Introduction
Depression is one of the most common mental illnesses globally and the third cause of disability. Additionally, it is among the leading causes of death among mental illnesses. Adolescents account for 14% of all access to depression, and the rates of suicide are high in the group (Mullen, 2018). Understanding the nature of depression and the treatment process is crucial for participating actively in treatment. This paper presents all the essential information about depression to the patients, families and caregivers of adolescents with depression.
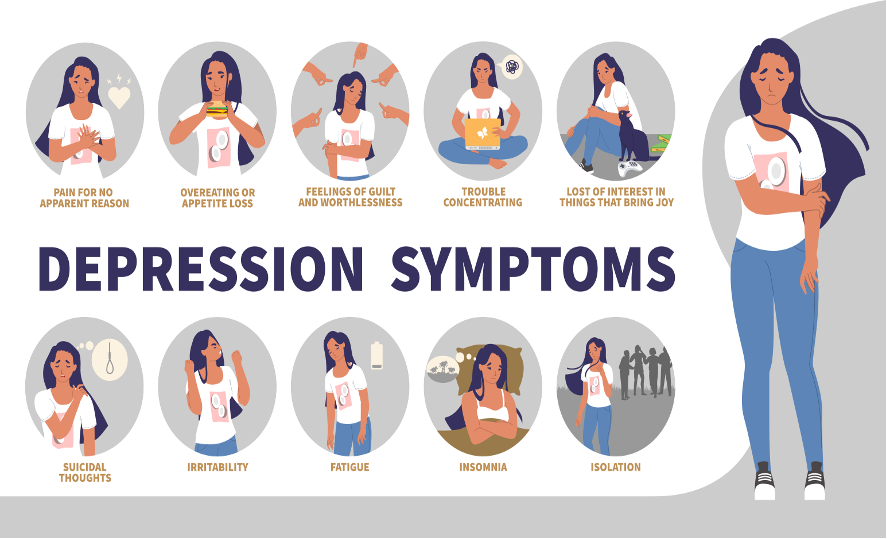
Depressive Disorder Causes and Symptoms
Depression is a type of mental illness that causes a low mood and loss of interest in things that initially sparked interest in the affected victim. While there is no identifiable cause for depression, there are some theories that scientists have devised to attempt to explain how depression occurs (Bains & Abdijadid, 2023). One of the most accepted theories is the imbalance of chemicals in the brain called neurotransmitters like serotonin and norepinephrine (Rikard-Bell et al., 2022). For that reason, the antidepressants that have been devised target mainly maintaining the normal levels of these chemicals.
Depressed people display a significantly low mood that is accompanied by a loss of interest in virtually everything. They are accompanied by low self-esteem, worthlessness, loss of hope, and inability to have fun (Mullen, 2023). A small proportion of people would experience hallucinations, delusions, and suicidal ideas, which is common in cases of severe depression. Furthermore, some people start isolating and report loss of energy, changes in appetite, slow thinking, and motor movements (Bains & Abdijadid, 2023).
Diagnosis of Depression among Adoslcenets
The diagnosis of depression is usually made based on the presenting symptoms and their duration using criteria as guided by the manual of diseases called DSM-5. The manual gives all the requirements that are essential for a diagnosis of depression to be made (Bains & Abdijadid, 2023). According to the DSM-5 manual, people with depression must have the following: low mood and loss of interest. The two should be accompanied by at least some of the following manifestations: loss of hope, feelings of worthlessness, appetite changes, change in sleep, and experiences of hallucinations, delusions, or suicidal ideations (Mullen, 2018).
| Question | Yes/no |
| Do you have a low mood | |
| Have you lost interest in things? | |
| Has your sleep pattern changed | |
| Do you feel hopeless or worthless? | |
| Have you ever thought of suicide? | |
| Has your appetite changed | |
| Has it lasted for more than one month? |
Adolescents account for 14% of all depression cases diagnosed, according to WHO. The adolescent stage is usually crucial in developing social and economic skills that are relevant in life, making it essential (Mullen, 2018). Depression among adolescents can be predisposed by experiences like drug abuse, violent sexual encounters, harassment, and cyberbullying (currently), among other experiences. To make it worse, the group is still developing and lacks the life skills to deal with complex experiences. Furthermore, they do not have health-seeking behaviour, making them suffer in silence (Sheffler & Abdijadid, 2023).
Medication Treatment Options
Treating depression relies on choosing medications that aim to restore the normal chemical levels in the brain, thus decreasing the symptoms of depression. There are seven groups of these medications, each working differently. The FDA has approved all of these classes for managing depression. Some target serotonin, norepinephrine, and enzymes for these chemicals; others are modulators (Mullen, 2018). However, those targeting serotonin and norepinephrine chemicals are recommended for adolescents due to their effectiveness and fewer side effects.
Fluoxetine and escitalopram belong to these classes and have been approved by the FDA for the treatment of depression in adolescence due to their excellent outcomes. The significant benefits of the two medications include their effectiveness in managing depression in the group (Mullen, 2018). Some of the risks associated with them include side effects like suicidal ideations, problems in the digestive system like diarrhoea and vomiting, possible allergies, changes in sexual function, increased appetite, and weight changes (Rikard-Bell et al., 2022).
| Drug | How they work |
| Selective serotonin reuptake inhibitors (SSRIs)
|
Restore normal levels of the chemical serotonin |
| Serotonin-norepinephrine reuptake inhibitors
|
Restore normal levels of the chemical serotonin and norepinephrine. |
Medication Considerations of Examples Prescribed

The medications present in the list belong basically to three distinct groups: tricyclic antidepressants, selective serotonin reuptake inhibitors, and serotonin-norepinephrine reuptake inhibitors. I would choose those targeting serotonin and norepinephrine (SSRIs and SNRIs) for the adolescent. Most drugs have similar risks, side effects, benefits, and suitability. Tricyclic antidepressants produce sedation and thus must be used cautiously for adolescents who are operating automobiles as they risk accidents. Secondly, when using them, doctors start with a low dose and gradually increase it until it suits the adolescent needs. Thirdly, it is crucial to measure heart rhythm since the drugs can badly affect the heart rate or rhythm (Rikard-Bell et al., 2022). It is also crucial to inform the physician of emerging drug side effects (Bipeta, 2019).
The class of SSRIs and SNRIs requires close monitoring of patients taking them due to suicidal ideations. Secondly, it is essential to let the doctor know that if the patient drives an automobile, the drugs can increase the risk of accidents due to sedation. Third, some drugs can interact and produce unwanted effects with these drugs, and thus, it is critical to inform the doctor about them, including ibuprofen (Mullen, 2018). For all agents, monitor for any suicidal ideations.
Important laboratory and comorbid issues to monitor
Depression is a mental illness that cannot be tested in blood or any other components of the body to diagnose it. However, various disorders in the human body can potentially predispose one to develop depression. It is a requirement that these disorders are ruled out before making a diagnosis of depression. Some of these disorders include drug abuse, hormonal imbalance and medication use, among others (Mullen, 2018). Therefore, some standard behavioural parameters to monitor include drug and hormone levels. However, evaluating the kidney and liver function is crucial because these drugs are broken down and exacerbated by the liver and kidney, respectively. Any problems with the kidney or liver would warrant dose changes.
Depression usually has various disorders that can predispose someone to develop them. The majority of the patients with major depression also have anxiety disorders and compulsive disorders. Additionally, people with depression occasionally have suicidal ideation, which can be translated into suicidal attempts (Rikard-Bell et al., 2022). Therefore, it is crucial to monitor their behaviour to prevent them from committing suicide. Lastly, people with depression also have a higher likelihood of drug abuse and thus must be continually assessed.
Special Considerations
Tricyclic antidepressants risk toxicity compared to the other agents used in the management of depression and thus must always be used when the other drugs have been deemed to be effective. On the other hand, SSRIs are generally not advised for adolescents less than 18 years old due to the possibility of severe suicidal ideations unless under caution. Similarly, due to the same risk, SNRIs should be used cautiously in the age group (Sheffler & Abdijadid, 2023). Prescribing drugs to adolescents poses numerous ethical, legal, and cultural considerations that must be followed.
Generally, an adolescent under the age of 18 years cannot afford treatment with antidepressants and thus should only receive the medication after the parents have been duly informed of the diagnosis and have connected (Michaud et al., 2023). Even after prescription, there has to be a unique way of monitoring adolescents to take medication because they have low defence to medications. Throughout the process, the healthcare professional will strictly adhere to ethical principles like respect, doing good, preventing harm, and confidentiality (Bipeta, 2019).
Culture influences various depression-related factors; thus, the patient and healthcare professionals must discuss the various issues (Bipeta, 2019). For example, some cultures believe that mental illnesses are curses and thus would seek religious interventions for the problems. In such cultures, therefore, adherence to antidepressant medication can be a significant problem. On the other hand, various socioeconomic factors can also influence the process of treating depression (Michaud et al., 2023). For example, in a low-income family, it is tough for them to afford antidepressants due to a lack of insurance coverage or money to pay for these services.
Community follow up
The community is one of the most crucial settings for addressing mental health services because of the proximity to where people live. They form an essential network for increasing the awareness of mental illnesses globally. Some areas where a person can gain information on mental health include community health centres and clinics.
Examples of how to write a prescription
Drug prescriptions for all controlled substances like antidepressants must have the name of the patient, age, sex, location, and address. Furthermore, it must bear the drug name, strength, dose, duration, formulation, and quantity. Lastly, it must bear the prescriber’s name, qualification, hospital, and date.
Examples 1
- No: 127272/2023
Name: Patient T.U Age: 17 years
Sex: Male Location: New York City
Address: 231-00 Highway Street
Drug: escitalopram
Strength: 10mg/tablet
Dose: 10mg
Frequency: once daily
Preferred time: night
Duration: 30 days
Quantity: 30 tablets
Instructions: Avoid driving, report any allergies, and take preferably at night
Prescriber: D. D. Qualification: APNP Date: 12/12/2023
Examples 2
- No: 12734/2023
Name: Patient D.L Age: 15years
Sex: Female Location: New York City
Address: 231-0044 Highway Street
Drug: Fluoxetine
Strength: 20mg/tablet
Dose: 20mg
Frequency: once daily
Preferred time: night
Duration: 30 days
Quantity: 30 tablets
Instructions: Avoid driving, report any allergies, and take preferably at night
Prescriber: R.Y. Qualification: Psychiatrist Date: 12/12/2023
Examples 3
- No: 127272/2023
Name: Patient L.P Age: 17 years
Sex: Male Location: Minnesota
Address: Municipal 230-22 street
Drug: escitalopram
Strength: 10mg/tablet
Dose: 20mg
Frequency: once daily
Preferred time: night
Duration: 30 days
Quantity: 30 tablets
Instructions: Avoid driving, report any allergies, and take preferably at night
Prescriber: D. D. Qualification: APNP Date: 12/12/2023
Conclusion
Depression is a severe mental illness that needs treatment and monitoring for all those who are affected. Despite it affecting anyone, adolescents are among the most vulnerable populations. Depression predominates majorly with mood changes and loss of interest accompanied by various other symptoms. Its treatment is mainly done by drugs that restore normal transmitter levels in the area. Adherence to these drugs is critical towards recovery. However, it is vital to consider various risks and benefits related to the drug before prescribing.
References
Bains, N., & Abdijadid, S. (2023, April 10). Major Depressive Disorder. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK559078/
Bipeta, R. (2019). Legal and ethical aspects of mental health care. Indian Journal of Psychological Medicine, 41(2). https://doi.org/10.4103/ijpsym.ijpsym_59_19
Michaud, P.A., Takeuchi, Y.-L., Mazur, A., Hadjipanayis, A. A., & Ambresin, A.-E. (2023). How to approach and take care of minor adolescents whose situations raise ethical dilemmas? a position paper of the European Academy of Pediatrics. Frontiers in Pediatrics, 11, 1120324. https://doi.org/10.3389/fped.2023.1120324
Mullen, S. (2018). Major depressive disorder in children and adolescents. Mental Health Clinician, 8(6), 275–283. https://doi.org/10.9740/mhc.2018.11.275
Rikard-Bell, C., Hunt, C., McAulay, C., Hay, P., Morad, A., Cunich, M., & Touyz, S. (2022). Adolescent Depression from a Developmental Perspective: The Importance of Recognizing Developmental Distress in Depressed Adolescents. International Journal of Environmental Research and Public Health, 19(23), 16029. https://doi.org/10.3390/ijerph192316029
Sheffler, Z. M., & Abdijadid, S. (2023). Antidepressants. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK538182/

 write
write