Introduction
Malaria remains one of the biggest public health problems in contemporary society. Notably, it is a big issue in many low-income states, which need more resources for its control. One low-income country that is highly affected by Malaria is Nigeria, and thus, it is chosen as the country of focus in this assignment. Nigeria is considered a low-income country, and here, it is used to give a rough general picture of the transmission and burden of Malaria in sub-Saharan Africa. Understanding malaria epidemiology has become necessary with the heightened need for control. A structured investigation of the outbreak through analysis of the factors will help to find out the causes contributing to its occurrence and make recommendations for workable interventions to reduce the impact on public health and enhance malaria control.
Epistemological features of Malaria
Figure 1: Malaria parasites (Chukwuzurum et al., 2021)
Malaria is one of the chief human vector-borne diseases caused by the genus Plasmodium (Oladepo et al., 2019). The main aspects of this disease include factors related to the types of Plasmodium-causing infections, characteristics of vector mosquitoes involved, environmental conditions, and human behavior; these all interact in the human-mosquito environment and affect malaria transmission (Chukwuzurum et al., 2021).
Transmission is mainly through a bite from an infected female Anopheles mosquito, through which sporozoites are injected into the human bloodstream during feeding (WHO, 2021). The Plasmodium genre regarding human species forms four primary species: Plasmodium falciparum, Plasmodium vivax, Plasmodium malaria, and Plasmodium ovale, with P. falciparum being the most lethal (Talapko et al., 2019).
On the other hand, malaria transmission may show a clear seasonality, most often with a peak period during the rainy season and an expansion in mosquito breeding sites. In some parts of endemic countries like Nigeria, however, year-round transmission occurs, especially in the areas with constant transmission of Malaria (Oladipo et al., 2022).
Malaria symptoms are mostly present through a clinical diagnosis and may result in fever, chills, headaches, muscle aches, and fatigue. In severe cases where the disease is more likely to be complicated, it may also worsen its effects into cerebral Malaria, severe anemia, or organ failure in children, pregnant women, or those with weakened immunity (Fornace et al., 2021).
The people of this population live in a malaria-endemic area, and therefore, the most significant burden is brought about by Malaria in mortality and morbidity (Effiong et al., 2022). The high persistence of Malaria in transmission is brought about by factors such as poverty, health care access, and proper housing, as well as ecological factors like deforestation and poorly managed irrigation.
Prevention efforts aim to control Malaria through vector control by using insecticide-treated bed nets and indoor residual spray, preventive interventions in high-risk groups with improved chemoprevention, timely diagnosis and treatment, and community involvement on the way forward to develop sustainable control strategies (Oboh et al., 2021). Some obstacles that hinder any remarkable progress in malaria control efforts are drug-resistant parasites and vector resistance to insecticides, among other challenges such as climate change.
Country Selection
For this hypothetical outbreak investigation, Nigeria, which is a low-income country in sub-Saharan Africa, will be the center of focus. The country has a significantly high population with strained resources for healthcare provision and is thus heavily burdened by the epidemic.
Structured Outbreak Investigation
Review of Surveillance Data: It will involve a detailed review of the surveillance data from the Ministry of Health in Nigeria concerning the number of reported cases, geographical distribution, analysis, and statistics of the demographic characteristics of the affected, including temporal trends (Omale et al., 2021). The analysis would guide identifying how vast and severe the outbreak has been and enhance pattern recognition.
Field Investigation: This will entail identifying the affected areas concerning surveillance information. Public health officials and experienced epidemiologists visit the areas to assess local environmental conditions, mosquito breeding places, and community practices, specifically malaria prevention and control (Chukwuzurum et al., 2021). This initiative may be achieved by inquiring community members, humans, or administrative staff about recent cases, exposures, environmental hazards, and possible control measures.
Case investigation: This is done through a case and caregiver interview to gather information concerning the symptoms when the symptoms started, recent travel history, use of methods of prevention like bed net use if one uses insect repellents, and if one is exposed to mosquito bites in areas with a confirmed case (WHO, 2021). Contact tracing is also done to trace people exposed to the parasite through close contact with a confirmed case.
Entomological survey: Maximum liaison between an entomologist and vector control expert should be present during the entomological survey. The entomological survey should determine the density of mosquito vectors, species found, and insecticides the mosquito vectors are susceptible to (Garrido-Cardenas et al., 2019). This is done by collecting mosquitoes from selected habitats, which are known to include breeding females, sentinel sites, and houses for species identification, determining the susceptibility of mosquito populations to insecticides, and assessing vector behaviors. Data obtained during entomological surveys present critical information regarding malaria transmission dynamics and provide information relative to vector control malaria.
Laboratory Testing: The laboratory tests for confirmation of a malaria diagnosis involve identifying species of malaria parasites and possible resistance to Malaria (Oboh et al., 2021). Proper diagnosis and surveillance of Malaria through an appropriate laboratory in situations where the required amenities include accurate microscopes, quick diagnostic tests, and molecular techniques. Therefore, timely and effective laboratory diagnosis is to be done before the administration of drugs and during the period of monitoring trends in drug resistance (Talapko et al., 2019).
Factors Potentially Involved in Malaria Occurrence
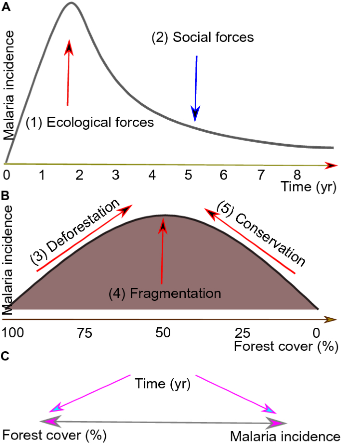
Figure 2: Potential factors involved in the spread of Malaria (Fornace et al., 2021).
Environmental Changes: These include various activities, such as deforestation from human habitation, urbanization, and irrigation efforts that contribute to the breeding sites of the vector that may bring about the potential transmission of Malaria; these have been observed in Nigeria. Stagnant water areas and taboo changes in land use are also possible in many other forms that increase this number, creating a hazard for malaria transmission (Oladipo et al., 2022).
Climate Variability: Temperature conditions are evident in determining breeding cycles and patterns of rainfall, but they also influence the geographical spread of malaria infections by mosquitoes (Omale, 2021). Variations and conditions, like very heavy and long rainy seasons or temperature variations, will favor reproduction and the gradual growth of malaria parasites through mosquito multiplication (Oladepo et al., 2019). As such, weather changes will contribute significantly to the outbreak of Malaria.
Population movement: Human migration, travel, conflict, or disaster-related displacement of populations due to their movement may spread malaria parasites to new areas within the country or promote the transmission of drug-resistant strains (Omale et al., 2021). The net movement of infected people from the endemic area to the non-endemic regions increases the risk of transmission. It neutralizes efforts put in by way of surveillance and control.
Vector Adaptation: A significant threat to malaria control in the country is vector adaptation, mainly due to Anopheles mosquito resistance to the insecticides applied in interventions (WHO, 2021). Repeated application of insecticides, without the rotation of chemical classes of insecticides, may exert selective pressure on mosquito populations and eventually develop a resistant genetic makeup that results in losing control.
Socio-cultural Practices: The practice of behaviors like outdoor activities at critical times of mosquito biting, perceptions about malaria transmission in general, and prevention, in particular, can influence the incidence of the disease (Fornace et al., 2021). At the same time, cultural beliefs and practices play a role in compliance with preventive measures and health-seeking behaviors impacting malaria control outcomes.
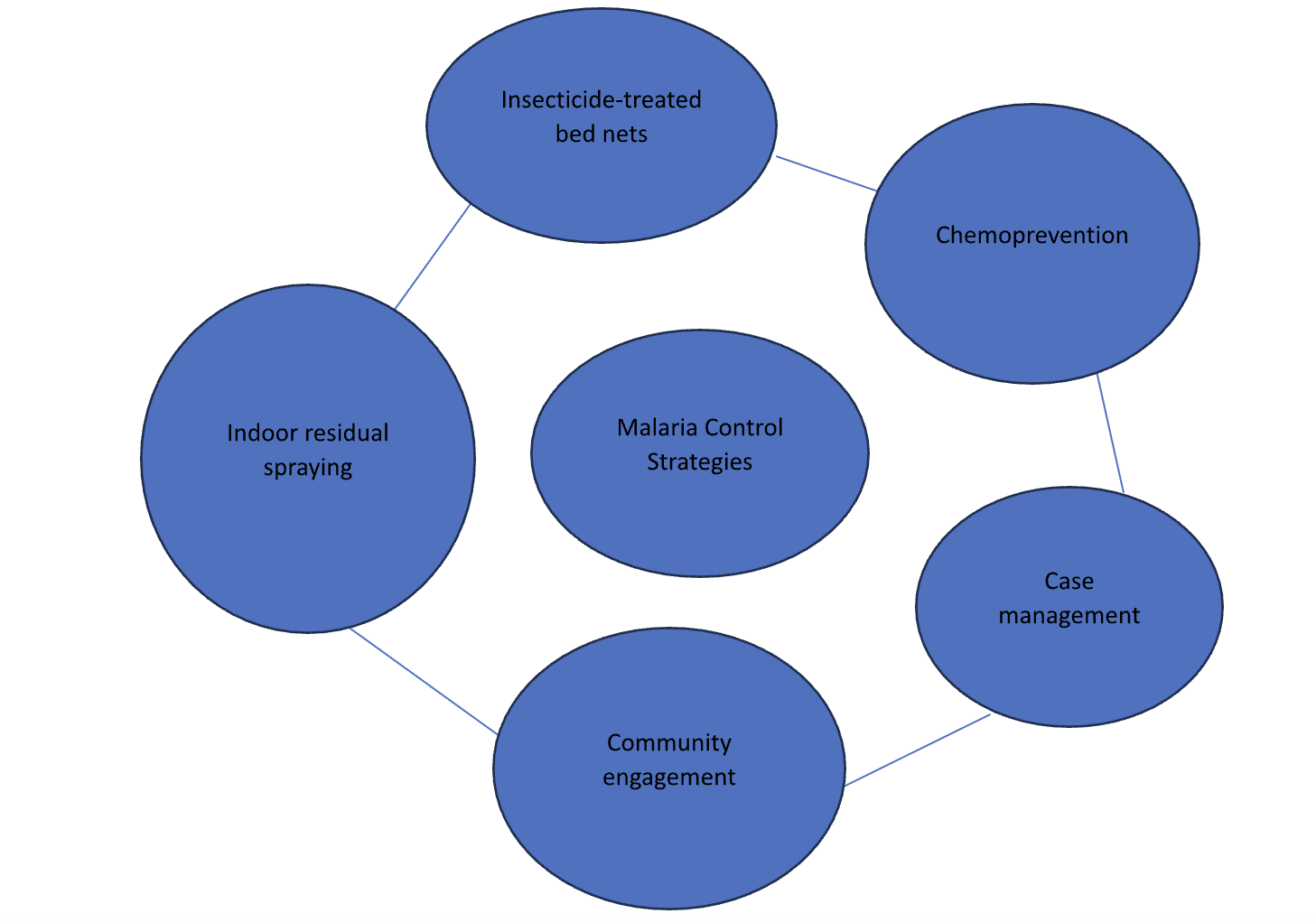
Conceptual Model of Disease Control Strategies
Critical Discussion and Comparison of Control Strategies
Insecticide-treated bed nets: Even though it has proved to be a significant factor in reducing patient-vector contact, this method is still characterized by problems like coverage and usage, among many others. Issues of access and use of bed nets, the proper use required, and the timely replacement of worn-out nets all work as obstacles to their impact on transmitting Malaria (Garrido-Cardenas et al., 2019). Moreover, bed nets become less effective with time due to wear and tear or insecticide resistance, making constant monitoring and distribution efforts necessary.
Indoor Residual Spraying: In addition, indoor residual spraying causes mosquito populations at rest indoors to be killed. It might not translate to a reduction in transmission as the approach used is not sustainable given that it is often required and might involve cases of resistance (Omale, 2021). All such environmental concerns need to be met, especially where insecticides need to be used, but ensuring long-term sustainability is very necessary beyond that.
Chemoprevention: Prophylactic use of anti-malarial chemoprevention accrues enormous benefits in the reduction of disease burden, more so among vulnerable populations. Some of these interventions, however, need help conferring a guarantee to assure this adherence, with infrequent dosing and monitoring of their adverse effects in resource-constrained settings, possibly due to inadequate infrastructural support (Effiong et al., 2022). Furthermore, resistance development has been said to reinforce further the absolute requirement for adherence to standard drug regimens and drug resistance surveillance.
Case management: The early diagnosis of a case and treatment with an effective anti-malarial drug are the cornerstones to the depreciation of sequelae to the patient and interruption of transmission (Omale, 2021). However, the availability of health care, accurate diagnosis, good quality, and working drugs remain perennial issues of concern in Nigeria. Effective case management requires strengthening the health system to help boost diagnostic capabilities and drug supply chains, among other things, in healthcare delivery infrastructure.
Community engagement: There is a need to ensure the community is effectively engaged, for it is the ultimate basis for any effective control of Malaria since behavior change will eventually be translated into good practices that bring consistent results for vector control and contribute to health education (Chukwuzurum et al., 2021). Community-led activities empower local populations by giving them a modicum of control over measures put into place to the extent that ownership is felt.
Prioritization of Investigation Factors
Vector Control Interventions: Anopheles mosquitoes are relevant vectors of malaria parasites, so those recommendations stress the critical need for entomological evaluations of the interventions to control these, in relevance to both insecticide-treated nets and programs on indoor residual spraying (Omale, 2021). Directly affected is consonant with the vectors that are transmitting the disease, which reduces the contact between humans and mosquitoes significantly and, in so doing, breaks the cycle of disease transmission. The interventions sought to establish that increased ownership and usage of ITNs and IPTp services and improvement in practices within the case management system indeed made a difference in the incidence of Malaria (Oladepo et al., 2019). Besides, these control measures are also crucial in monitoring insecticide resistance patterns in mosquito populations to ensure continued effectiveness.
Access to comprehensive quality health services: Identifying and working on critical barriers to ensure timely diagnosis and access to treatment, especially in rural areas or marginalized populations where adequate healthcare infrastructure could not be a letdown (Effiong et al., 2022). The challenge of late diagnosis of Malaria, delayed access to tools for diagnosis, anti-malarial drugs, and professional health workers continues to stand in the way of proper management of Malaria, allowing for increases in morbidity and mortality. Such are the guarantees, with access to other public services, interventions such as mobile clinics, community health workers, and telemedicine initiatives, to see strategies for effectively delivering malaria services to the population living in remote areas, reducing the disease burden.
Social-Economic Determinants: Social-economic factors that significantly influence the risk of Malaria include poverty, education level, and house quality. Understanding how these determinants act in diseases can guide targeted interventions toward modifying the underlying social inequalities (Omale, 2021). These include the improvement of education and information about prevention, which is more likely to be implemented by the community, and the improvement of housing construction so that less habitat is present for mosquitoes to breed in. It thus re-emphasizes the socio-economic-driven character of looking into the causes of Malaria to enable a whole system of interventions targeting both the immediate causes of malaria transmission and the root causes of health disparities against preventable infections within affected populations (Oladepo et al., 2019).
Advising the MoH on Control Measures
Strengthen vector control: increase the distribution and promotion of ready-to-treat bed nets, improve indoor residual spraying coverage, and monitor insecticide resistance patterns—end of vector control.
Case management: Improve access to diagnostic testing and treatment with anti-malarial through diagnostic testing at clinics, mobile clinics, community health workers, and by using the telemedicine initiative.
Socioeconomic Drivers Address: Endemic malaria regions have related symptoms of poverty that must be attended to, meaning that maybe housing conditions must be reformed and education and public health access must be attended to.
Specific Goals for the MoH
Raise bed net coverage to a baseline of at least 80% of households within two years in high-endemic areas, a guarantee to reduce vector-human contact during the sleeping hours when transmission occurs (Effiong et al., 2022). Through prioritization in the distribution and promotion of the use of long-lasting insecticidal nets, especially in high malaria burden regions, the Ministry of Health does, therefore, achieve its intervening area of protecting vulnerable persons against mosquito bites and consequently reduces incidences of Malaria (Oboh et al., 2021).
The formation of mobile testing and treatment units assures that at least 90% of the affected will be provided with a correct diagnosis and treatment. Prompt and proper diagnosis and treatment epitomize the strategy for reducing morbidity and mortality from Malaria (Oladepo et al., 2019). This includes deploying wholly equipped mobile clinics to rural and such areas with low coverage of diagnostic tests and anti-malarial services.
Support for community-directed initiatives aimed at socioeconomic determinants of the risks of initiating Malaria (Oladepo et al., 2019). The spread of Malaria is associated with socioeconomic factors: poverty, poor housing, a lack of education, and inadequate health care all result in increased risks. Community-based interventions that seek to better and improve conditions related to sanitation and housing can be ways toward eradicating the basis for malaria transmission and, with full empowerment, thereby effectively reducing its burden (Talapko et al., 2019).
Conclusion
Ultimately, the rapidly escalating burden of Malaria in low-income countries creates a call for multifaceted interventions, among which are the control of the vector, improved case management, and socioeconomic interventions. Given that, the Ministry of Health is then able to substantially reduce the burden of Malaria and improve public health in many other related ways through proper study of the problem areas and guidance toward concentrated interventions like upscaling bed net coverage, timely diagnosis and treatment, and the social determinants of health. The participatory approach in developing and implementing malaria control will allow Nigeria to integrate monitoring and evaluation within the system, putting Nigeria in the best position to lower the magnitude of the public health burden from Malaria.
References
Chukwuzurum, E. P., Daniel, E. O., Popoola, I. O., Abiodun, P. O., Bello, A. M., Amari, K. Y., & Ayeni, G. O. (2021). Malaria diagnosis and treatment: perceptions of community pharmacists in Abuja Metropolis, Nigeria. Int J Infect Dis Ther, 6(1), 6.
Effiong, F. B., Makata, V. C., Elebesunu, E. E., Bassey, E. E., Salachi, K. I., Sagide, M. R…. & Uwishema, O. (2022). Prospects of malaria vaccination in Nigeria: anticipated challenges and lessons from previous vaccination campaigns. Annals of Medicine and Surgery, 81.
Fornace, K. M., Diaz, A. V., Lines, J., & Drakeley, C. J. (2021). Achieving global malaria eradication in changing landscapes. Malaria journal, 20(1), 69.
Garrido-Cardenas, J. A., Cebrián-Carmona, J., González-Cerón, L., Manzano-Agugliaro, F., & Mesa-Valle, C. (2019). Analysis of global research on malaria and Plasmodium vivax. International journal of environmental research and public health, 16(11), 1928.
Oboh, M. A., Oriero, E. C., Ndiaye, T., Badiane, A. S., Ndiaye, D., & Amambua-Ngwa, A. (2021). A comparative analysis of four malaria diagnostic tools and their implications for malaria treatment in southwestern Nigeria. International Journal of Infectious Diseases, 108, 377–381.
Oladepo, O., Oyeyemi, A. S., Titiloye, M. A., Adeyemi, A. O., Burnett, S. M., Apera, I., & Alliu, M. (2019). Malaria testing and treatment knowledge among selected rural patent and proprietary medicine vendors (PPMV) in Nigeria. Malaria journal, 18, 1–8.
Oladipo, H. J., Tajudeen, Y. A., Oladunjoye, I. O., Yusuff, S. I., Yusuf, R. O., Oluwaseyi, E. M., & El-Sherbini, M. S. (2022). Increasing challenges of malaria control in sub-Saharan Africa: Priorities for public health research and policymakers. Annals of Medicine and Surgery, 81, 104366.
Omale, U. I. (2021). Knowledge, attitude, and practice of the National Guidelines for Diagnosis and Treatment of Malaria among medical doctors in Ebonyi State, Nigeria: A cross-sectional survey. Plos one, 16(9), e0257600.
Omale, U. I., Oka, O. U., Okeke, I. M., Azuogu, B. N., Alo, C., Madubueze, U. C.,… & Anene, O. C. (2021). Demand for malaria rapid diagnostic tests, healthcare-seeking behavior, and drug use among rural community members with fever or malaria-like illness in Ebonyi State, Nigeria: a cross-sectional household survey. BMC Health Services Research, 21(1), 857.
Talapko, J., Škrlec, I., Alebić, T., Jukić, M., & Včev, A. (2019). Malaria: the past and the present. Microorganisms, 7(6), 179.
World Health Organization. (2021). WHO malaria terminology.
 write
write