilities and fractures, and death. The most common metabolic bone diseases are Osteoporosis, Osteomalacia, and Osteopenia. However, some uncommon diseases are Melorheostosis, Paget Disease of the bone, Tumor-induced Osteomalacia, Osteogenesis Imperfecta, and many others. The prevalence of the various metabolic bone diseases is shown in table 1.
Analysis and Diagnosis of the Various Bone Diseases
Osteoporosis
Osteoporosis is mainly prevalent in the most developed nations. Osteoporosis mainly affects older women more than men. There are two clinically identified forms of the complication: primary and secondary Osteoporosis. Further categorization of the primary Osteoporosis presents Type I and type II. Type I Osteoporosis often affects older women above the age of 50 -65 4. Osteoporosis’s radiological and clinical features are closely related to other bone diseases. However, the process of formation might be different.
Diagnosis and Treatment
Radiology is one of the methods used in the diagnosis of Osteoporosis. Despite the modern technological advances in radiology, conventional radiology is still the most preferred radiology method. One main disadvantage of this method is that it only detects changes after approximately 30% of the bone is demineralized [4]. Some bones are more likely to be affected than others due to more expansive surfaces and proportions of the trabecular bone. Therefore, conventional radiography identifies that such changes are more common in the axial skeleton and at the ends of the trabecular bones of the juxta-articular appendicular skeleton. Other commonly affected bones are those in the hips, wrists, and spine. Other methods to detect bone complications include quantitative ultrasounds, the DEXA, quantitative CT scans, and micro-CT.
The forms of treatments available for Osteoporosis primarily address the elements of bone reformations. The most recent available osteoporosis treatments deter bone resorption. Increased resorption has been clinically identified as the primary mechanism that causes postmenopausal Osteoporosis [4]. Reversal and deterrence of the resorption process majorly entail clinical use of Bisphosphonates. Common antiresorptive agents include estrogen, denosumab, and calcitonin. However, due to the coupled nature of bone remodeling, antiresorptive methods in treatment may cause suppression in bone formation. Importantly, the most inexpensive and effective treatment method for Osteoporosis is encouraging patients to participate in weight lifting activities and increase their intake of vitamin D and calcium.
Osteopenia
Osteopenia primarily results from low bone density. Osteopenia differs from Osteoporosis in that bones do not easily break. Practitioners do not consider Osteopenia as an actual clinical disease but as a marker of probable fractures or the onset of Osteoporosis [7]. The older population is the most affected population where they stand at risk of developing unrecognized Osteoporosis, which may be diagnosed if one breaks a bone. Common risk factors of complication other than bones density include age (probability of breaking a bone increase with age), smoking, alcohols consumption, and racial disparities where white women are more likely to fracture than black and Hispanic elder women. When women are beyond menopause, they naturally start experiencing lower bone density due to the low estrogen levels. When they lose much bone mass, they are likely to develop Osteopenia.
Diagnosis and Treatment
Early detection of Osteopenia is a significant stage in preventing its adversity. Therefore, women that are past menopause stages should attend regular checkups to measure their Bone Mineral Density (BMD). DEXA is the commonly used method to determine the mineral composition of a bone [7]. However, it is mainly disadvantaged by the accuracy and precision of the results in specific bones. Similar to Osteoporosis, DEXA in this context deploys T-scores for various sets of densitometric readings of different age groups. According to WHO, a T-score of approximately -1.0 to -2.5 is regarded as a decrease in BMD [7]. Medical practitioners recommend that follow-up measures should be done throughout two to three years, especially for those females that lose 1-2% of bone density yearly [7]. Physical examination is another crucial consideration during the diagnosis of the condition. Common elements of consideration include height and weight to examine body mass index (BMI). Other physical aspects are checking for flexibility of joints, especially the fingers and feet, proximal muscle wastage, and skin elasticity.
Paget’s Disease
Paget’s disease may involve single or multiple bones. Paget’s disease symptoms include pain and deformity in the bones, arthritis, and neurological problems. Some neurological problems include hearing loss, headache, and peripheral neuropathies [1]. The spread of Paget’s disease increases with increase in age. However, the spread of Paget’s disease differs in various ethnic groups, with the infection being rare in China, African blacks, and Japan.
Diagnosis and Treatment
A blood test for alkaline phosphate is the primary diagnosis of Paget’s disease. Other tests include bone x-rays that are conducted by doctors to diagnose Paget’s disease [1]. In bone X-rays, the bones look damaged and thick. On the other hand, in blood and urine tests, other tests such as MRI and CT scans are needed if the alkaline phosphate enzyme level is found to be high [1]. Radiograph tests are also used to diagnose Paget’s disease, which is performed mainly in symptomatic patients.
Tumor-induced Osteomalacia
Tumour-induced Osteomalacia is characterized by muscular and bone pains, height, and weight loss. High concentrations of phosphates, Vitamin-D regulates hormones, and FGD23 in the blood cause tumor-induced Osteomalacia [2]. When tumor-induced Osteomalacia occurs before growth plate closure, rickets is caused. The symptoms and signs of tumor-induced Osteomalacia are associated with other infections such as prostate and cell cancer.
Diagnosis and Treatment
Laboratory tests, patient history, physical examination, and imaging are used to diagnose tumor-induced Osteomalacia. The laboratory tests include various measurements of serum FGF23 levels and serum phosphorus [2]. Patient history is used to evaluate the presence of hypophosphatemia, which helps establish the diagnosis of tumor-induced Osteomalacia. On the other hand, imaging is used to confirm tumor-induced Osteomalacia presence [2]. After diagnosis, tumor-induced Osteomalacia is then treated through surgical resection. The treatment is the most reasonable approach as it helps relieve pain and other symptoms associated with tumor-induced Osteomalacia.
Osteogenesis Imperfecta
Osteogenesis Imperfecta is a bone disease that affects the connective tissue, which may lead to bone breakage. Mutations of genes cause osteogenesis Imperfecta. The severe cases of Osteogenesis Imperfecta occur before a child is born, and it entails fractures throughout one’s life. More than 19 forms of Osteogenesis Imperfecta are designed as type 1 [8]. However, different forms of complications due to Osteogenesis Imperfecta are identified via their signs and symptoms. The risk of bone breakage due to Osteogenesis Imperfecta is high for individuals of 40 years and above.
Diagnosis and Treatment
Genetic testing is the most used method of diagnosing Osteogenesis Imperfecta. Conduction of Ultrasounds in pregnant women is another method of diagnosing Osteogenesis Imperfecta in children. Genetic testing includes biochemical testing or DNA sequencing [8]. When Osteogenesis Imperfecta is present in an individual, surgery is done, and protective devices are used to stabilize the broken bones. In children, rodding surgery is mainly done to treat Osteogenesis Imperfecta.
Melorheostosis
Melorheostosis usually affects children in the childhood and puberty stages. Melorheostosis causes chronic pain, limiting an individual’s body motion, flexibility, and bone deformities. Other symptoms of Melorheostosis include thickening, swelling, and reddening of the skin around the affected area [5]. Melorheostosis is caused by the mutations in the MAP2K1 gene, which is responsible for the production of protein Kinase MEK1 responsible for facilitating cell division and development [5]. As a result of MAP2K1 gene mutation, the bones are compressed and eventually damage nerves, leading to Melorheostosis. X-ray imaging tool is the primary method of diagnosing Melorheostosis, after which pain is received through various management programs.
Conclusion
Various elements such as phosphorus, calcium, vitamin D, and magnesium are essential in forming bones in the human body. However, lack of enough features results in abnormalities of the bones, a condition referred to as Metabolic Bone Disease. As a result of the bone abnormalities, various complications are caused. Some metabolic diseases include Osteomalacia, tumor-induced Osteomalacia, Osteopenia, Osteoporosis, Osteogenesis Imperfecta, Paget’s disease, and melorheostosis. Various methods such as X-ray tests are used to diagnose different metabolic bone diseases. As discussed in this report, the diseases are also characterized by various signs and symptoms.
Acknowledgement
I would like to thank the Almighty God for successfully enabling me to finish this project. Thanks to my professor and librarian for helping to acquire the necessary materials for the project. I also thank my college mates for words of motivation and encouragement through completing this report.
References
Chong W, Molinolo A, Chen C, Collins M. Tumor-induced osteomalacia. Endocrine-Related Cancer. 2011 [accessed 2022 Apr 6];18(3): R53-R77.
Fick C, Fratzl-Zelman N, Roschger P, Klaushofer K, Jha S, Marini J, Bhattacharyya T. Melorheostosis. American Journal of Surgical Pathology. 2019 [accessed 2022 Apr 7];43(11):1554-1559.
Florenzano P, Gafni R, Collins M. Tumor-induced osteomalacia. Bone Reports. 2017 [accessed 2022 Apr 7];7:90-97.
Marini J, Do A. Osteogenesis Imperfecta. 2020 [accessed 2022 Apr 7]. https://www.ncbi.nlm.nih.gov/books/NBK279109/
Minisola S, Colangelo L, Pepe J, Diacinti D, Cipriani C, Rao S. Osteomalacia and Vitamin D Status: A Clinical Update 2020. JBMR Plus. 2020 [accessed 2022 Apr 7];5(1).
Shaker J. Paget’s disease of bone: a review of epidemiology, pathophysiology, and management. Therapeutic Advances in Musculoskeletal Disease. 2009 [accessed 2022 Apr 6];1(2):107-125.
Teng Z, Zhu Y, Yu X, Liu J, Long Q, Zeng Y, Lu S. An analysis and systematic review of sarcopenia increasing osteopenia risk. PLOS ONE. 2021 [accessed 2022 Apr 7];16(4):e0250437.
Tu K, Lie J, Wan C, Cameron M, Austel A, Nguyen J, Van K, Hyun D. Osteoporosis: A Review of Treatment Options. 2018 [accessed 2022 Apr 7]. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5768298/
Figure 1
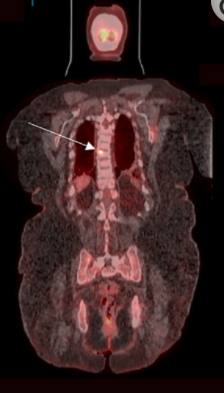
Figure 2
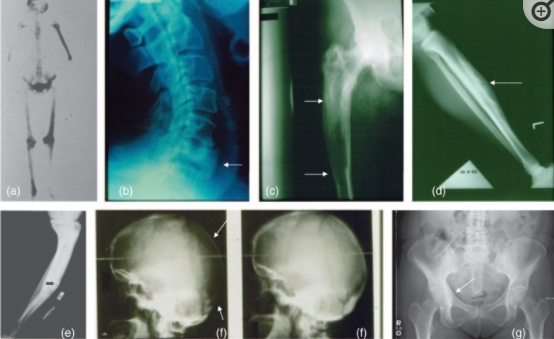
Figure 3

Table 1
|
Disease |
Areas of Prevalence |
|
Osteopenia and Osteoporosis
|
The diseases mostly occur in postmenopausal women in American society. The diseases also occur more in female than male counterparts. |
|
Osteomalacia
|
The disease is most common in adult Europeans. |
|
Paget’s Disease
|
The disease is most prevalent in the UK, Australia, North America, New Zealand, and France. |
|
Melorheostosis
|
Melorheostosis affects about 1 in 1 million people. Four hundred cases of Melorheostosis have been reported worldwide.
|
|
Tumor-induced Osteomalacia
|
The disease is rare, and only 1000 cases have been reported globally. |
|
Osteogenesis Imperfecta
|
The condition affects individuals at a ratio of 1:10,000-20,000 globally. Up to 25000 to approximately 50000 people live with this condition.
|
 write
write