Neurology deals with nervous system disorders. It deals with diagnosing and treatment of various types of diseases and conditions that involve the peripheral and central nervous system including their blood vessels, coverings, and all other tissues such as the muscles. Neuro patients suffer from severe injuries in their brains, brain tumours, or strokes, complete or partial paralysis, complete or partial loss of feeling or sensation, seizures, having difficulties in reading and writing, lacking proper cognitive abilities, and muscle weakness. Most people tend to recognize the physical signs of a condition or disorder, it is crucial to understand that neurological problems can also have emotional symptoms. These symptoms can be signs such as individuals experiencing mood swings and these individuals may also suffer from depression and experience delusions. Some assessments can be done to detect neurological problems. Tests such as genetic screening, neurological examination, brain scans, and other tests can be undertaken to detect the presence of neurological conditions. This research will critically look at these conditions and possible treatment options available for patients suffering from neurological problems such as drug options, lifestyle changes to prevent or minimize the conditions, physiotherapy, and pain management. It is important to note that there is no known cure for neurological problems.
Assessment
A neurological assessment is an evaluation of an individual’s nervous system. It can be done with tools such as lights and reflex hammers. Neurologic symptoms may be caused by injuries and trauma such as electrical injury, burns, compression or severing of nerves, detaching of nerves from the spine, dislocation of bones, physical assault, gunshot injuries, and other spine conditions such as slipped vertebral disks. Several areas are tested and assessed during a neurological examination such as the mental status of an individual to determine a person’s awareness and interaction level with their environment. Testing motor function and balance by engaging the patient in small tasks like pulling and pushing and also testing how the patient stands and walks. Conducting a sensory exam by checking the ability of the patient to feel and this can be done by using dull needles, alcohol swabs and other objects. During an assessment, an evaluation of the twelve main nerves of the brain called the Cranial nerves is conducted to determine the functioning of the brain (Celik et al., 2021). During the assessment, a coordination exam is also conducted where the patient may be required to perform functions such as walking normally on a line on the floor or the patient may be instructed to tap their fingers or foot quickly or touch something with their eyes closed. The neurological assessment focuses on the nervous system to examine and recognize abnormalities that affect normal functions in the body in the day-to-day life of an individual.
Assessment of neurological problems in patients looks for signs and symptoms that point to different conditions that are caused by these problems and other common factors such as pathophysiology which is the disordered physiological processes associated with injuries or diseases and also clinical features. Neurological signs are the symptoms that occur in the nervous system of an individual or are caused by the nervous system. Two anatomic parts consist of the nervous system. There is the central nervous system which consists of the spinal cord and the brain that act as the central processing station. The second part is the Peripheral nervous system which transmits sensory information between tissues, muscles, and nerves to the brain and the rest of the body. Neurological signs and symptoms occur when this connectivity in the body is disrupted. The peripheral nervous system is where neurological symptoms often originate from and these are signs and symptoms such as numbness, muscle weakness, paralysis, burning sensation, sensitivity, and prickling sensations. These signs and symptoms may be a result of a local injury when the pain being experienced can be related directly to a systematic illness or trauma that affects the entire body. Referred pain is a condition that is more complex and the pain sensation is felt in a different part of the body from where the illness or injury is in the body (Muhamed, 2019). The most difficult to diagnose and treat is referred pain. It is also important to note that Neurological symptoms can emerge from one nerve in the body or many. When a nerve is compressed leading to a lack of proper blood flow it leads to the occurrence of syndromes such as carpal tunnel syndrome. Neurological symptoms because of the breaking down of the automatic nervous system which is part of the peripheral nervous system may disrupt reflex actions such as swallowing, controlling the bladder, and breathing.
Assessing an individual with neurological conditions requires looking at other signs that may accompany neurological symptoms which may range depending on the pre-existing conditions, diseases, or disorders. Neurological signs and symptoms are vast and this is because the nervous system participates in several functions and also body systems which include controlling the body temperature, regulating the blood pressure, appetite, digestion, sight and movement. There are also neurological symptoms that might accompany other signs and symptoms that affect the nervous system of an individual such as a feeling of burning, altered taste, or smell, cognitive changes, change in the level of consciousness or fainting, involuntary muscle contractions, loss of balance, having muscle weakness, numbness, pain that follows a course of a specific nerve, individuals lacking the ability to move the body which is caused by paralysis, feeling a prickling sensation, tingling, and sensitivity (Celik et al., 2021). Individuals with neurological problems may also experience gastrointestinal signs and symptoms that may accompany nerve symptoms which include individuals experiencing difficulties when chewing, having digestive problems, lacking bowel control, and feeling nausea with or without vomiting.
There are more critical signs and symptoms that may point out conditions that are may be life-threatening. Neurological symptoms that occur as a result of a breakdown in the functioning of the automatic nervous system can be detected by identifying symptoms such as having an abnormally sized pupil or not reacting to direct light, changes in alertness, or individuals not being responsive, experiencing difficulties when swallowing, individuals being disoriented, experiencing vertigo or dizziness, having difficulties when speaking or a slurred speech, the body losing coordination of muscles, experiencing respiratory problems which include shortness of breath, breathing difficulties, choking, wheezing, laboured breathing, or not breathing, experiencing seizures, sudden paralysis, and sudden loss or change of vision (Muhamed, 2019).. Just like the nervous system the causes of neurological symptoms are wide and diverse. The most common part where these symptoms originate from is the nervous system which functions as the transmitter of sensory signals to the central nervous system which is the spinal cord and the brain from the rest of the body.
Treatment
Neurorehabilitation focuses on an individual’s functional independence and well to offer a series of therapies from physiotherapy, psychological therapies, medications, speech and swallow therapies, occupational therapies, re-training patients on mobility skills, communication processes and other dimensions of a patient’s daily life. Neurorehabilitation also provides focus on nutrition, mental health and parts of an individual’s recovery process (Janse et al., 2019). The ultimate goal of assessing and diagnosing neurological disorders in patients is to find a possible method of treatment for an individual to pursue. It is however challenging sometimes to find the most suitable treatment.
Traumatic brain injuries happen when there is a blow to the head and this injury can be penetrating injuries such as machete cut or non-penetrating wounds such as being hit by a blunt object and these injuries vary in severity. Individuals with mild and moderate traumatic brain injury require minimal treatment. The care of such individuals may involve a short period of rest from physical activities and the patient should improve within a few weeks. Severe traumatic brain injury cases often require hospital care and more serious treatment. This treatment includes counselling sessions for emotional support since many patients get stressed and worried about their recovery process. Individuals find it is more difficult to get back to their normal daily routine than they anticipated and this makes counselling very crucial together with other treatments. Surgery may be required for severe cases such as intracerebral haemorrhage which is bleeding in the brain tissue as a result of rapturing of the arteries or veins caused by abnormal pressure, trauma or abnormal enlargement to stop bleeding in the brain reduce brain swelling. Rehabilitation may also be required and this includes physical therapy, occupational therapy and speech therapy. Rest is very important in the treatment process in neurorehabilitation (Sutton, and Visintini, 2018). A doctor gives guidance on how long the patient they are treating traumatic brain injury. The type of traumatic brain injury is put into consideration when a doctor is determining how long a patient should rest before going back to their daily routines. For minor head injuries, rest should not be too long as individuals have more difficulties in returning to work, school and other daily activities and for severe injuries returning to normal activities too soon can make symptoms worse as the aim of treatment is to ease the symptoms and improve the quality of life.
Cognitive behavioural therapy is one way to treat behavioural neurological problems. Cognitive behavioural therapy focuses on the re-orientation of the thoughts of a patient and their behaviour related to their disability. However cognitive behavioural therapy may not be the appropriate treatment for disorders resulting from brain injuries or trauma and the nervous system such as epilepsy. This method of treatment has shown significant effects in the treatment of anxiety and mood disorders and a number of primarily psychogenic impairments (Janse et al., 2019). Cognitive behavioural therapy is advantageous since it does not present the risk of side effects unlike drugs or other interventions. It can also be administered by someone else other than a doctor although it should be administered by a licensed therapist. Because of its noninvasive nature, it is frequently among the first choice for patients.
Physiotherapy intervention is a treatment option that is very effective for patients with neurological conditions such as stroke. High intensity of practice sessions is very important in physiotherapy and the intensity of practice is a crucial factor in meaningful exercising after a stroke and more training leads to faster and better progress. Research has shown that seventeen hours of therapy over a ten-week period is essential for a significant positive impact on motor function and balance (Sutton, and Visintini, 2018). Physiotherapists advocate for at least forty-five minutes of therapy every day in order to achieve the set rehabilitation goals and it is important to ensure a patient can tolerate the intensity of the exercises and is aware that high-intensity practice is better and there is a significant contrast between the recommended and the actual applied therapy time. Treating stroke patients through physiotherapy sessions requires an understanding of the neurophysiological mechanisms, together with neuroplasticity, mechanisms that drive stroke recovery, including the impact of physiotherapy interventions on these mechanisms.
Outcome measures
Outcome measures are the results of the tests used specifically to recognize the primary functioning of a patient at the beginning of treatment. When treatment commences the same instrument can be used to check on the progress and treatment success. Outcome measures are an important part of practice based on evidence. Outcome measures are recognized as important but recent evidence argues that outcome measures are limited in clinical practice (Ronen et al., 2021). Identifying the most suitable outcome measure increases clinical practice by recognizing and evaluating body function and limitations of the structure, preparing the assessment, diagnosis and prognosis, notifying the care plan, and helping to assess the progress and success of the physiotherapy interventions.
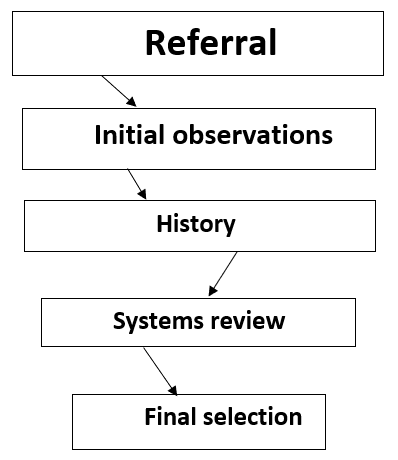
The first step in selecting outcome measures is the clinical decision-making structure. A physical therapist refines and points out the list of possible outcome measures as the therapist continuous through the assessment process directing to the final selection of outcome measures. The guide below is used to give to enhance patient management in the determination and selection of outcome measures. During the history and systems review, potential constructs are identified that may be crucial to measure (Boxer et al., 2019). This enables the recognition of applicable categories for tests and measures which enable the identification of specifics to be measured and pointing out the most suitable outcome measures.
Outcome measures can be grouped into various methods and one is which discusses the purpose of the outcome measures. Outcome measures in clinical practice are designed to achieve one of three particular purposes: to isolate, predict and assess. In most instances, one outcome measure can serve all three purposes which are, discriminate, predict and evaluate. However, in some cases, an outcome measure was developed to serve only a single purpose. An outcome measure designed for one purpose may not effectively serve others and therefore it is important to ensure an outcome measure is used for the intended purpose that it was created and validated. Discriminative outcome measures differentiate between persons or groups on the grounds of a specific characteristic. They also place patients into specific groups of already defined categories. Discriminative outcome measures normally have fewer choices, restricting their capacity to recognize minor changes after intervention (Ronen et al., 2021). A good example is the performance-oriented mobility assessment, which is used to measure balance and gait. It uses a two to three-point ordinal scale. The performance-oriented mobility assessment has outstanding discriminative ability. For example, it can distinguish elders with versus without a history of falls, which is helpful in recognizing individuals who can gain from physiotherapy intervention. This type of scale, however, has a restricted ability to detect change. Imminent measures are intended to predict the future status and may be used to identify risk, decide a prognosis, and arrange discharge.
A performance-based outcome measure provides awareness of a patient’s actual capability at the point in time the test was conducted. A restriction of performance-based outcome measures is that a patient’s capability measured in the clinic may not reflect real performance in their home and community (Boxer et al., 2019). Personal report outcome measures give information on the patient’s point of view and perceptions of the effect of the health condition. They may also provide data on the patient’s awareness of activities performed in their home and community, which cannot be directly observed in the clinic. A restriction of personal report measures is that patients may over-or underestimate their capacity and report what they think the doctor wants to hear.
When deciding whether an outcome measure is suitable to use, various factors such as time, space and equipment requirements, training required to give and interpret the outcome measures, cost to acquire and use the outcome measure, proprietary restrictions, respondent burden, and the patient’s language and culture, should be considered. Some outcome measures may give valuable data, but due to the time required to finish, the suitability for use may be restrictive (Emery et al., 2019). The Balance Evaluation Systems Test for instance which was designed to assist in comparing between possible causes of impaired postural control takes approximately thirty-five minutes to administer. A busy clinician may not have the time to include this outcome measure when first assessing a patient. However, the mini-BESTest was designed from a segment of items from the BESTest. This test can be administered in ten to fifteen minutes, which may be more attainable for many clinicians.
Conclusion
Neurological problems include a wide range of disorders such as epilepsy, neuromuscular disorders, brain tumours, cerebral palsy, gait among others. Examining an individual with neurological conditions requires looking at other signs that may accompany neurological symptoms which may range depending on the pre-existing conditions, diseases, or disorders. Neurological signs and symptoms are vast and this is because the nervous system participates in several functions and also body systems which include controlling the body temperature, regulating the blood pressure, appetite, digestion, sight and movement. Neurorehabilitation focuses on an individual’s functional independence and well to offer a series of therapies from physiotherapy, psychological therapies, medications, speech and swallow therapies, occupational therapies, re-training patients on mobility skills, communication processes and other dimensions of a patient’s daily life. Neurorehabilitation as an intervention to neurological conditions. It provides focus on nutrition, mental health and parts of an individual’s recovery process. The ultimate goal of assessing and diagnosing neurological disorders in patients is to find a possible method of treatment for an individual to pursue. Physiotherapy is also an alternative for treating neurological conditions. It is however challenging sometimes to find the most suitable treatment. Outcome measures are the results of the tests used specifically to recognize the primary functioning of a patient at the beginning of treatment. There are various factors to look at when determining outcome measures such as patient factors, psychometric factors, clinic requirements, and feasibility.
References
Emery, C.A., Whittaker, J.L., Mahmoudian, A., Lohmander, L.S., Roos, E.M., Bennell, K.L., Toomey, C.M., Reimer, R.A., Thompson, D., Ronsky, J.L. and Kuntze, G., 2019. Establishing outcome measures in early knee osteoarthritis. Nature Reviews Rheumatology, 15(7), pp.438-448.
https://www.nature.com/articles/s41584-019-0237-3
Boxer, A.L., Gold, M., Feldman, H., Boeve, B.F., Dickinson, S.L.J., Fillit, H., Ho, C., Paul, R., Pearlman, R., Sutherland, M. and Verma, A., 2019. New directions in clinical trials for frontotemporal lobar degeneration: Methods and outcome measures. Alzheimer’s & Dementia.
https://www.sciencedirect.com/science/article/abs/pii/S1552526019353609
Moccia, M., Lanzillo, R., Brescia Morra, V., Bonavita, S., Tedeschi, G., Leocani, L., Lavorgna, L. and Digital Technologies Web and Social Media Study Group of the Italian Society of Neurology, 2020. Assessing disability and relapses in multiple sclerosis on tele-neurology. Neurological Sciences, 41, pp.1369-1371.
Ronen, G.M., Rosenbaum, P.L. and Streiner, D.L., 2021. Patient perspectives in pediatric neurology: a critical shift in the paradigm of outcome measurement. Developmental Medicine & Child Neurology.
Sutton, D. and Visintini, S., 2018. Off-label use of intravenous immunoglobulin for neurological conditions: a review of clinical effectiveness.
https://europepmc.org/article/nbk/nbk531883?report=printable&client=bot
Janse van Rensburg, H.D., Legoabe, L.J., Terre’Blanche, G. and Van der Walt, M.M., 2019. Methoxy substituted 2-benzylidene-1-indanone derivatives as A1 and/or A2A AR antagonists for the potential treatment of neurological conditions. Medchemcomm, 10(2), pp.300-309.
https://europepmc.org/article/pmc/pmc6390816
Celik, Y., Stuart, S., Woo, W.L. and Godfrey, A., 2021. Gait analysis in neurological populations: Progression in the use of wearables. Medical Engineering & Physics, 87, pp.9-29.
https://www.sciencedirect.com/science/article/abs/pii/S1350453320301697
Muhamed, S.A., 2019. Objective Assessment of Neurological Conditions using Machine Learning (Doctoral dissertation, University of York).
https://etheses.whiterose.ac.uk/25158/
 write
write