ABSTRACT
Background: Overweight and obese refers to excessive or abnormal fat buildup that poses a risk to human health. According to studies, more than 500 million individuals worldwide are overweight, which hurts various health consequences. Two-thirds of adults in the United States are overweight or obese. Although lifestyle and interpersonal influences play a significant role in the pathophysiology of overweight, gene mutation has also been proven to have a significant effect; predictions of susceptibility range from 40% to 85%. The objectives included causal estimates between overweight and coronary heart disease are obtained by dividing the instrument-outcome association by the instrument-exposure association of each single nucleotide polymorphism(SNP), and studying the association ratios using weighted method (IVW) for the main MR analysis.
Methods: All of the genetic data were obtained from publicly available GWAS summary data through the MR-BASE repository. The MR-BASE platform was developed by the Medical Research Council (MRC) Integrative Epidemiology Unit of the University of Bristol in the United Kingdom to facilitate two-sample MR analysis. The IVW estimate was used to infer the causal effects in the regression of the Wald ratio sets. By balancing each of the estimates by IVW, MR estimates as Wald ration estimates were derived.
Results: Based on Inverse-variance-weighted (IVW), we found that overweight is significantly related to the increased risk of coronary heart disease (OR 1.249, P=0.005, 95 % CI 1.064-1.434), alcoholism (OR 1.249, 95 % CI 0.869-1.797, P 0.253), and smoking (OR 0.178, 95% CI 1.503-1.317, P 0.004). The study found a causal association between overweight, smoking and alcohol consumption with CHD. We discovered that a genetically inherited high predisposition toward overweight was strongly related to an elevated risk of coronary heart disease and big vascular stroke using multiple MR analyses using recent public large-scale GWAS summary data.
Conclusion: In conclusion, we discovered that overweight is substantially associated with coronary heart disease risk, gestational weight gain, and a lower smoking risk in European populations using two-sample Mendelian randomization. These findings imply that an individual’s attitude plays a major impact in predicting illness risk or future health issues.
INTRODUCTION
Study Background
Overweight and obese refers to excessive or abnormal fat buildup that poses a risk to human health. According to studies, more than 500 million individuals worldwide are overweight, which hurts various health consequences[i]. Two-thirds of adults in the United States are overweight or obese. Although lifestyle and interpersonal influences play a significant role in the pathophysiology of overweight, gene mutation has also been proven to have a significant effect; predictions of susceptibility range from 40% to 85%[ii]. BMI is highly linked to cardiovascular disease, alcoholism, smoking and all-cause fatalities in large population-based epidemiological studies. BMI is linked to glycemic characteristics such as glucose and characteristics that are primarily related to CHD, such as blood lipids and blood pressure[iii].
On the other hand, few randomized trials have provided data that can precisely delineate the underlying causal links between cardiometabolic characteristics and overweight. Because of confounding when a correlation does not suggest a causal link and reverse causality, statistical relationships between BMI and characteristics or illness occurrences are critical4. The illness process changes the exposure of focus.
A recent phase III prospective study of weight management for cardiovascular preventive care was halted due to a lack of impact in terms of CHD occurrences. Using genetic markers in the Mendelian randomization technique is an alternate and effective way of determining whether a physical system leads to a result3. This method takes advantage of genetic variants’ random selection during gametogenesis, allowing them to be employed as parameter estimates (attributes that can be applied as substitutes for exposure but are unaffected by interfering) in causality studies. Because of the disparity between randomized and observational findings to date, we decided to study the impact of overweight in cardiovascular characteristics and events using a Mendelian randomization methodology. According to the worldwide burden of sickness, more than 4 million persons died in 2017 from obesity or overweight4. There is a distinction to be made between being overweight and being obese. Obesity refers to a considerably larger percentage of body fat than “overweight.” Hypertension (high blood pressure) is caused by obesity and refers to the pressure that blood exerts on the inner walls of the arteries. Obesity is frequently mentioned as a risk influence for CHD1. A high body mass index (BMI) has been linked to elevated jeopardy of coronary heart illness in several epidemiology studies. Environmental confounding factors and measurement error, on the other hand, can lead to an underestimation of the proportion of effect mediated in epidemiology research2.
Obesity is a significant risk factor for coronary heart illness (CHD) progression and development. Approximately 80% of people suffering from CHD are obese or overweight. Weight loss is a wide risk response remedy, even though obesity is generally considered a “small” CHD risk factor [iv]. Weight reduction can significantly impact a variety of “major” adverse outcomes, such as alcoholism, smoking, dyslipidemia, and hypertension. Despite the growing awareness that obesity is a potential cause, most cardiac rehabilitation (CR) treatments lack a specific, focused strategy to help individuals lose weight. As a result, the calorie restriction experienced during CR is minor and improbable to impact risk variables significantly5. Relying just on CR-associated workouts to facilitate losing weight is an inadequate method. Behavioural weight loss (BWL) strategies, on the other hand, are beneficial in the CR context. Studies showed that patients in CR-associated BWL strategies lose much more weight than those in regimens that do not provide a targeted measure4. Increased insulin responsiveness and other symptoms of obesity, such as lipid and hypertension abnormalities, are correlated to the BWL intervention’s further weight loss3. BWL therapies should be standard coaching for obese/overweight persons in CR programs to maximize CHD risk factor elimination2.
Adiposity has been linked to an increased risk of incident type 2 Diabetes Mellitus, stroke, and CHD in epidemiological studies[v]. Many inferential researchers claim similar relationships between overweight or obesity and CHD and selected adiposity variables; for instance, the risk Influences found similar relations with various ischaemic and CHD and central and general adiposity assessed by the hip to waist ratio and BMI for ischaemic stroke and CHD4. Alternative adiposity metrics have also been reported to have significant correlations with alcoholism. While classic forms of inaccuracy such as reverse causation, regression dilution, and confounding are minimized in Mendelian randomization (MR) analyses, they may be prone to the prospect of having bias (correlation of hereditary factors with many factors)3. Polymorphism can be perpendicular due to many downstream influences that abide by the SNP impact the understanding of interest, but MR assumptions are not jeopardized. Pleiotropy can also be lateral, in which the instruments or SNP affects systems other than those of the exposure of interest, possibly contradicting the MR hypothesis that the SNP only influences the consequence through the sensitivity of interest and generating in skewed causal estimations5. There seems to be a probability that pleiotropic influences will become balanced with multi-SNP detectors, allowing for reasoning about the exposure. Research studies use newly founded approaches robust to horizontal pleiotropy under additional assumptions to perform MR analyses of WHR and BMI in this study4. In the case of asymmetrical pleiotropy, apply MR-Egger modelling to offer a criterion for it and a causal prediction of treatment on outcome. Studies also employ the subjective median model, which can produce mathematical equations even in the manifestation of lateral pleiotropy if at minimum half of the data in the analysis derives from legitimate device variations and has the improvement of keeping more correctness in the predictions than MR-Egger124. The study by Dale is the most thorough examination of the causative role of adiposity in CHD, stroke, and T2D. It compares the causal influences of central adiposity against general adiposity overweight on several cardiovascular consequences: new CHD occurrences from current and future studies5. In an MR analysis of adiposity, studies offer the largest number of cardiometabolic characteristics ever studied, including lipids from the consortium for worldwide lipids genesis and a variety of new intermediate sickness end criteria, such as electrophysiology (ECG) assessments of lung diseases, renal markers, left ventricular hypertrophy, and media thickness of carotid intima as a biomarker of sub-clinical cholesterol5. Rese used the most comprehensive repertory available from recent genetic sequence correlation with SNPs for BMI for more than tripling the gene flow predicted in previous MR studies.
Study Objectives
The two-sample MR technique was utilized in this study, with causal estimates between prognostic factors produced by dividing the equipment correlation by the equipment association of each nucleotide polymorphism(SNP). Following that, the inverse weighted correlation ratios are combined. For the primary MR analysis, we used the (IVW) approach. The study achieved the aims through the use of a two-sample Mendelian randomization model. The objectives are as follows:
- Where causal estimates between overweight and coronary heart disease are obtained by dividing the instrument-outcome association by the instrument-exposure association of each single nucleotide polymorphism(SNP)
- These association ratios are then combined using the inverse-
- weighted method (IVW) for the main MR analysis.
MATERIALS AND METHODS
Study Population and Data Sources
All of the genetic data were obtained from publicly available GWAS summary data through the MR-BASE repository. The MR-BASE platform was developed by the Medical Research Council (MRC) Integrative Epidemiology Unit of the University of Bristol in the United Kingdom to facilitate two-sample MR analysis[vi]. The GWAS outcomes are usually insufficiently precise, destabilizing the efficient application of this method in analysis. MR-Base (http://www.mrbase.org) is a website that incorporates précised database of comprehensive GWAS outcomes (no limitations based on statistical importance) with an application R packages, web app, and software design interface that systematize two-sample MR analysis6. The database presently encompasses 11 billion single nucleotide polymorphism (SNP)-trait associations from 1,673 GWAS and is updated on a regular basis.
Statistical Methods
Standard Two -Sample MR
In this study, all MR analyses were calculated using R packages in R version 3.6.1 from the R Core Team, based in Vienna, Austria1,6,9. The Wald ratios for each genetics instrument were constructed by dividing the association outcome for each instrument by the exposure association for each instrument using a two-sample MR summary[vii]. The IVW estimate was used to infer the causal effects in the regression of the Wald ratio sets. By balancing each of the estimates by IVW, MR estimates as Wald ration estimates were derived.
Radial MR
The directional pleiotropy of each genetic instrument was determined using radial MR regression6. Cochran’s statistics were used to investigate the heterogeneity of the Wald ratio estimations. The radio plot method was used to find single outlier SNPs that created substantial disparities. In radial MR, the variance of the instrument’s associated outcomes and the variance of the instrument’s associated exposure were both used for weighting, but in two-sample MR, the variance of the instrument result association was used5.
MR RASP
We used MR‐Robust Adjusted Profile Score (RAPS) technique to model pleiotropic influence of genetic variations using a random‐impact distribution[viii]. It is worth noting the assumption made that pleiotropic influences normally distributed about point zero with unknown value of variance8. We used the profile-likelihood to estimate the variance and causal influence of the pleiotropic effect function.
MR egger
Traditionally, the MR technique does not presume that pleiotropy has no effect on any SNP outcome relationships, therefore all variations are permitted to be non-zero8. The assumption is that the size of pleiotropy effects is unaffected by respective instrument strengths. In other words, the size of the variants provides no information about the sizes of other variants, a situation known as InSIDE (Instrument Strength Independent of Direct Effect). MR eager, like the IVW approach, makes Nome assumptions. A regression of the SNP result relation on the SNP exposure relationship is used in this strategy7. This approach can only discover pleiotropy if it is ‘directional,’ meaning it has a non-zero average value.
RESULTS
GWAS Consortium
Table 1 below shows a sample of European participants with overweight, alcoholism, cigarette smoking and CHD conditions:
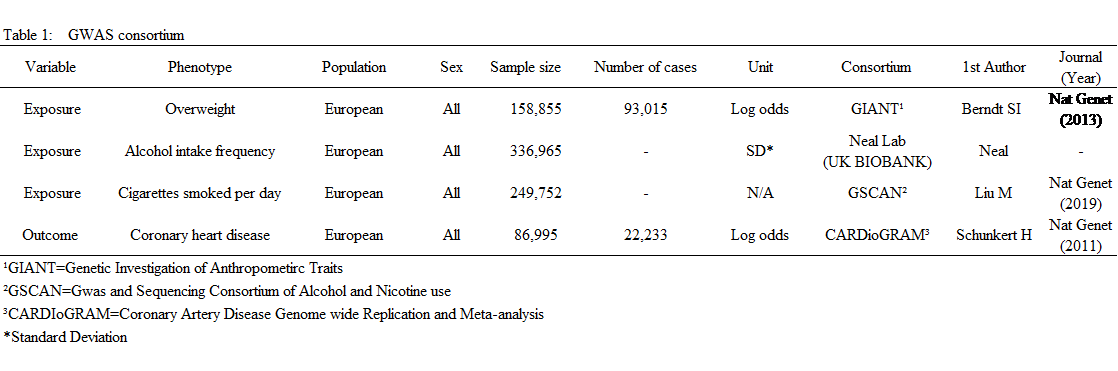
Table 1: GWAS data obtained from the MR-BASE
Overweight and CHD
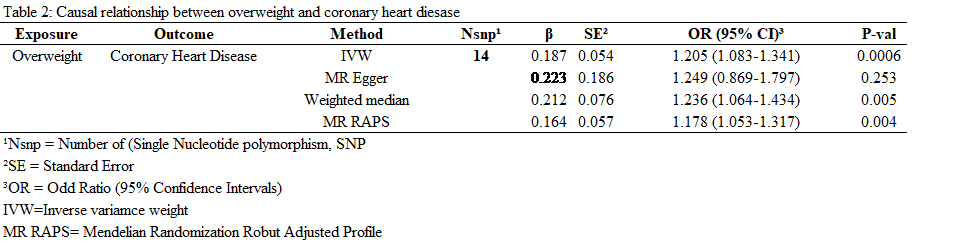
The table below shows the relationship between Overweight and CHD:
 <
<
Table 2: The causal association between overweight and CHD.
The MR test is as illustrated below:
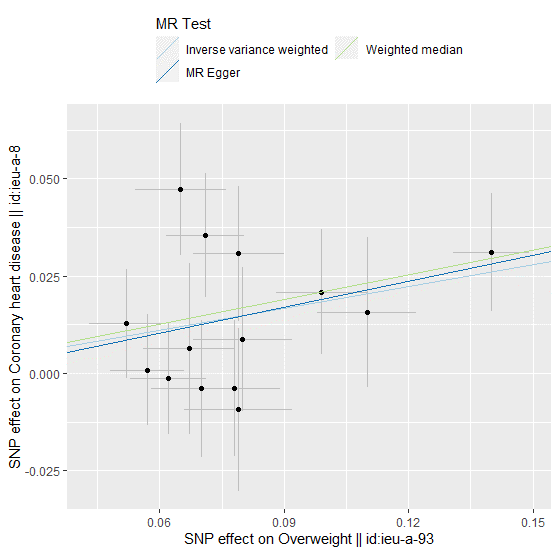
Figure 1: A plot relating the effect sizes of the SNP overweight association CHD.
Figure 2 and 3 below shows the causal effect on overweight on CHD:
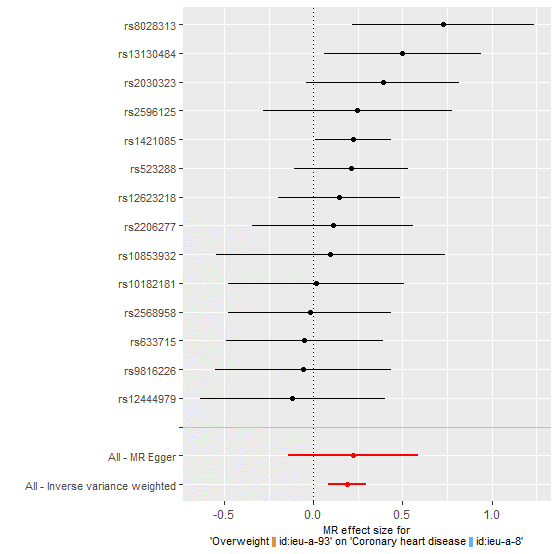
Figure 2: MR size effects for overweight and CHD.
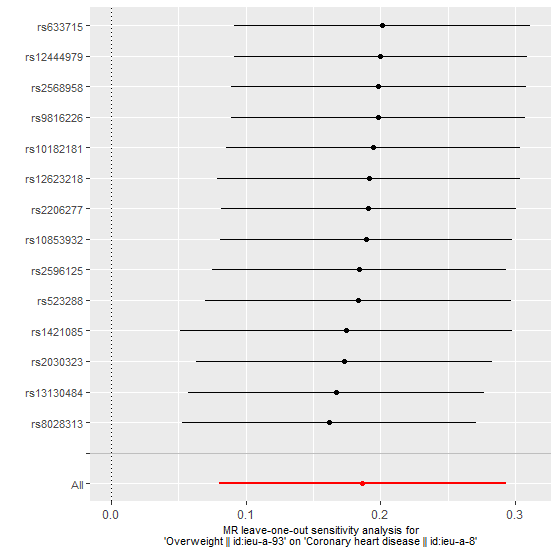
Figure 3: MR leave-one-out sensitivity analysis for overweight indicating a varied causal association between overweight and CHD.
MR Analysis for Detection of Individuals Outlier SNPs
The analysis without the outliers is illustrated in the figure 4 to figure 6 below:
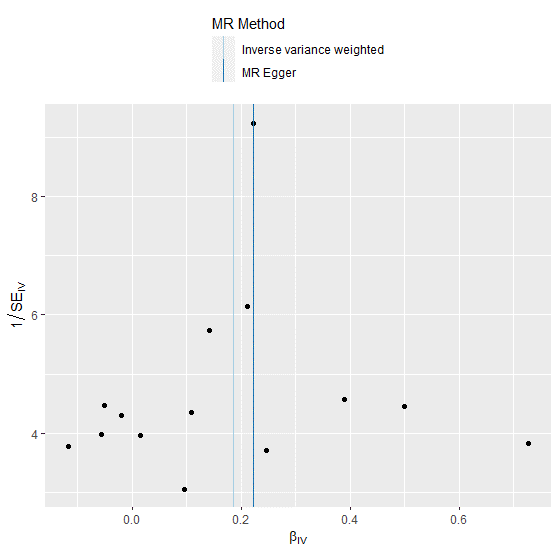
Figure 4: Funnel plot showing the relationship between the cause effect of overweight and coronary heart disease.
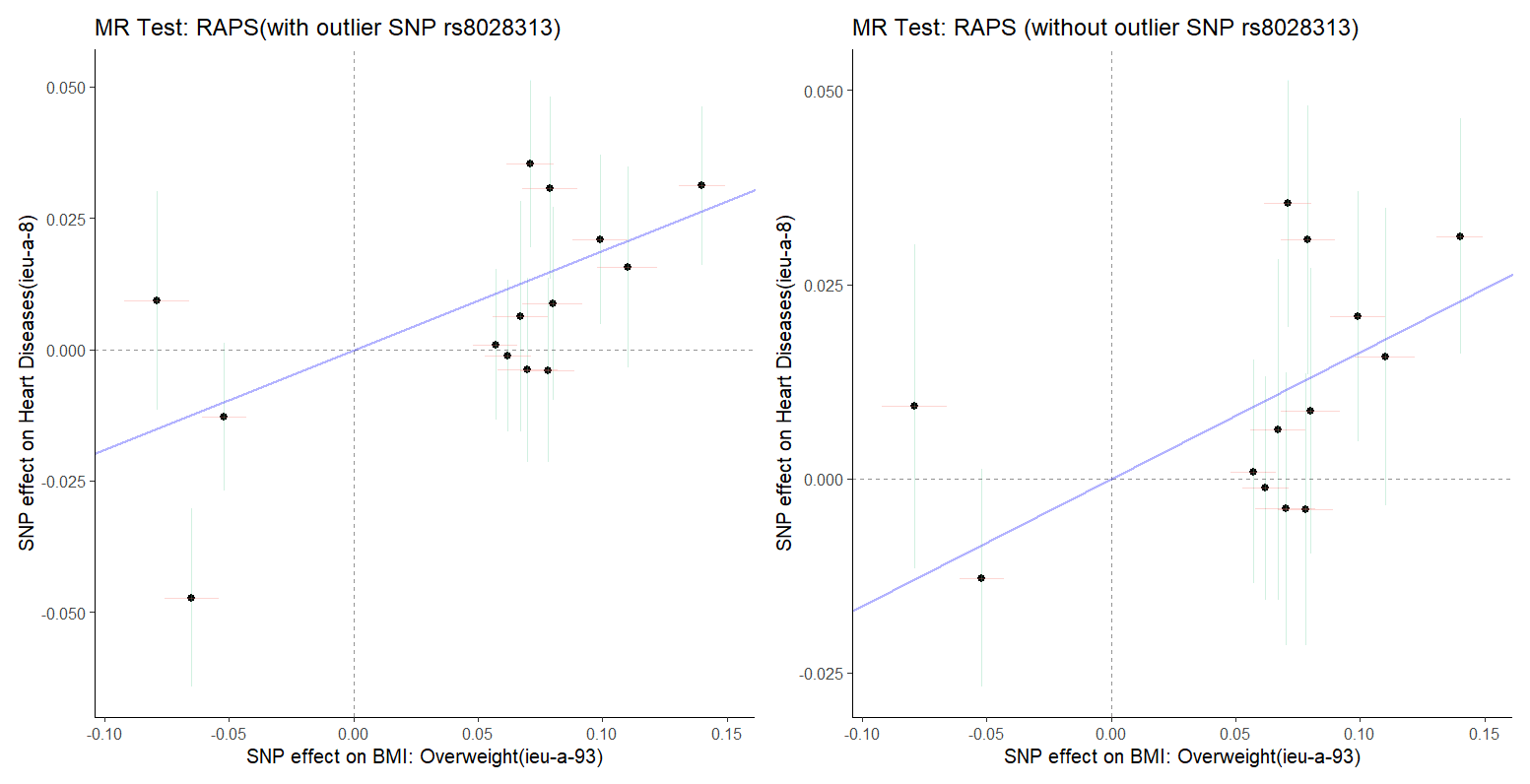
Figure 5: (Left) and 6 (Right). The MR test with outlier rs8028313 and MR test without outlier rs8028313.
Alcohol and Coronary Heart Disease
The table below illustrates the relationship between alcohol consumption and CHD:
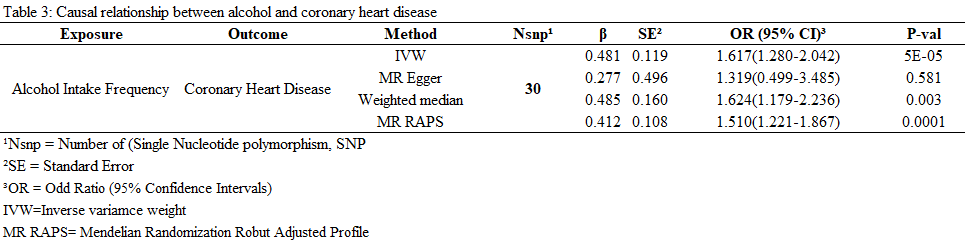
Table 3: The causal relationship between alcohol and CHD.
The causal effect of alcohol intake on CHD graphically illustrated by figure 6 to figure 10 below:
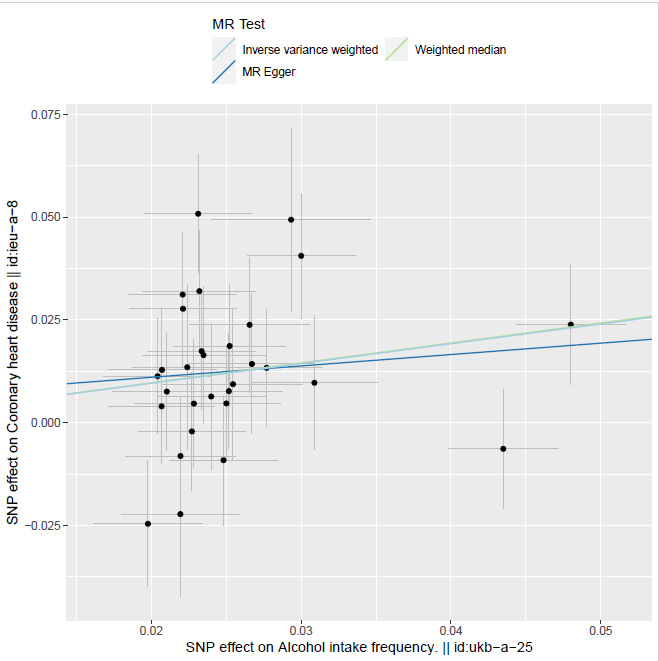
Figure 6: Two sample MR estimates showing a causal association between alcohol and CHD.
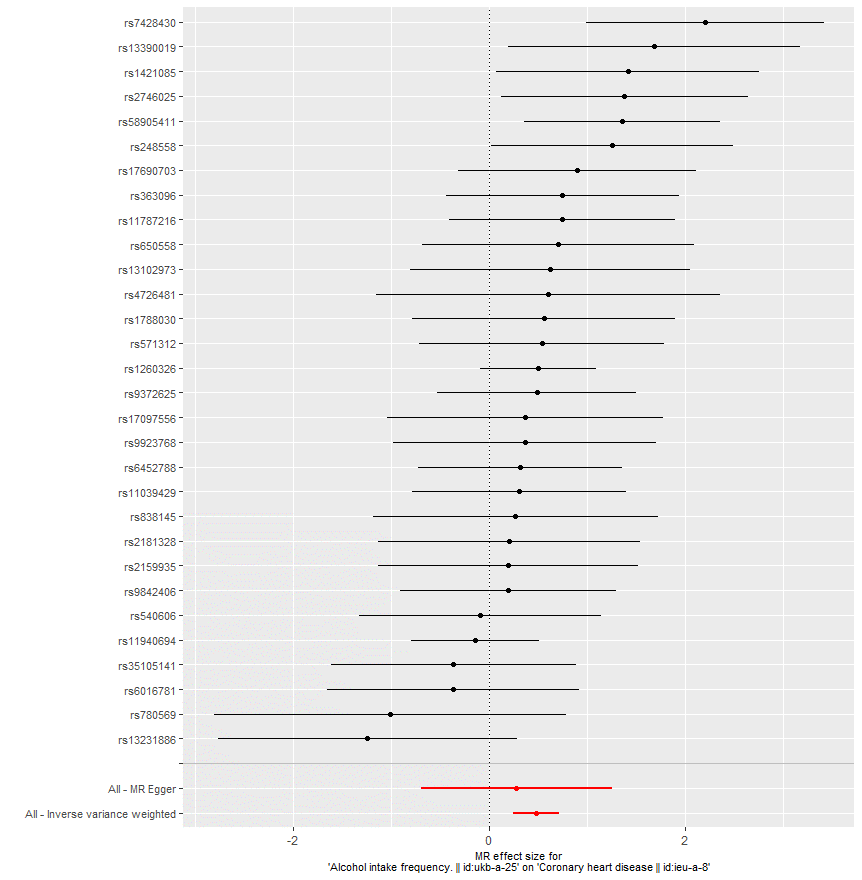
Figure 7: MRI effect size for alcohol intake frequency on CHD showing a strong causal relationship between the alcohol variable and CHD outcome.
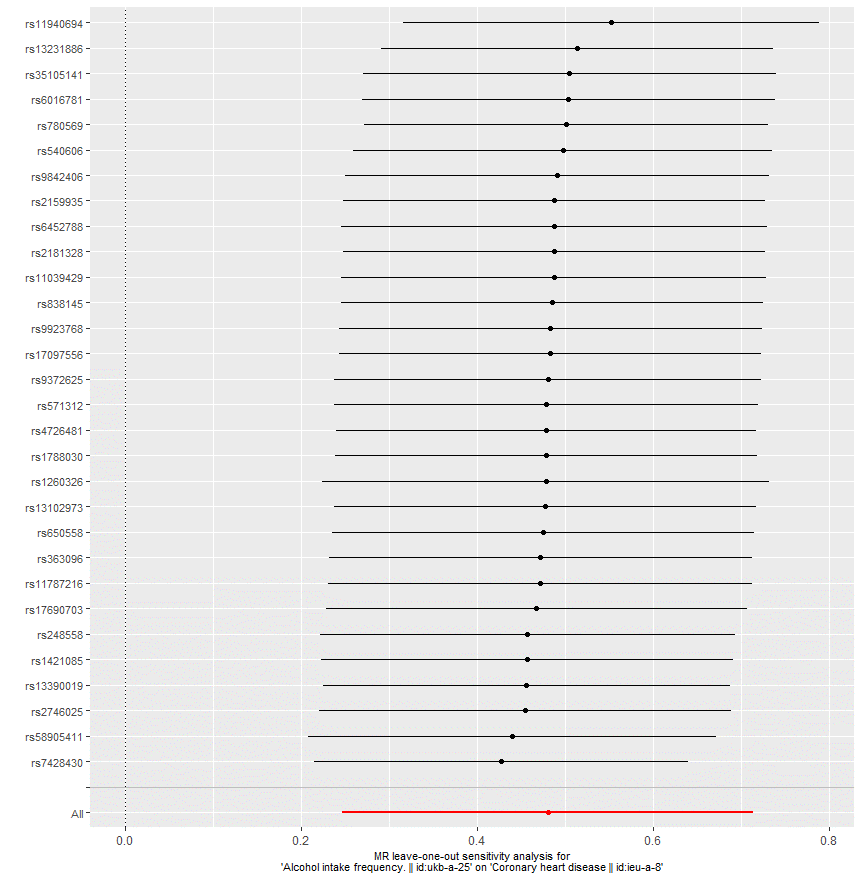
Figure 8: MR leave-on-out sensitivity analysis of alcohol intake frequency on CHD, indicating a strong association between alcohol intake and CHD.
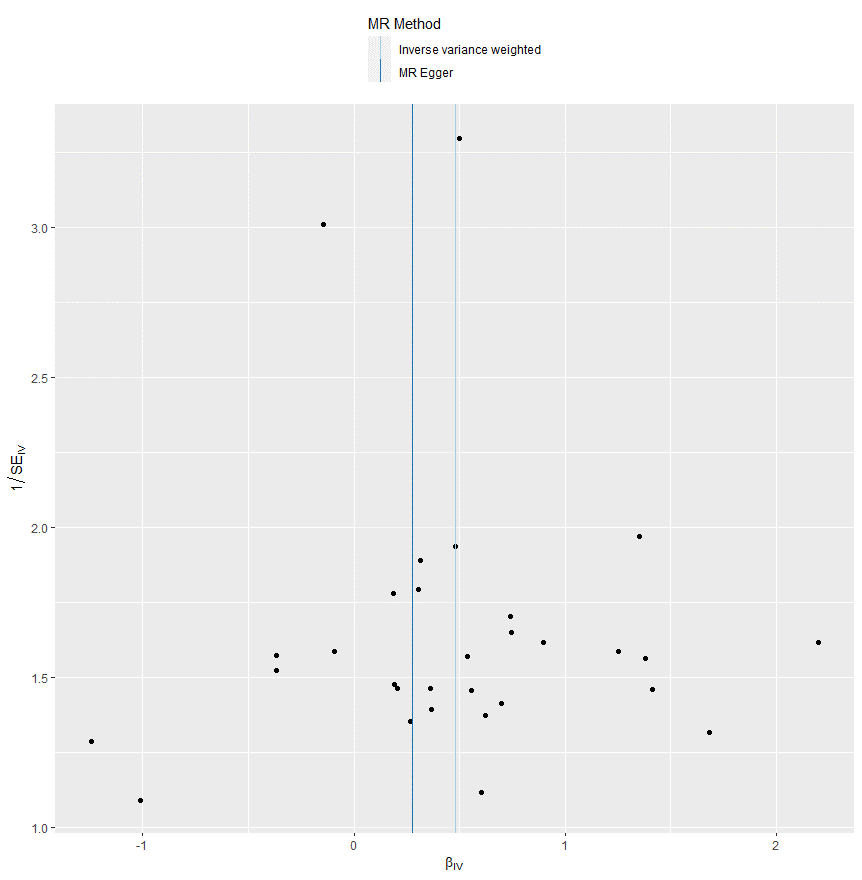
Figure 9: The causal relationship between alcohol intake frequency and CHD based on IVW and MR-Egger methods.
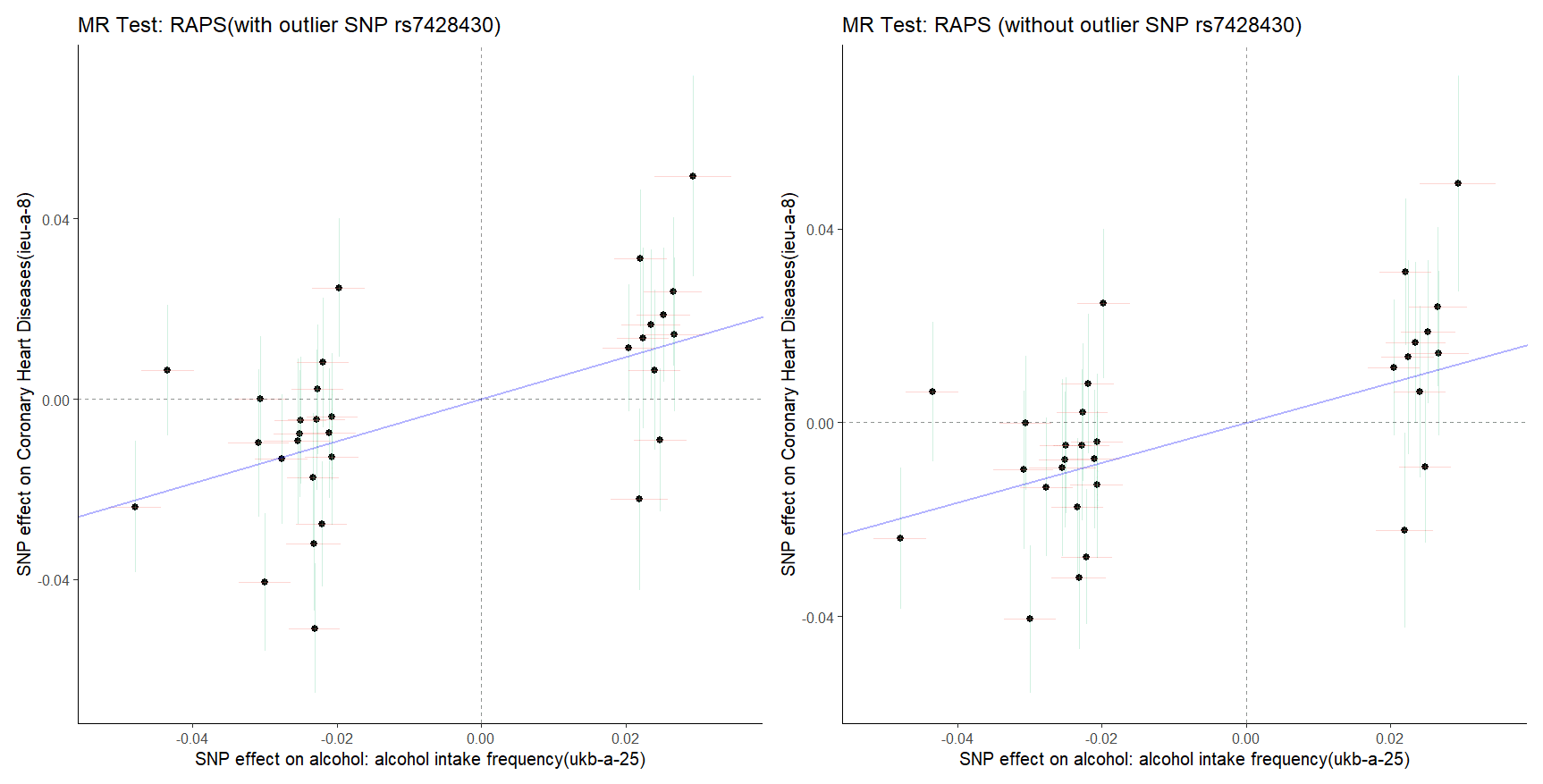
Figure 10 : (Left) and 11 (Right). The MR test with outlier rs8028313 and MR test without outlier rs8028313.
Smoking and CHD
The table below illustrates the relationship between smoking and CHD:
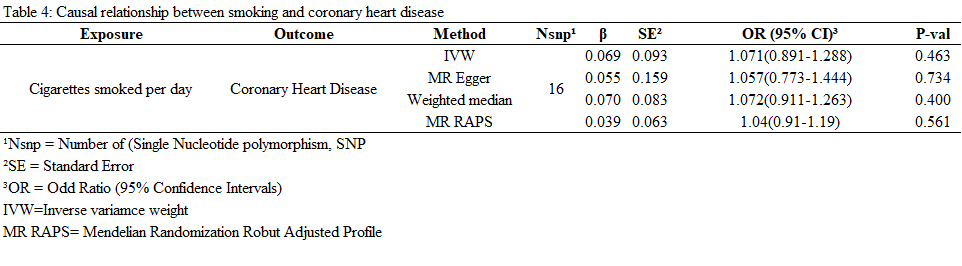
Table 4: Causal relationship between smoking and CHD.
The relationship between smoking and CHD illustrated in figure 12 to 17 below:
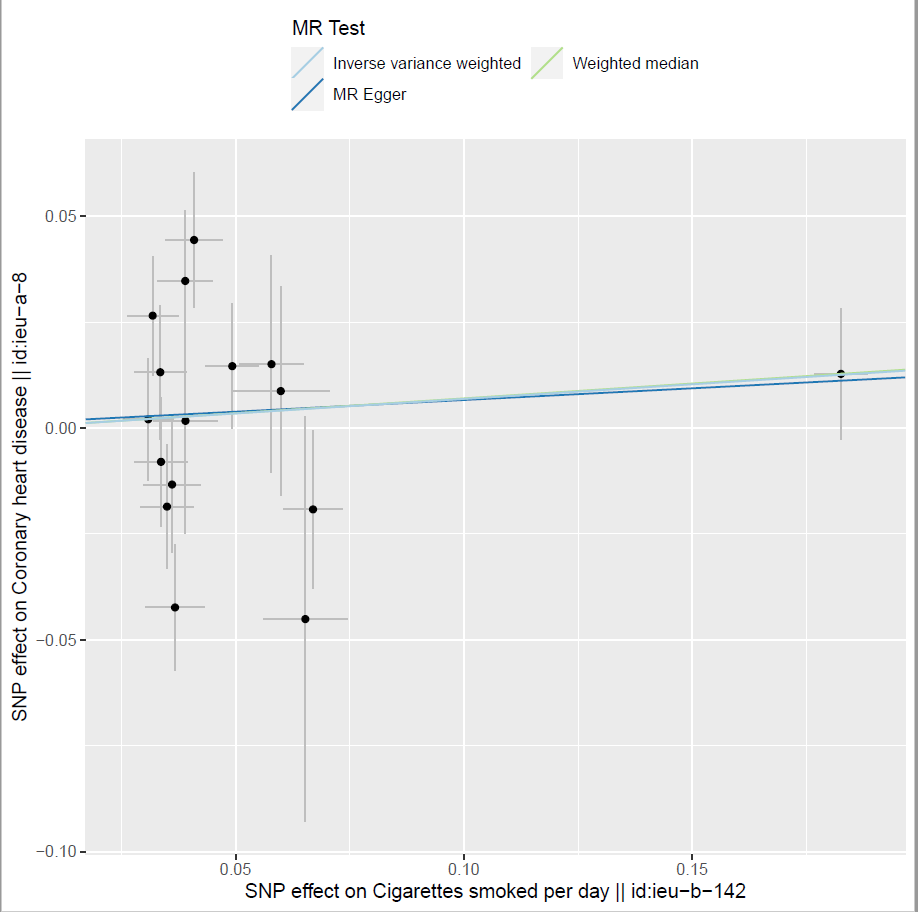
Figure 12: Two sample MR estimates showing a causal association between smoking and CHD.
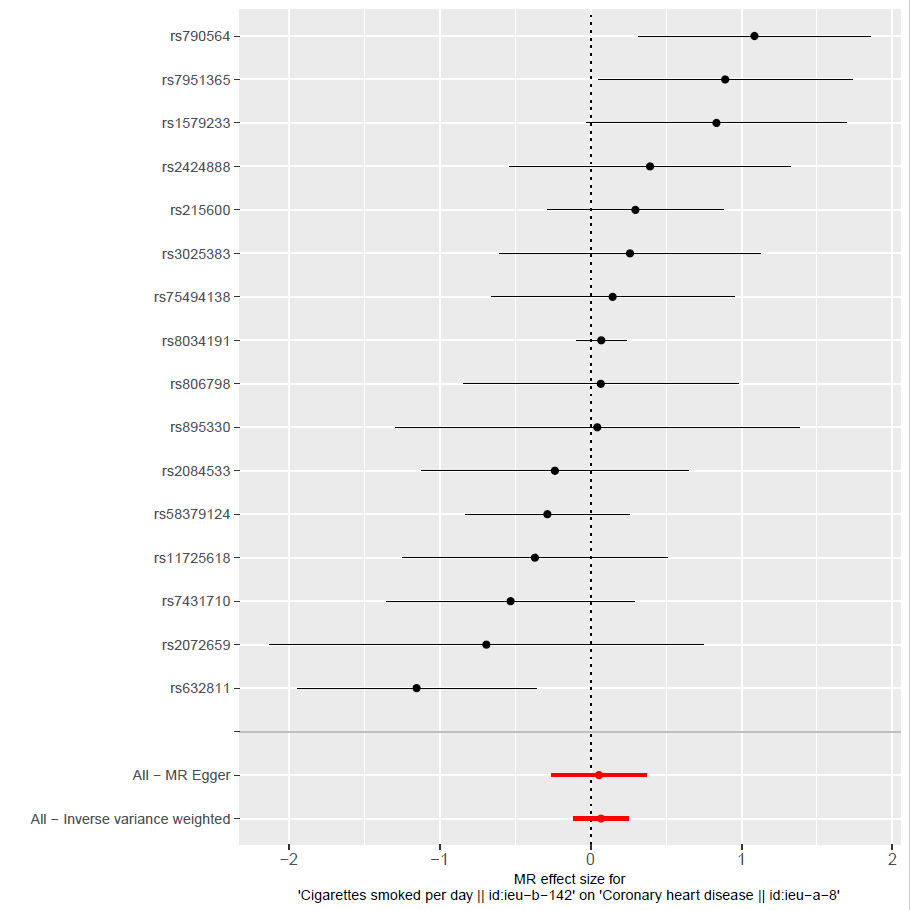
Figure 13: MRI effect size for alcohol intake frequency on CHD showing a strong causal relationship between the smoking variable and CHD outcome.
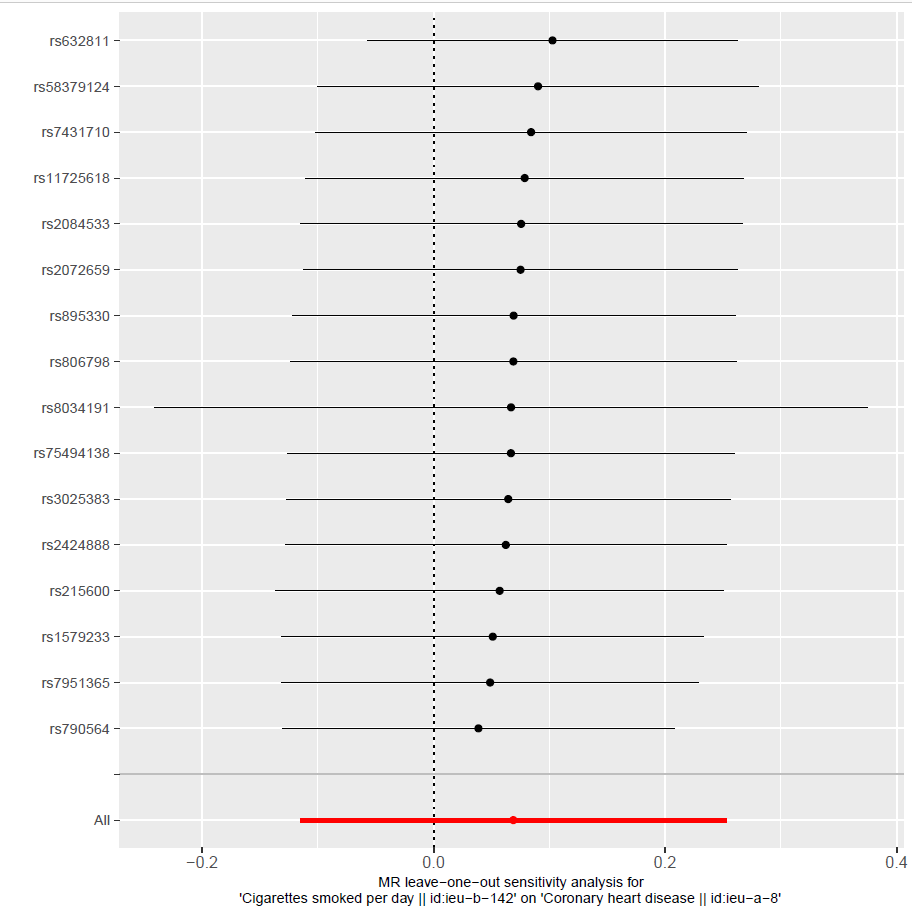
Figure 14: MR leave-on-out sensitivity analysis of alcohol intake frequency on CHD, indicating a strong association between smoking and CHD.
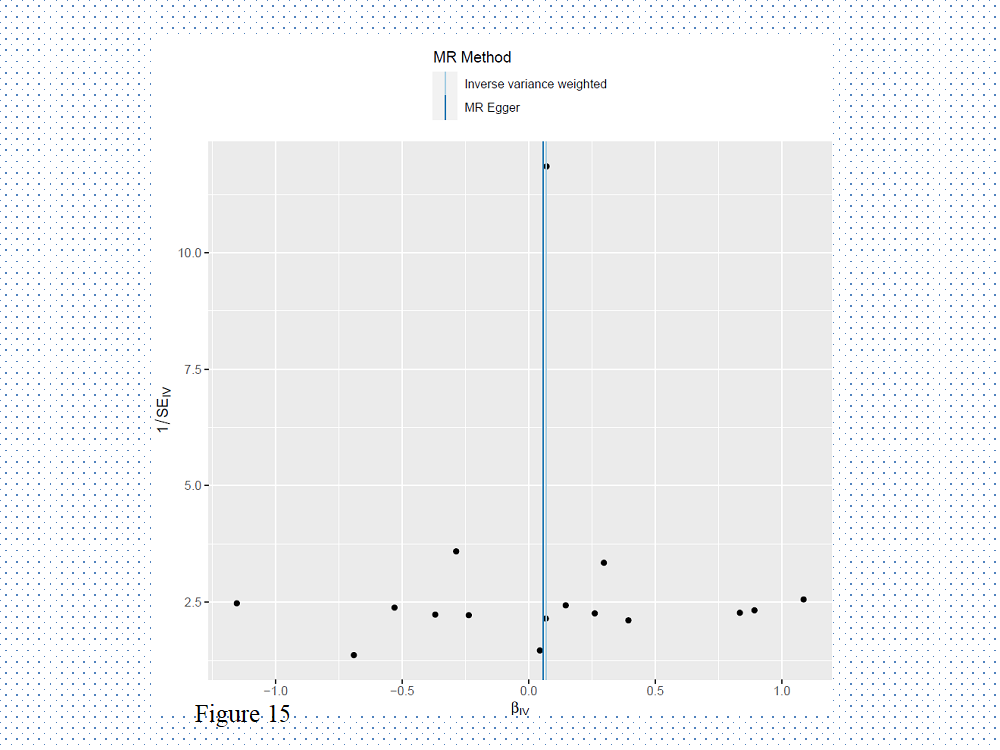
Figure 15: Two sample MR estimates showing a causal association between smoking and CHD.
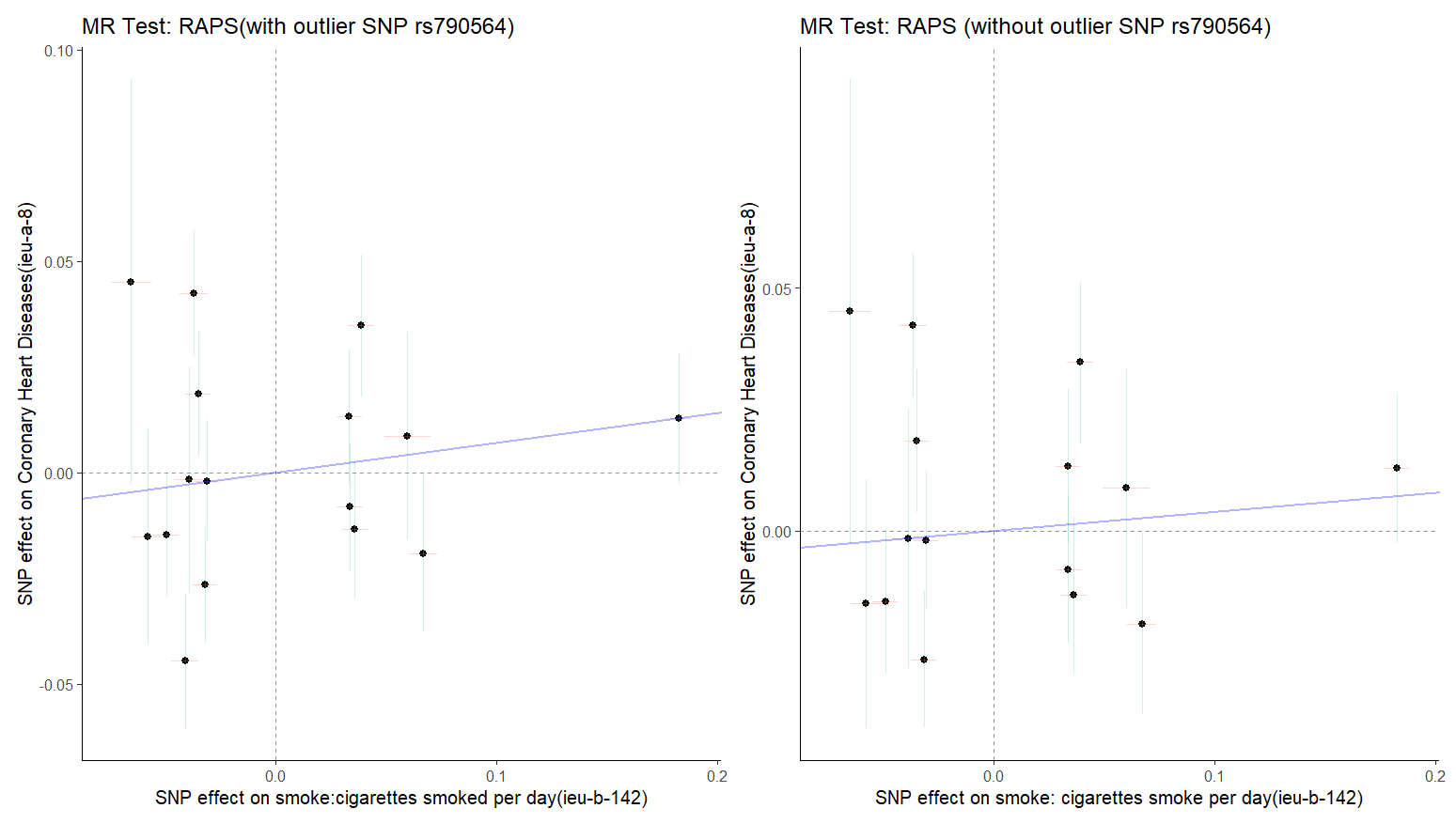
Figure 16 : (Left) and 17 (Right). The MR test with outlier rs8028313 and MR test without outlier rs8028313. Both MR tests indicated a positive causal association between smoking and CHD.
Comparison between Overweight, Smoking, and Cigarette Smoking
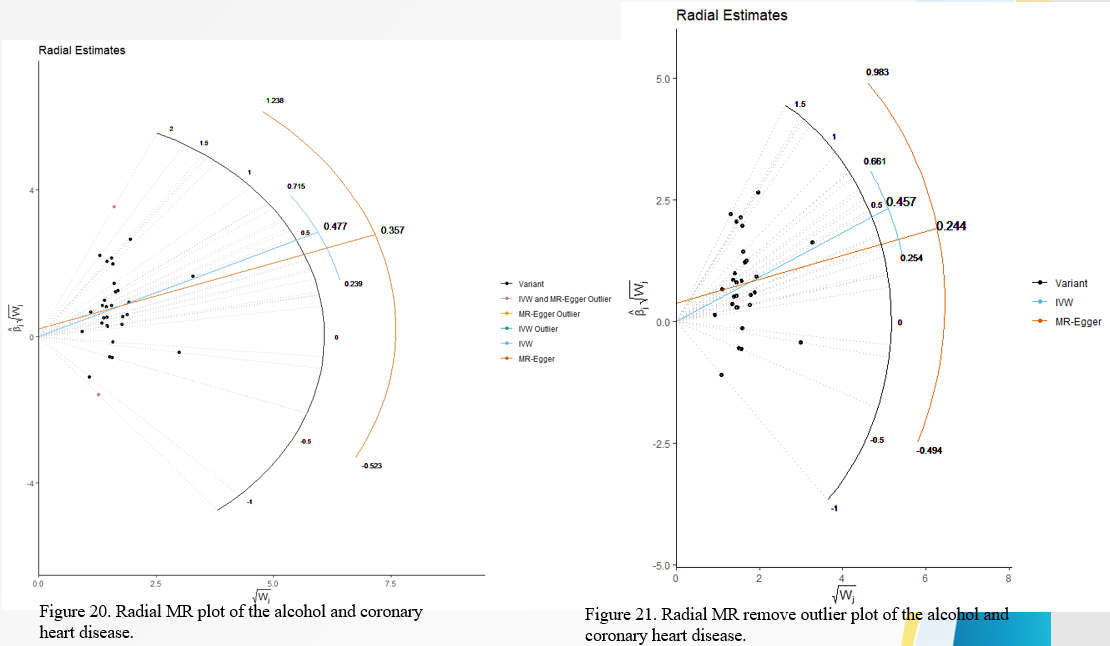
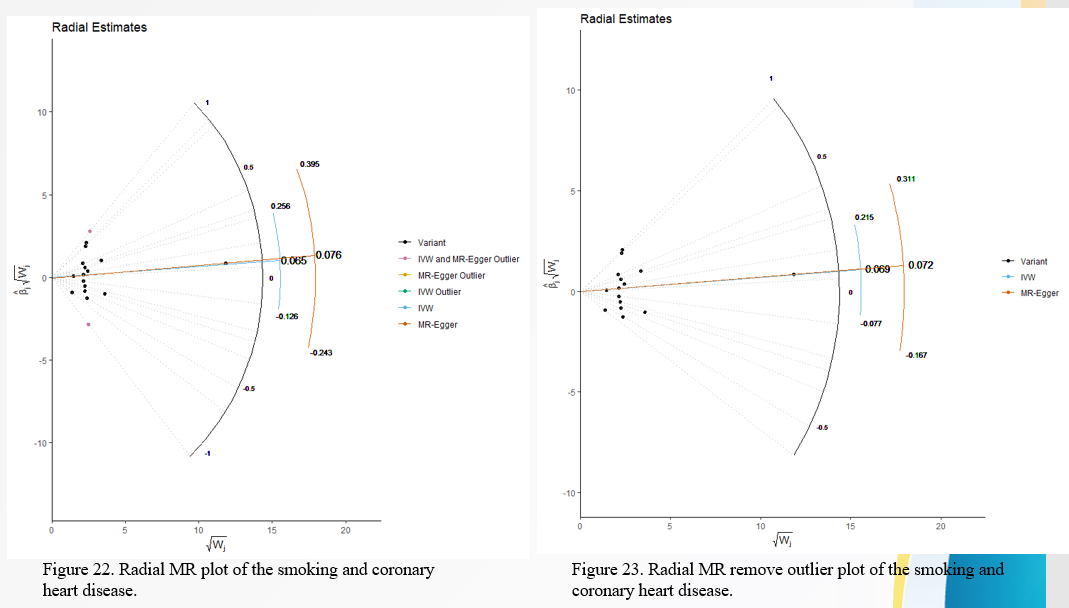
Table 5 to table 9 below illustrates the relationship between overweight, smoking, and cigarette smoking:
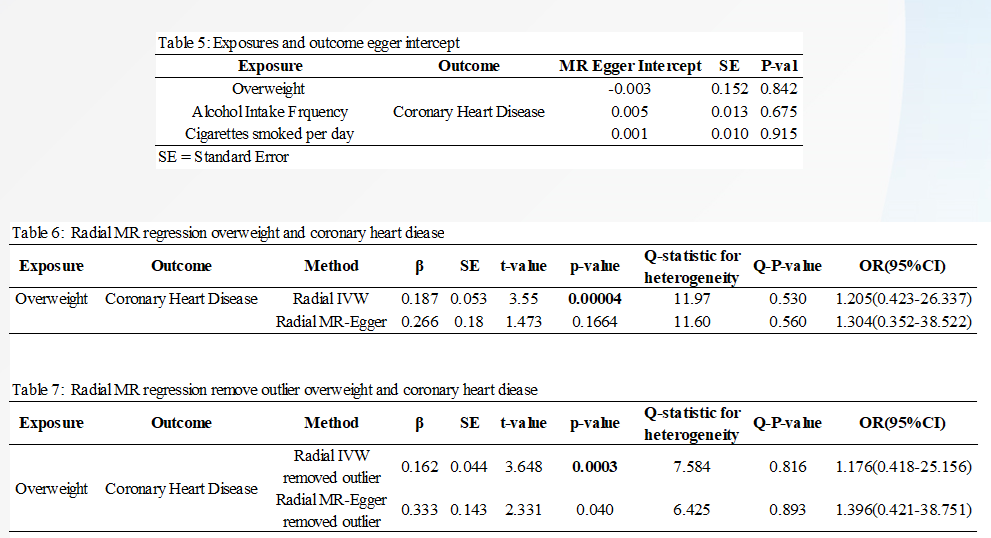
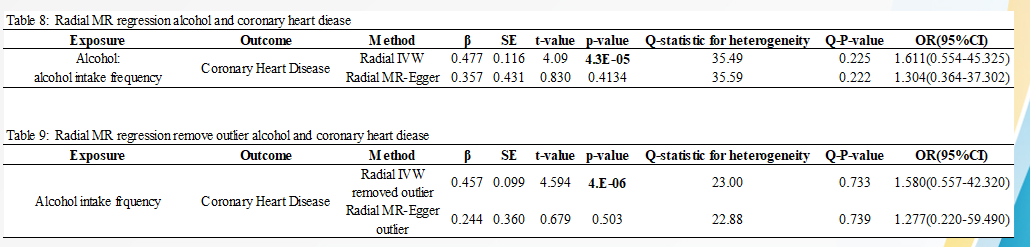
The Radial estimates from regression are as illustrated in figure 18 to figure 21 below:
DISCUSSION
Main Findings
Mendelian randomization was applied in this study to investigate the function of human behaviour in the development of cardiovascular disease and their health conditions. We discovered that a genetically inherited high predisposition toward overweight was strongly related to an elevated risk of coronary heart disease and big vascular stroke using multiple MR analyses using recent public large-scale GWAS summary data. Furthermore, a high predisposition to be overweight was tangibly linked to obesity markers. We also discovered that a genetically established strong predisposition toward obesity was the development and sustainability with a lower incidence of drinking, alcoholism, and smoking. The number of overweight European participants was 158855, whereas those who drank alcohol were 336965. The number of people who smoked cigarettes per day was 249 752, whereas those who had CHD outcomes were 86, 995, implying that the participants had high rates of smoking and drunkenness, which could predispose them to CHD. With a P-value of 0.0006, the IVW approach revealed that the odds ratio (OR) for a single standard deviation (SD) rise was 1.205 with a 95 percent confidence interval (1.083-1.341). (Table 2). The weighted median technique (1.249, with a P-value of 0.005) and 95 percent CI (1.064-1.434). We assessed the MR-Egger methodological approach (OR, 1.249) at 95 percent CI (0.869-1.797), P-value of 0.253 was both in agreement with these findings. The study found a causal association between overweight, smoking, and alcohol consumption with CHD using inverse-variance-weighted. The (IVW) (95 percent CI 1.083-1.341, OR 1.205, P 0.0006), weighted median (OR 1.249, P= 0.005, 95 percent CI 1.064-1.434), MR-Egger (OR 1.249, 95 percent CI 0.869-1.797, P 0.253), and MR RAPS (OR used a two-sample MR to investigate the link between smoking and CHD. We discovered the OR value (1.071) at 95 percent CI at the genome-wide statistical significance threshold of p 0.463. (0.891-1.288). When assessed at a 95 percent confidence interval, the radial IVW data revealed a larger positive connection between alcohol and CHD (OR 1.611). (1.5540-45.325). The radial MR-Egger data showed a similar pattern, indicating a positive relationship between alcohol and CHD (OR, 1.580, 95 percent CI) (0.557-42.320)
To discover any apparent pleiotropy in the correlations calculated using the usual IVW assessment, we applied the most recent MR approaches, including radial MR and multivariable MR4. Amongst the essential basic assumptions in MR analysis is the absence of pleiotropy. However, obtaining valid MR results after adjusting for pleiotropy is difficult. We employed radial MR to find outlier SNPs and a more realistic weighting mechanism, indicating that being overweight raised the risk of coronary heart disease, big vascular stroke, and infarction considerably3. Overweight has a critical correlation with obesity indicators such as the waist to hip ratio, waist circumference, and body mass index, according to the axial MR study. Utilizing radial MR, we also confirmed that being overweight is related to alcoholism and smoking. Nonlinear system MR analysis revealed that the link between obesity and CHD became weaker and negligible5. This study found that abdominal fat could play a role in the relationship between obesity and coronary heart disease by acting as a possible vertical pleiotropy. When we controlled the influence of the waist-to-hip ratio, however, parametric MR analysis revealed that the relationships between obesity and drunkenness and smoking after the assignment grew stronger6. This research found that being overweight has an impact on alcoholism that is independent of abdominal obesity.
Previous Observational Studies
Overweight and Cardiovascular Diseases
According to European data, the ideal cardiovascular mass in slim people is linked to the disease of survival. Obese society is a problem[ix]. As a consequence of rapid Body mass CARDIOVASCULAR and slender people, weight excess and minimization is difficult for firms in the middle are the most relevant class, a population even though loss appears to be linked to death[x]. To indicate weight. Data from and such evidence is confined to the association in studies by insurance companies. Other pathologic discoveries make it challenging to gain cause-and-effect relationships. Patterns in mortality risk have been studied repeatedly. However, data from weight for various reasons and impacts have been collected from the entire study population. Obesity, hazards in the population, evaluation parameters, and overall and beneficial factors were all determined in this study. Feed intake with age is common in most developed regions. Once obtained, it is stubbornly maintained without exercise, or confounding resulting from health impairs low sociocultural and can be utilized to investigate the influence of overweight in nonsmokers1. These statistics reveal that those somewhat malnourished may gain some weight, but their mortality rate declines. Death happens compared to mortality overweight people, who improved, the insurance in data in those underweight with time[xi]. Whether the role of age on appropriate weight estimation varies by age is a point of disagreement, as is the impact of concealed sickness caused by smoking on weight.
Being overweight contributes to heart disease in three ways, and what you can do to reclaim control of your actions and combat hunger and heart disease. It can affect your cholesterol level, for starters. Obesity is well recognized for rising bad serum cholesterol and lowering good higher lipoproteins cholesterol on occasion[xii]. The clearance of plaque from the arteries and the decrease of the risk of cardiovascular illnesses are both dependent on cholesterol levels. Second, it can boost your pulse rate. Obese persons require more blood to provide nutrients and oxygen to their bodies, resulting in higher blood pressure. The human body will need more pressure to transport this blood to the whole body. High blood pressure is a leading factor of heart failure, which are unfortunately more common among overweight people[xiii]. Thirdly, it carries the risk of causing diabetes. Obesity causes many medical problems, such as high cholesterol, high blood pressure, and heart failure. Obese people are also more likely to develop diabetes. At least three-quarters of alcoholics aged 65 and over develop heart disease. Even though people with diabetes are two to four times more likely to develop heart disease, the European Heart Association considers diabetes to be one of the top seven key avoidable factors for heart disease[xiv]. If you have hypertension that hasn’t been linked to heart disease, now is the time to act.
We discovered that being overweight causes cardiovascular risk factors such as dyslipidemia, drinking, hypertension, and sleep disturbances. Obesity, like other cardiovascular events, contributes to the development of cardiovascular disease and cardiovascular disease mortality. Recent research has identified abdominal obesity as a cardiovascular disease risk sign irrespective of BMI, as measured by waist circumference[xv]. Radiology methods for evaluating body composition, particularly visceral adiposity, have also advanced significantly. Excess visceral adiposity has been linked to worse cardiovascular outcomes in studies that measure fat depots, including ectopic fat. Metabolic syndrome and associated systemic inflammation and endothelial dysfunction are improved by changing one’s lifestyle and losing weight. Lab tests of medical weight loss, on the other hand, have not shown a reduction in vascular complications rates.
In contrast, prospective studies comparing weight loss surgery patients to nonsurgical obesity patients found that surgery patients had a lower risk of coronary artery disease. The implications of adiposity upon that diagnosis, clinical care, and consequences of atherosclerotic cardiovascular disease, heart failure, and arrhythmias, particularly irregular heartbeats and tachycardia, is summarized in this statement. We look at the impact of obesity on noninvasive and invasive diagnostic techniques for cardiovascular disease in particular. We also look at the effects of obesity affecting heart hypertrophy and prognosis in heart failure patients with reduced or retained ejection fraction. Finally, we discuss how behavioural and therapeutic weight loss therapies affect coronary artery disease, heart failure, and atrial fibrillation consequences.
Alcoholism and Overweight
Alcohol consumption would have most certainly contributed to the additional energy intake associated with weight gain in some persons throughout the decades. However, the present evidence is conflicting and restricted, making it virtually impossible to draw clear conclusions concerning the effect of alcohol on weight gain. Moderation in drinking is still advised, as is a sensible diet that does not promote weight gain[xvi].
Genetic variables can also determine a patient’s genetic tendency to gain weight due to alcohol consumption. Recent research suggests that genetic polymorphisms determine alcoholism susceptibility and may also alter body weight underlying gene-related changes in fuel utilization[xvii]. As per the researchers, the genotype of the alcohol dehydrogenase-1B (ADH1B) gene (rs1229984) is a good predictor of body weight in addicts. Ethanol would be used less efficiently as an energy source due to the ADH1B*2 particular genetic quicker ethanol excretion10. Based on the results, more research is needed to completely study the genetic components of the link connecting alcoholic use and weight gain.
Obesity is a multi-factorial condition, making it difficult to determine the impact of alcohol use on obesity risk on its own. The experimental results are hampered by the short follow-up duration and the difficulty of controlling for all lifestyle habits in physiological circumstances. In contrast, quantitative results are hampered by the possibility of observational studies by unmeasured parameters. It’s tough to demonstrate a cause-and-effect relationship between alcohol usage and weight gain because of obesity’s slow transition and multidimensional character[xviii]. As a result, we must rely on relatively brief intervention trials and statistical research, both of which have severe limitations in proving the impact of alcohol on muscle mass sensitivity4. However, a growing body of evidence demonstrates that alcohol may be a growing health problem in some persons, especially when consumed in large amounts. Because of the quantity and form of alcohol consumed by men, the relationship involving alcohol consumption and body weight is frequently stronger in men than in women. Alcohol is claimed to constitute 16 percent of the overall drinkers’ total energy consumption in the Country, with males, drink nearly three times as much as females2. Men are also more inclined to drink beer with a higher starch content and provide more energy per standard drink than wine. This conclusion is backed up by the findings of a thorough study overview, which found positive associations between beer consumption and measures of abdominal adiposity (commonly known as “beer belly”) in males but mixed results in women3.
Another key complicating element to consider is one’s degree of physical exercise. Even though an increase in energy output may offset increases in energy intake caused by alcohol drinking, much epidemiologic research fails to consider lifestyle factors like physical activity and sedentary behaviours13. In addition, beer and spirit drinkers appear to have poorer eating patterns than wine drinkers. Both sides of the balance equations (lifestyle, expenditure, and intake choices) must be considered when examining the link between alcohol consumption and obesity. Sleep deprivation has also been linked to increased alcohol use and excess body weight amongst adults1. People who sleep just under 6 hours a night are more likely to consume more alcohol, have a higher BMI and are more expected to exceed the recommended alcohol intake14. In addition, we discovered that a combination of insufficient sleep and unregulated eating behaviour is connected to increased consumption of alcohol and water retention[xix]. These findings highlight the role of identifying high-risk individuals (for example, signal degradation short sleepers) who require additional preventive actions3.
Obesity and Smoking
According to several studies, cigarette smokers had a lower BMI (in kg/m2) than moderate drinkers. There was no populace in which chain-smokers had a greater Propensity than people who smoke. The cigarette had no influence on hunger symptoms in smokers or secondhand smoke[xx]. However, it did cause daily caloric consumption during meals to decrease. Ultimately, smoking appeared to have an acute inflammatory effect that encourages weight loss, although the impact on caloric is ambiguous1.
Strengths and Limitations
The main strength of this study is large-scale GWAS data was used for the MR analysis. Other strengths are as follows:
- The large sample size allowed for a reliable causal effect estimation, assessing the consistency of associations across different MR methods.
- The MR approach reduces bias due to reverse causality and confounding.
- Reverse causality is minimized in MR studies because the disease cannot modify genotype, fixed at conception.
The disadvantages of this study are as follows:
- We only used the data from individuals of European descent; we should be cautious about generalizing our findings to other populations.
- Limited availability of population-specific information on genetic associations, genetic instruments tend to show poor statistical power.
CONCLUSION
We discovered that overweight is substantially associated with coronary heart disease risk, gestational weight gain, and a lower smoking risk in European populations using two-sample Mendelian randomization. These findings imply that an individual’s attitude plays a major impact in predicting illness risk or future health issues. Our results are significant because we established the impact of personality traits on an unhealthy lifestyle by studying people in the regular populace rather than individuals living with alcohol addiction. As a result, the present study has demonstrated the necessity for tailored therapy to detect and prevent illness formation based on a person’s characteristics.
References
[i] Noor, N. M. (2010). Overweight, Smoking and Self-Esteem Among Adolescents in Malaysi. Lap Lambert Academic Publishing GmbH KG.
[ii] Zheng, J., Baird, D., Borges, M. C., Bowden, J., Hemani, G., Haycock, P., . . . Smith, G. D. (2017). Recent developments in Mendelian randomization studies. Current epidemiology reports, 4(4), 330-345. Retrieved from https://link.springer.com/article/10.1007%2Fs40471-017-0128-6
[iii] Malcolm K Robinson, A. T. (2006). Obesity and Cardiovascular Disease. CRC Press.
[iv] Ades, P. A., & Savage, P. D. (2017). Obesity in coronary heart disease: An unaddressed behavioral risk factor. Preventive medicine, 104, 117-119. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5640469/
[v] Dale, C. E., Fatemifar, G., Palmer, T. M., White, J., Prieto-Merino, D., Zabaneh, D., . . . McLachlan, S. (2017). Causal associations of adiposity and body fat distribution with coronary heart disease, stroke subtypes, and type 2 diabetes mellitus: a Mendelian randomization analysis. Circulation, 135(24), 2373-2388. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5515354/
[vi] Hemani, G., Zheng, J., Elsworth, B., Wade, K. H., Haberland, V., Baird, D., . . . Tan, V. Y. (2018). The MR-Base platform supports systematic causal inference across the human phenome. elife, 7, e34408. Retrieved from https://elifesciences.org/articles/34408
[vii] Sanderson, E., Smith, G. D., Windmeijer, F., & Bowden, J. (2019). An examination of multivariable Mendelian randomization in the single-sample and two sample. International journal of epidemiology, 48(3), 713-727. Retrieved from https://academic.oup.com/ije/article-abstract/48/3/713/5238110
[viii] Zhao, Q., Wang, J., Hemani, G., Bowden, J., & Small, D. S. (2020). Statistical inference in two-sample summary-data Mendelian randomization using robust adjusted profile score. The Annals of Statistics, 48(3), 1742-1769. Retrieved from https://arxiv.org/abs/1801.09652
[ix] Lavie, C. J., Arena, R., Alpert, M. A., Milani, R. V., & Ventura, H. O. (2018). Management of cardiovascular diseases in patients with obesity. Nature Reviews Cardiology, 15(1), 45-56.
[x] Kannel, W. B., d’Agostino, R. B., & Cobb, J. L. (2016). Effect of weight on cardiovascular disease. The American journal of clinical nutrition, 63(3), 419S-422S. Retrieved from https://academic.oup.com/ajcn/article/63/3/419S/4651460?login=true
[xi] Elagizi, A., Kachur, S., Lavie, C. J., Carbone, S., Pandey, A., Ortega, F. B., & Milani, R. V. (2018). An overview and update on obesity and the obesity paradox in cardiovascular diseases. Progress in cardiovascular diseases, 61(2), 142-150.
[xii] Piché, M. E., Tchernof, A., & Després, J. P. (2020). Obesity phenotypes, diabetes, and cardiovascular diseases. Circulation research, 126(11), 1477-1500
[xiii] Burgess, S., Smith, G. D., Davies, N., Dudbridge, F., Gill, D., Glymour, M., . . . Theodoratou, E. (2019). Guidelines for performing Mendelian randomization investigations [version 1; peer review: 1 approved, 1 approved with reservations]. Retrieved from https://doi.org/10.12688/wellcomeopenres.15555.1
[xiv] Barry, V. W., Caputo, J. L., & Kang, M. (2018). The joint association of fitness and fatness on cardiovascular disease mortality: a meta-analysis. Progress in cardiovascular diseases, 61(2), 136-141
[xv] Larsson, S. C., Bäck, M., Rees, J. M., Mason, A. M., & Burgess, S. (2020). Body mass index and body composition in relation to 14 cardiovascular conditions in UK Biobank: a Mendelian randomization study. European heart journal, 41(2), 221-226. doi:10.1093/eurheartj/ehz388
[xvi] Fountain, B. J., & Komm, A. R. (2017). Relationship Between Alcohol Consumption, BMI, and Weight Perception in Women Aged 20-29 Years. MSSTATE.
[xvii] Kasper, P., Martin, A., Lang, S., Kütting, F., Goeser, T., Demir, M., & Steffen, H. M. (2021). NAFLD and cardiovascular diseases: a clinical review. Clinical Research in Cardiology, 110(7), 921-937
[xviii] Davies, N. M., Holmes, M. V., & Smith, G. D. (2018). Reading Mendelian randomisation studies: a guide, glossary, and checklist for clinicians. Bmj, 362. doi:10.1136/bmjk601
[xix] Minelli, C., Del-Greco, M. F., van-der-Plaat, D. A., Bowden, J., Sheehan, N. A., & Thompson, J. (2020). The use of two-sample methods for Mendelian randomization analyses on single large datasets. bioRxiv. doi:10.1093/ije/dyab084
[xx] Lee, W., Hwang, S. H., Choi, H., & Kim, H. (2017). The association between smoking or passive smoking and cardiovascular diseases using a Bayesian hierarchical model: based on the 2008-2013 Korea Community Health Survey. Epidemiology and health, 39
 write
write