Introduction
Social workers are the most significant contributors to psychiatric health services in the United States of America. They help such patients manage their lives and social problems due to various mental disorders. According to Cox et al. (2019), they collaborate with other professionals such as psychiatrists, nurses, and psychologists to evaluate and provide necessary help to patients with mental diseases and behavioural issues. Despite the grave attention required to help this population, it is often underserved in society, including during conviction of crimes. Thus, the essay explores issues surrounding mental health patients and appropriate interventions to help them at the micro, mezzo, and macro levels.
At-risk Population
Mental health is a significant yet often overlooked aspect in healthcare. In most cases, the term is associated with “mad” and incompetent individuals in psychiatric hospitals. However, it includes a person’s emotional, social and psychological welfare. As such, it affects how people behave, think and feel (“What is mental health,” 2020). Clearly, mental health patients are diverse and thus require specialized attention. They vary from mild cases such as depression and anxiety to severe issues like bipolar disorders. I chose this population following the often generalized treatment for these patients. In most cases, health practitioners ignore the severity of symptoms and assume that the patient will get well after a particularly traumatic event fades away in their minds.
Moreover, some generalize treatment for different mental health patients despite their varying degrees of unwellness. Practitioners need to understand the various mental health issues and how they manifest differently in patients. As a result, they should individualize treatment for their patients. Also, mental wellbeing surrounding newly convicted individuals is an important aspect that needs to be addressed. Some cases involve crimes committed by mentally ill individuals. As a result, the court orders for psychiatric evaluation to avoid charging incompetent individuals. Such offenders are often jailed, awaiting these psychiatric tests that take a long time to be processed and presented. Therefore, these individuals suffer in prisons unethically awaiting trial.
Population Description
The mental health patients population is increasing daily in the United States of America. This populace is often unprivileged and discriminated, instead of receiving the necessary healthcare services required. Psychological disorders are pervasive in the country and include different disorders. According to the National Institute of Mental Health, approximately one in five American adults live with a psychiatric illness. As of 2019, mental illness patients amounted to 51.5 million (AMI) and 13.1 million (SMI) (NIMH, 2021). As mentioned earlier, mental illness varies with the severity and is often categorized as any mental illness (AMI) and serious mental illness (SMI).
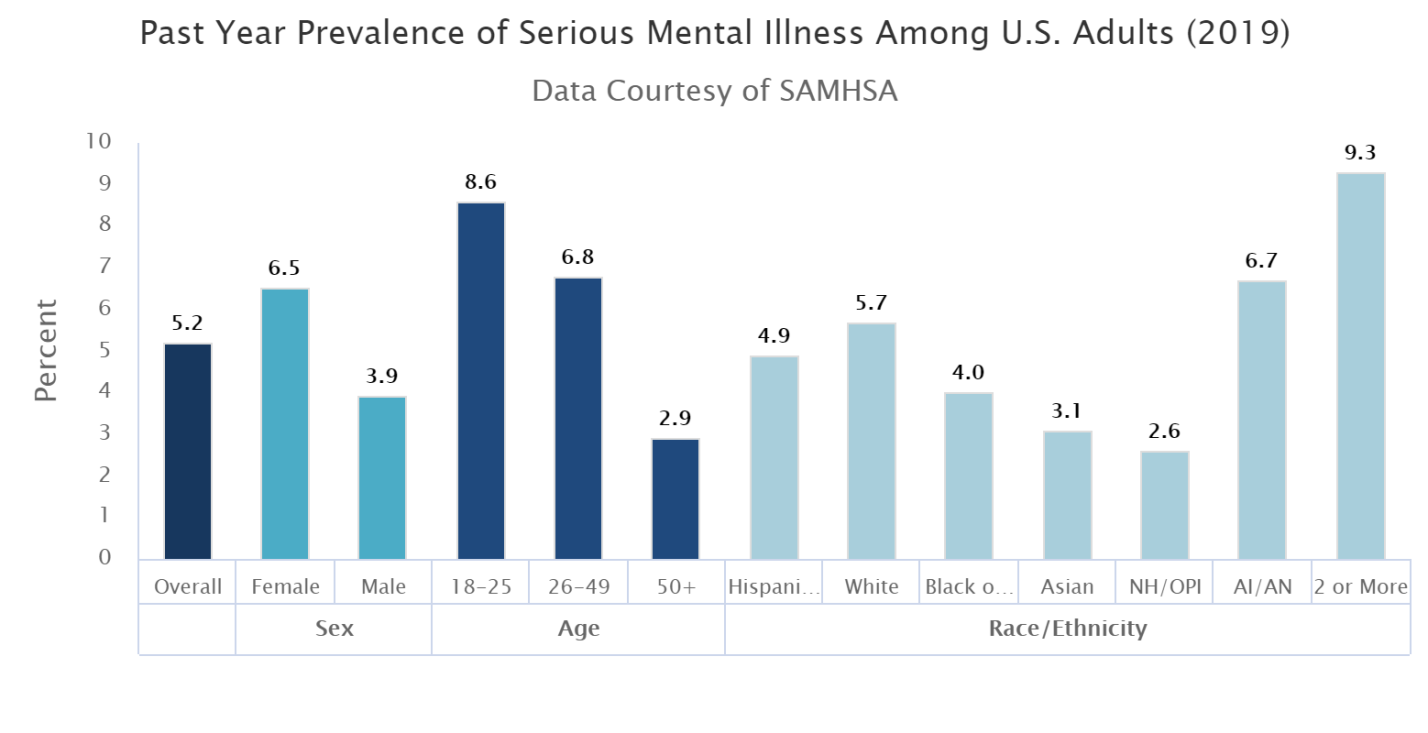
AMI differs with effects ranging from no injury to mild and moderate impairment and often involves behavioural, emotional, and mental conditions. The 2019 statistics illustrated that about 20.6% of American adults had AMI. However, females recorded a higher number (24.5%) than their male counterparts (16.3%). Moreover, AMI attacks younger people more than older ones. Figure 1 displays AMI prevalence among U.S individuals in 2019. On the other hand, SMI includes psychological, emotional, or behavioural conditions due to severe functional disabilities hindering or limiting an individual’s life activities. 2019 statistics approximate 13.1 million patients suffered SMI (5.2%). Similarly to AMI, more females suffer from SMI than men (6.5% and 3.9%, respectively). Figure 2 shows its prevalence among young adults being higher than the elderly.
Mental health in prisons is a serious issue that requires attention. It involves offenders in jails taking mental evaluation tests awaiting sentencing and already convicted mental health patients. The latter category ranges from criminals who suffer mental disorders due to their actions, such as drug abuse, and inmates who get mentally disturbed following their conviction and experience as inmates. Beynon and Drew (2005) point out that prisons are bad for mental health due to prison’s adverse factors such as overcrowding, bullying, and inadequate health services. Moreover, they serve as dumping sites for mentally ill patients. Some countries convict mentally disabled individuals for their lack of access to mental healthcare. These people include drug and substance users thrown into prisons instead of in psychiatric facilities.
The mental condition signs and symptoms may not be entirely obvious, and this may lead to stigmatization. Some of the less obvious symptoms include appetite changes, irritability, change in sleeping patterns, and loss of joy, among others. Prolonged symptoms require immediate medical attention to curb the issue before it gets out of hand. Some obvious symptoms may include intense memory loss, weight loss, other chronic disorders such as high blood pressure and low energy. These features should make it easy for an individual or a health practitioner to recognize a mentally ill patient and provides timely interventions.
Historical Experiences
Social workers are often at the forefront to help mental illness patients. Human relationships are fundamental to social workers and, thus, strive to engage with patients, their families, and the community (“Education policy and accreditation standards for Baccalaureate and Master’s social work programs,” 2015). Mostly, mental health patients are incapable of making informed choices and hence the need for family involvement. Furthermore, they require unprofessional help such as love and support from family and friends. Thus, the need for engaging other parties is fundamental. However, social workers need to distinguish cases that require third parties and those that require confidentiality to avoid breaching the patient’s right to autonomy and consent. The following peer-reviewed articles discuss different issues on mental illnesses and suitable interventions.
Mental illness stigma kills more than the disease. It comes from different sources such as family, individual or social factors. According to Silva et al. (2020), individuals delay seeking mental healthcare due to shame and fear of how society will view them. Others have a negative attitude and lack knowledge about mental healthcare and its importance. Therefore, the authors suggest awareness campaigns on mental wellness to encourage people to seek help immediately. Staff training is critical to help reduce and prevent stigmatization and stereotype associated with mental illnesses.
Lake’s and Turner’s article, “Urgent need for improved mental health care and a more collaborative model of care,” aims to improve the mental healthcare system to attend to complex mental disorder problems adequately. The authors explain that patients suffering from SMI, such as schizophrenia, often lack appropriate care models to help them. Therefore, there is a pressing need to adopt a collaborative care model and standard staff training to help improve the mental healthcare sector (Lake & Turner, 2017). This will, in turn, ensure patients get the required help on time to avoid adverse consequences.
Orjiakor et al. (2017) researched the effect of prolonged incarceration on wellbeing among awaiting trial prisoners (ATP). They explain that some offenders spend many years in detention waiting for trials and final verdicts from courts. Such individuals may be rendered innocent following the lack of evidence or new evidence that shows their innocence. However, such people may have spent almost one year in prison for a crime they did not commit. This affects their mental wellness as they witness other incarcerated inmates succumbing to mental illnesses following the pressures from bullying and guilt (Orjiakor et al., 2017). Thus, they call for practitioners to be more sensitive to this primarily neglected issue and impose alternative institutionalizing for these people.
As seen earlier, mental illnesses affect young people more than older adults. McLafferty et al.’s (2017) article focused on mental disorders among University students. It can be challenging for students to transition to university life due to the stress and challenges championed during lectures and examinations. This triggers mental illnesses among students, which may lead to suicides. The authors discovered that most students did not get the necessary treatment and did not think that emotional issues require professional help. As a result, they recommend learning institutions and parents to encourage help-seeking behaviour and advocate for anti-stigma campaigns to motivate students to seek mental healthcare help.
Mental illness patients can be health professionals too. Physicians, social workers, and nurses are often exposed to traumatic experiences that may trigger mental instability. However, most are unwilling to seek mental health treatment and care. According to Mehta’s and Edward’s (2018) research, approximately 35% of health practitioners do not get mental help despite the symptoms display. These choices are often a result of the stigma of mental disorders among the medical community and issues about licensure. As a result, suicide is higher among physicians than among the general population.
Unmet Needs of the Population
According to the literature, the healthcare sector does an excellent job of identifying and evaluating individuals who require mental healthcare services. However, the programs fail to sufficiently address complex issues such as bipolar disorders and schizophrenia. As a result, such patients suffer at the hands of capable professionals. Moreover, mental health issues are prevalent in prisons. ATPs suffer mental disturbances due to the prolonged detention as they wait for final sentencing, which sometimes takes years. These inmates experience the pressures of incarceration unlawfully as their status of guilt or innocence is pending. They are often neglected, and some may even succumb to the illness before knowing their fate.
Suicide rates are high in prisons, owing to the mental instability among inmates. Mentally ill patients require undivided attention and care to help them overcome the problem. However, most inmates are denied this right as they are viewed as criminals and a disgrace to society. Another unmet need is immediate medical help for mental illness patients due to stereotyping and stigmatization. It can be from the family, society, or healthcare providers. Some parents feel ashamed when they have a mentally disabled member and fail to help them seek medical help. Some patients fear stigmatization and prefer hiding in the closet, which worsens their situations.
Mental illnesses are common among university students, especially those reporting for the first year. The transition is challenging for many learners, which leads to stress, often aggravated during course lectures and exams. Such students fail to seek help as they think it is not a big deal. Others lack the knowledge and opportunity to acquire the needed help. Universities assume that the transition is not a serious one and that the students would adapt soon and overcome the mental anxiety on their own. Medical practitioners are also prone to mental illnesses due to the nature of their job. However, they do not seek help due to fear of professional consequences linked to disclosing the issue and stigmatization. For example, medical students dread getting professional help as it could affect their career advancement adversely. Hence, they end up committing suicide.
Interventions at the Micro, Mezzo, and Macro Levels
The several works of literature reviewed offer important interventions to help this at-risk population. The authors suggest improved standards of clinical training to improve mental healthcare promotion and quality. Each staff member interacting with the patients should know how to handle them in various emotional and mental states. Generally, a mentally unstable individual exhibits different behaviours under different circumstances. Thus, the entire workforce, including subordinate staff members, should know how to treat these patients right to avoid upsetting them.
Researchers about mental illness patients in prison suggest a diversion of these people towards the mental health system. The criminal justice system focuses on deterrence and punishment instead of treatment and care, making prisons unconducive environments for mentally ill inmates. Therefore, the need for legislation that permits the transfer of prisoners to psychiatric facilities at all criminal proceedings phases is fundamental. Moreover, those sentenced for minor charges should be taken to mental facilities to ensure they get the required help and reduce prisons’ overcrowding.
Moreover, staff training is critical to deal with mental illnesses inmates. Correctional officers, administrators, and healthcare providers should be educated on handling mentally ill prisoners to help offenders with major criminal offenses receive adequate care and treatment while serving their sentences. The training programs should aim to create awareness for human rights, understand the different mental conditions and discourage stigmatization. The programs should include suicide recognition and prevention as it mainly affects mental disorder inmates. Furthermore, they call for re-envisioning the existing care models by adopting a collaborative model delivery system in the primary care setting. The system involves conventional biomedical therapy and alternative treatment techniques.
The works of literature further suggest that education is essential to eradicate mental illness stigmatization. The appropriate education programs and measures for mental disorders stigma modify stereotypes, and as a result, replace them with facts and authentic information. These measures may include public service announcements, websites, and podcasts. Lastly, the researchers call for training among physicians to understand better mental illness as assimilated in medicine to encourage the medical community to destigmatize its viewpoint. They recommend reviewing the psychological health questions on state licensing boards to help health professionals overcome the licensure concerns due to disclosure of mental disorders.
Conclusion
Mental illnesses account for a large percentage of causes of death in America. This population is at-risk as many people overlook this as a serious issue that requires attention. Also, mentally ill patients shy away from seeking help due to stigma and shame. This includes medical practitioners, as they avoid stigmatization from the medical community. Mental health awareness, education, training, and campaigns are fundamental interventions to help this population get the required help at the right time to avoid AMI from graduating from SMI.
References
Beynon, J., & Drew, N. (2005). Mental health and Prisons. World Health Organization. https://www.who.int/mental_health/policy/mh_in_prison.pdf
Cox, L. E., Tice, C. J., & Long, D. D. (2019). Introduction to social work: An advocacy-based profession (2nd ed.). SAGE Publications.
Education policy and accreditation standards for Baccalaureate and Masters social work programs. (2015). Council on Social Work Education (CSWE). https://www.cswe.org/getattachment/Accreditation/Accreditation-Process/2015-EPAS/2015EPAS_Web_FINAL.pdf.aspx
Lake, J., & Turner, M. S. (2017). Urgent need for improved mental health care and a more collaborative model of care. The Permanente Journal. https://doi.org/10.7812/tpp/17-024
McLafferty, M., Lapsley, C. R., Ennis, E., Armour, C., Murphy, S., Bunting, B. P., Bjourson, A. J., Murray, E. K., & O’Neill, S. M. (2017). Mental health, behavioural problems and treatment seeking among students commencing university in Northern Ireland. PLOS ONE, 12(12), e0188785. https://doi.org/10.1371/journal.pone.0188785
Mehta, S. S., & Edwards, M. L. (2018). Suffering in silence: Mental health stigma and physicians’ licensing fears. American Journal of Psychiatry Residents’ Journal, 13(11), 2-4. https://doi.org/10.1176/appi.ajp-rj.2018.131101
NIMH » mental illness. (2021, January). NIMH. https://www.nimh.nih.gov/health/statistics/mental-illness
Orjiakor, C. T., Ugwu, D. I., Eze, J. E., Ugwu, L. I., Ibeagha, P. N., & Onu, D. U. (2017). Prolonged incarceration and prisoners’ wellbeing: Livid experiences of awaiting trial/pre-trial/remand prisoners in Nigeria. International Journal of Qualitative Studies on Health and Well-being, 12(1), 1395677. https://doi.org/10.1080/17482631.2017.1395677
What is mental health? (2020, May 28). MentalHealth.gov. https://www.mentalhealth.gov/basics/what-is-mental-health
Appendices
Figure 1
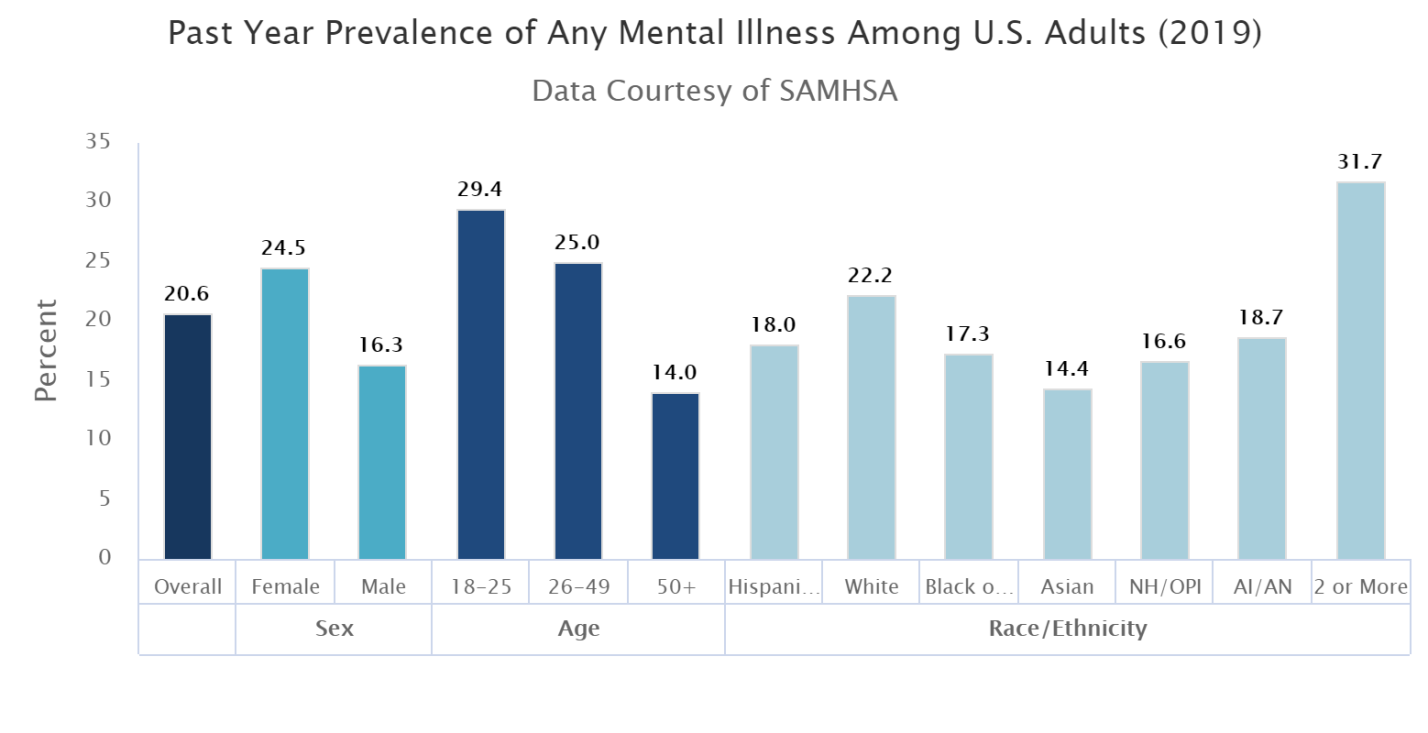
Figure 2
 write
write