Quality of care has been a major concern among healthcare professionals, patients, lawmakers and the general populace. Healthcare facilities are expected to deliver high-quality care to improve public health and service provision. According to Zuriati and Chiew (2020), the role of healthcare facilities is to offer services that meet the needs of surrounding communities and satisfies their expectations. Various factors including the social, economic, political and environmental drivers impact the quality of healthcare offered in various facilities. Clinical governance utilizes the factors that affect healthcare provisions to formulate strategies that ensure quality care (Buja et al., 2018). It offers guidance to healthcare professionals by focusing on risk management, quality improvement and patient safety. Clinical governance also identifies the responsibility of healthcare providers and other stakeholders including patients and how they should relate with each to promote their well-being. High-quality health meets all the legal requirements identified by the authorities within specific political jurisdictions. It also meets the social and ethical needs and expectations of the patients and communities around them. Additionally, it focuses on how healthcare delivery affects the economy and the environment. This report examines healthcare risks in a Hong Kong-based care facility, important clinical governance strategies and the audit cycle model and how they can be applied to remedy the challenges at the healthcare organization.
Healthcare Risks and Poor Quality of Healthcare in Hong Kong
The current thinking of what quality healthcare provision entails was by the National Health Service next review which proposed “high-quality for all” which was enacted by the Health and Social Care Act of 2012. According to the Health and Social Care Act of 2012, high-quality services providers must ensure patient safety, positive experience and safety (National Health Service, 2019). Clinical effectiveness requires healthcare providers to utilize evidence-based practices to improve patient healthcare outcomes. Healthcare programs must also ensure patient safety by using strategies that protect individuals from avoidable health risks and harms and promote well-being for all clients. Avoidable risks and hazards in healthcare include poor communication, employing staff with wrong job descriptions and qualifications, medical errors such as wrong patient identification and prescription and the use of inappropriate medical devices that might cause harm. Studies reveal that a lack of teamwork and interdisciplinary collaboration can significantly result in health risks and hazards that can harm the patients. On the other hand, the patient experience dimension of quality services focuses on giving individuals a positive experience by treating them with dignity, compassion, and respect. Healthcare providers must protect the patients’ right to privacy and autonomous decision-making (Kouwenhoven et al., 2019). They should collaborate with clients when delivering care by involving them in shared decision-making through patient-centred practices.
In Hong Kong, poor quality of healthcare has been detrimental to the healthcare system leading to the death of many patients according to the 2020 Annual Report on Sentinel and Serious Untoward Events (Hospital Authority of Hong Kong, 2020). The report focused on the cases of patient misidentification and medical errors and client self-harm practices such as suicides due to poor patient experience in various healthcare facilities in the Hong Kong administrative region. Between October 2019 and September Hong Kong healthcare facilities had various types of medical errors: 7 cases of known drug allergy, 4 cases of insulin-related medical errors, 4 cases of a dangerous drug and 11 cases of harm caused by anticoagulant prescriptions. Most of the medical errors occurred in accident and emergency departments and wards of Hong Kong healthcare facilities (Hospital Authority of Hong Kong, 2020). A few cases were recorded in the specialist out-patient departments. Patient misidentification reported in 2020 also occurred when referring to patients’ laboratory reports and medical history. Misidentification also occurred during drug prescription and administration. The facilities also had cases of maternal morbidities and deaths associated with delivery or labour. Some patients had a permanent loss of function while others died when receiving healthcare services.
Focus on Scenario 2: Example of a Healthcare Facility in Hong Kong
This paper focuses on Scenario 2 which involves a healthcare facility that has had multiple medical errors including wrong drug prescription and dosage, wrong patient identification and failure to record drug administration. The health facility has also increased the number of patient complaints characterized by concerns about client safety. These challenges have been persistent for more than 6 months. Service delivery at the organization does not have all the three dimensions of high-quality healthcare as stipulated by the National Healthcare Service. High-quality healthcare services ensure clinical effectiveness, positive patient experience and exceptional patient safety by avoiding medical errors (Kalender et al., 2020). Contrary to the expectations of NHS quality care, the healthcare facility described in scenario 2 does not prioritize patient safety and experience. The complaints received by the healthcare facility demonstrate that people are not satisfied with the quality of care services offered at the hospital. Clinical governance and appropriate interventions are needed to restore patient trust for the facility and improve their safety and healthcare outcomes by eliminating potential healthcare risks and medical errors in the organizations.
Maxwell Framework: Assessment of Quality Issue at the Organization
In 1984, Maxwell proposed six dimensions of quality care: effectiveness, access, equity, social acceptability, equity, relevance, efficiency and economy (Schiavone et al., 2021). Unlike, the NHS approach which focuses only on three dimensions of quality, Maxwell’s model offers an in-depth analysis of the components of quality healthcare. The model suggests that access to services is the first dimension of quality healthcare. Patients must have access whenever they need it. In the scenario described people have access to healthcare. Another dimension of quality is equity/fairness which means that all people have access to services and are not discriminated against based on their social status and situations. Quality health should also have social acceptance and effectiveness for individual clients (Kosikova et al., 2019). In this case, the healthcare services offered by the organization has social acceptance but lacks effectiveness for individual patients. This is because many patients receive but complain due to a lack of patient safety in the organization. Additionally, the organization has recorded many cases of medical errors such as wrong patient identification and inappropriate dosage which jeopardizes the patients’ health. Maxwell’s framework also suggests that quality healthcare should be affordable to improve access and equity.
Based on Maxwell’s framework for quality assessment, the organization needs to enhance patient safety and the effectiveness of its services to improve healthcare outcomes. The organization should also ensure that they gain the social acceptance of the surrounding communities and promote clients satisfaction. Healthcare should be accessible and relevant to the needs of the community to promote public health. Addressing patient complaints will also be an important step in meeting Maxwell’s approach to quality service. Quality control and accreditation play a significant role in ensuring patient safety and client satisfaction due to improved healthcare outcomes (Kavak et al., 2020). Quality and accreditation systems introduce standards that state the optimal quality service that hospitals and healthcare facilities should offer. Standards also define all components of effective healthcare delivery, the correct procedures and processes and the level of preparedness that health professionals need to have.
Clinical Governance and Healthcare Quality Control
Clinical governance is integral to the quality control and delivery of high-quality healthcare. According to the NHS (2020), clinical governance is “a framework through which healthcare organizations are accountable for continually improving the quality of their services and safeguarding high standards of care by creating an environment in which excellence in clinical care can flourish.” The primary goal of clinical governance is to assure patients of effective and sustainable healthcare services. Clinical governance promotes excellence and safety in the delivery of patient care. It also plays role in identifying, prioritizing and managing clinical care and risks (McSherry & Snowden, 2019). Clinical governance also protects the safety of patients and healthcare providers thus boosting the trust between them. Besides, clinical governance ensures optimal use of healthcare resources through interdisciplinary collaboration, teamwork and evidence-based practice. The healthcare issues in Hong Kong healthcare organizations, particularly the facility described in the scenario can be remedied through the application of the relevant quality control measures and accreditation.
Most healthcare organizations have clinical governance systems that include the audit model to improve the quality of care. Other frameworks of quality improvements are not always included as clinical governance strategies. Effective quality improvement plans require organizations to focus on the healthcare risk or issue that needs that should be investigated, adjusted and improve followed by the application of an appropriate framework (Kashani et al., 2019). The model selected for improvement should be transparent and open to the presentation and evaluation of quality improvement outcomes. Clinical governance also involves the regulation, inspection and accreditation of healthcare facilities to ensure that they meet all the optimal quality of service. Regulation offers standards of performance against which facilities should compare the services they provide (Wolfson et al., 2018). All facilities that meet the threshold performance and quality standards are allowed to offer their services to the public. On the other hand, inspections ensure that healthcare organizations do not deviate from the quality standards they had during accreditation. Inspection is done periodically and annual reports are submitted to the relevant regulatory and accreditation bodies.
Patient involvement is another critical aspect of service quality improvement. Patients have firsthand experience of the healthcare system and can provide insightful feedback with those clinicians and other stakeholders of healthcare organizations can utilize to improve the quality of services (Sinnige et al., 2022). The leader of the healthcare team in scenario 2 should actively engage patients in their treatment process. Additionally, the organization should use the patients complaints that have persisted for more than six months to improve patient safety and the quality of services offered. Patient involvement in quality improvement of healthcare services using various strategies. Involvement can be done by appointing a patient representative in quality committees of healthcare organizations (Pomey et al., 2019). Healthcare organizations should also analyze patient claims, complaints and concerns to identify the areas of improvement. For instance, in the scenario described in this paper, the healthcare team leader should understand that the major patient concern is patient safety. Quality improvement in the facility should also ensure patient safety by eliminating medical errors. Patients can also be involved in quality improvement by reviewing their information databases and allowing them to network with healthcare providers and enabling them to learn about effective self-care strategies (Aghajanloo, 2021). Additionally, patient-led assessments and survey responses can also be an effective way of being involved in quality improvement and delivery of care.
Application of Audit Cycle Model in Clinical Governance
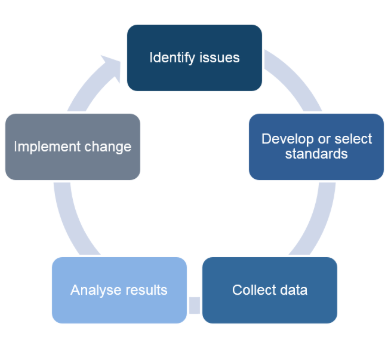
The audit cycle is a useful strategy in quality improvement in healthcare organizations. Clinical audit is used to examine whether care meets the quality standards, address the shortfalls identified and monitor improvements implemented to eliminate the shortcomings. It also ensures that healthcare practitioners comply with the required clinical standards set for quality care. The audit cycle also promotes evidence-based practice and patient-centred care. A clinical audit involves identifying the underlying healthcare issue. This is followed by the understanding of the issue from a perspective of the quality standards defined by the accreditation board. The auditor then develops a theory for change by identifying what needs to be done to improve quality and where the organization should be. The next step involves collecting data and testing the potential solutions for the healthcare issue identified. Data collection is followed by the implementation of the identified solutions to facilitate change and quality improvement. The audit process also involves quality control activities that evaluate monitor and regulate healthcare services offered to patients. It also ensures continuous quality improvement. The audit cycle for scenario 2 described in this paper is as follows:
The Audit Cycle
Audit topic/Planning and Preparation
The first stage of the audit cycle is to identify the topic/area of focus in the healthcare facility. This report focuses on patient safety, identification and dosage. The planning process involves creating that consists of healthcare professionals from various departments in the healthcare facility. Inter-professional collaboration and teamwork is important aspect of clinical audit and governance. Patients should also be involved in quality control. During planning the healthcare professionals are expected to develop specific, measurable, attainable, realistic and time-bound goals that will guide the process of change. The goal of this audit cycle is as follows:
- To eliminate medical errors in the facility by the end of the second month of implementation.
- To ensure patient safety by installing appropriate medical technologies that will facilitate accurate prescription, identification and recording of patient data.
Quality Health Care Standard/What Should Happen
The NHS and Maxwell’s framework for quality, healthcare services need to be effective, efficient, accessible, equitable distributed and relevant to the needs of the patients. Effective care meets the needs of patients and ensures that they are satisfied with the quality of services offered. Besides, the NHS expects healthcare providers to treat their patients with respect and dignity and protect their confidentiality and right to privacy. Setting standards is integral to quality control. It ensures that healthcare professionals have a template for delivering quality healthcare services.
Healthcare Quality Issue/What Is Happening
The healthcare facility has experienced several medical errors: lack of proper drugs records, wrong patient identification, wrong dosage and patient safety issues that jeopardize their healthcare outcomes. The facility has also received many complaints from customers due to dissatisfaction. According to the Hospital Authority of Hong Kong (2020), medical errors resulted in permanent loss of vital functions and deaths of many patients in Hong Kong healthcare facilities. Some patients with terminal illnesses such as cancer also committed suicide because they were dissatisfied with the quality of healthcare services offered to them.
Data Collection
The team leader at the healthcare facility is expected to collect data about the patients affected by the healthcare issue identified: a lack of patient safety due to improper drug records, wrong patient identification and inappropriate dosage. The data collected may include the number of patients affected by the healthcare issue, how each person was affected. It should determine the number of people that permanently lost their vital functions or died due to poor drug records, wrong patient identification or inappropriate dosage. Poor records and medical errors are due to a lack of efficient technologies to store and manage patient data (Menachemi & Collum, 2014).
Data Analysis
The information collected during the clinical audit indicates that there have been a series of patient complaints for the past six months because of a lack of patient safety. Many patients’ life is at risk and various adjustments need to be done. Medical errors are a result of a lack of proper technology for identifying patients, recording drugs and monitoring drug prescriptions. Inadequate training and development of employees is also a challenge because some healthcare providers are not able to operate the electronic healthcare records in the healthcare facility. Potential solutions for the problem include training and development of healthcare staff and installation of new healthcare technologies such as nursing information systems. Bates et al. (2014), suggest that using appropriate healthcare technologies to manage patient data may significantly reduce health is risks and eliminate avoidable deaths.
Implementation
The implementation of the identified solutions or change theory is accompanied by improvement in the quality of healthcare delivery. In this case, the healthcare facility is should install new healthcare technologies including nursing information systems and computerized patient records to improve how healthcare professionals record, store, access and utilize patient data. This will reduce medical errors that pose risks to patients’ health (Ngunyen et al., 2014). Training and development of healthcare providers will help them gain the appropriate knowledge, skills and competencies needed to operate the new medical technologies installed and implemented at the healthcare facility. The healthcare outcomes are evaluated to determine whether all the healthcare issue identified in the first stage has been addressed.
Significance of SMART Goals and Clinical Audit
The audit cycle is one of the most important strategies for clinical governance. The clinical audit allows healthcare organizations to be accountable for the continuous improvement of care. The process also helps organizations to safeguard high standards and offer quality care by creating an environment of excellence. The clinical audit also helps healthcare facilities to identify their strengths, weaknesses and possible areas of improvement (Pozo-Rodríguez et al., 2021). It increases the engagement of the patient in delivery through evidence-based practices and patient-centred care.
SMART goals help clinicians and other health care professionals to assess change and track their progress when implementing new strategies to improve quality. Goal-setting is motivated employees and allows them to focus their energy, effort and skills on the most important issues in the organization including the elimination of medical errors and patient safety (Drotz & Poksinska, 2014). SMART goals also ensure optimal use of resources because the healthcare facility will focus on installing technologies that will improve the quality of care. Training and development of healthcare providers also require effective goal-setting and implementation of the proposed solutions.
Recommendations
- The healthcare facility should submit the audit reports after 3 months to ensure that all staff members remain accountable for promoting, improving and maintaining high care standards to improve patient outcomes.
- The organization should actively involve patients in the audit cycle to establish the effectiveness of its services and the challenges facing patients in the facility. Addressing patient grievances is an important process in quality improvement.
- The organization should adhere to accreditation standards and have a quality control team that monitors performance to ensure that it does not deviate from quality care standards.
Conclusion
The health facility has also increased the number of patient complaints characterized by concerns about client safety. These challenges have been persistent for more than 6 months. Service delivery at the organization does not have all the six dimensions of high-quality healthcare as stipulated by the NHS and Maxwell’s model of quality. The audit cycle is a useful strategy in quality improvement in healthcare organizations. Clinical audit is used to examine whether care meets the quality standards, address the shortfalls identified and monitor improvements implemented to eliminate the shortcomings. It also ensures that healthcare practitioners comply with the required clinical standards set for quality care. Major steps in the clinical audit include planning, identification of the healthcare quality issue, and defining goals for improvement, implementation and evaluation. The organization can improve patient safety by installing new healthcare technologies and training developing its staff members.
References
Aghajanloo, A., Negarandeh, R., Janani, L., Tanha, K., & Hoseini‐Esfidarjani, S. S. (2021). Self‐care status in patients with heart failure: Systematic review and meta‐analysis. Nursing Open, 8(5), 2235-2248.
Bates, D. W., Saria, S., Ohno-Machado, L., Shah, A., & Escobar, G. (2014). Big data in health care: using analytics to identify and manage high-risk and high-cost patients. Health Affairs, 33(7), 1123-1131.
Drotz, E., & Poksinska, B. (2014). Lean in healthcare from employees’ perspectives. Journal of health organization and management.
Hospital Authority of Hong Kong. (2020). Annual Report on Sentinel and Serious Untoward Events. Hospital Authority Website. https://www.ha.org.hk/haho/ho/psrm/E_SESUE1920.pdf
Kalender, Z. T., Tozan, H., & Vayvay, O. (2020, September). Prioritization of medical errors in patient safety management: Framework using interval-valued intuitionistic fuzzy sets. In Healthcare (Vol. 8, No. 3, p. 265). Multidisciplinary Digital Publishing Institute.
Kashani, K., Rosner, M. H., Haase, M., Lewington, A. J., O’Donoghue, D. J., Wilson, F. P., … & Wu, V. C. (2019). Quality improvement goals for acute kidney injury. Clinical Journal of the American Society of Nephrology, 14(6), 941-953.
Kavak, D. G., Öksüz, A. S., Cengiz, C., Kayral, I. H., & Şenel, F. Ç. (2020). The importance of quality and accreditation in health care services in the process of struggle against Covid-19. Turkish Journal of medical sciences, 50(8), 1760-1770.
Kosikova, M., Vasanicova, P., & Litavcova, E. (2019). Analysis of aspects of the tourism development in Slovakia in the context of the European Space. Montenegrin Journal of Economics, 15(2), 127-137.
Kouwenhoven, P. S., Van Thiel, G. J., Van Der Heide, A., Rietjens, J. A., & Van Delden, J. J. (2019). Developments in euthanasia practice in the Netherlands: Balancing professional responsibility and the patient’s autonomy. European Journal of General Practice, 25(1), 44-48.
McSherry, R., & Snowden, M. (2019). Exploring Primary Healthcare Students and Their Mentors’ Awareness of Mentorship and Clinical Governance as Part of a Local Continuing Professional Development (CPD) Program: Findings of a Quantitative Survey. In Healthcare (Vol. 7, No. 4, p. 113). Multidisciplinary Digital Publishing Institute.
Menachemi, N., & Collum, T. H. (2011). Benefits and drawbacks of electronic health record systems. Risk management and healthcare policy, 4, 47.
National Health Service (2019). The NHS patient safety strategy. Safer culture, safer systems, safer patients.
Nguyen, L., Bellucci, E., & Nguyen, L. T. (2014). Electronic health records implementation: an evaluation of information system impact and contingency factors. International journal of medical informatics, 83(11), 779-796.
Pomey, M. P., Denis, J. L., & Dumez, V. (Eds.). (2019). Patient engagement: How patient-provider partnerships transform Healthcare organizations. Springer Nature.
Pozo-Rodríguez, F., López-Campos, J. L., Alvarez-Martinez, C. J., Castro-Acosta, A., Agüero, R., Hueto, J., … & AUDIPOC Study Group. (2021). Clinical audit of COPD patients requiring hospital admissions in Spain: AUDIPOC study.
Schiavone, S., Annecchiarico, A., Lisi, D., Mensorio, M. M., & Attena, F. (2021). Evaluation of Patients’ Perception of Safety in an Italian Hospital Using the PMOS-30 Questionnaire. International Journal of Environmental Research and Public Health, 18(9), 4515.
Sinnige, A., Spruijt, S., Saes, M., Van der Wees, P. J., Hoogeboom, T. J., & Teijink, J. A. (2022). Using a Learning Health System to Improve Physical Therapy Care for Patients With Intermittent Claudication: Lessons Learned From the ClaudicatioNet Quality System. Physical therapy, 102(1), pzab249.
Wolfson, M. A., Tannenbaum, S. I., Mathieu, J. E., & Maynard, M. T. (2018). A cross-level investigation of informal field-based learning and performance improvements. Journal of Applied Psychology, 103(1), 14.
Zuriati, Z., & Chiew, L. (2020). Relationship quality of health services with the satisfaction of patients in H. Hanafi Muara Bungo Hospital in 2019. Enfermería clínica, 30, 168-170.
 write
write