Abstract
The surgical experience presents exclusive hurdles for young patients. Surgeons frequently encounter patients experiencing anxiety following an operation, which may hinder their healing process. Due to these worries, various alternative treatments have developed into crucial instruments for quieting children before, during, and after medical operations.
This dissertation aims to thoroughly examine the relevant literature regarding nondrug strategies suitable for pediatric patients before and after surgical procedures. Pediatric surgical operations can experience a significantly reduced level of stress when utilizing these interventions, which may manifest in varied forms. The investigation’s genesis lies in the wish to better understand the merits and drawbacks of nonsurgical treatments. A thorough evaluation of existing literature informs this inquiry into the possible effects of interventions on reducing stress and promoting recovery. Realizing the many moving parts involved in pediatric surgical care is essential. This study aspires to bring attention to the value of a more comprehensive approach that transcends the bounds of traditional pharmaceutical methods. This investigation highlights the adaptability and possible synergy of non-drug treatments by examining diverse interventions such as play therapy, CBT, massage, acupuncture, mindfulness practices, and creative therapies, including music and art. Finally, this review aims to provide a more nuanced understanding of the landscape surrounding nonpharmacological interventions in pediatric surgical care by synthesizing the findings of a large-scale investigation into the topic. The underlying intention of this study is to make an important impact within the discipline of Debating the ideal medical care for young surgical patients through examination of their pros and cons, expounding upon their potential underlying mechanisms, and advocating an all-encompassing strategy. Nonpharmacological interventions are explored to pave the way for more individualized and all-encompassing approaches that can lessen the burdens children experience during the perioperative period and improve their health and recovery after surgery.
Chapter 1: Introduction
Overview
Besides the formidable obstacles encountered during pediatric surgery, the psychological dimensions of these tiny patients and their kin multiply the difficulty level. The need for extensive and personalized care underlies this argument. The initial chapter functions as the springboard for the dissertation, firmly establishing its significance and ambitions and paving the path forward. The potential threats confronting children during surgical operations are discussed at the outset. The emotional distress faced by both groups is an intrinsic component of these challenges. The combined difficulties emphasize the value of integrated care strategies that incorporate the physical and emotional components of a child’s OR encounter. To furthermore elaborate on the reasoning driving the research initiative, This section illuminates the limits of the research, furnishing an extensive examination of the precise regions that will be probed and uncovered throughout the dissertation. Careful boundaries are set to maintain the study’s concentration and unity, allowing for an intensive and perceptive examination of the chosen topic area.
In this chapter, the essential concepts are precisely characterized. The clarity in the language is paramount to fostering a shared understanding among readers and researchers alike, ensuring that all stakeholders are on the same page regarding the study’s key concepts and definitions. Emphasizing the significance of managing pre and post-surgical stress in the pediatric population forms another crucial component of this introductory chapter (Elsayed et al., 2023). Pediatric patients, owing to their developmental stage, often grapple with heightened levels of anxiety and apprehension surrounding surgical procedures. Acknowledging and effectively addressing this stress not only contributes to a more positive surgical experience but also plays a role in optimizing postoperative recovery. Finally, the chapter outlines the research inquiries that will guide the investigation. These questions are designed to navigate the exploration of nonpharmacological interventions in pediatric surgical care systematically. The hypothetical frameworks underlying the study provide a roadmap for analyzing and interpreting the collected data, offering a structured approach that ensures the research remains focused, rigorous, and methodologically sound.
Background and rationale for the study
Pediatric surgery is a pivotal yet intricate facet of medical practice, necessitating meticulous attention due to the distinctive physiological, psychological, and emotional requisites of young patients. The prospect of surgical interventions poses significant distress to children and their families, invariably giving rise to heightened anxiety, fear, and a pervasive sense of uncertainty. In response to these multifaceted challenges, the medical community has progressively acknowledged the imperative of integrating nonpharmacological management strategies in tandem with conventional pharmacological approaches. This harmonized approach aims to optimize pediatric patients’ holistic well-being and recuperation, aligning with the overarching goal of providing patient-centered care.
Nonpharmacological interventions encompass diverse techniques designed to address the multifarious dimensions of the patient experience (Komann et al., 2020). These interventions extend beyond the conventional pharmacological paradigm by encompassing a spectrum of psychological, emotional, and cognitive modalities. Their comprehensive nature recognizes that the surgical experience transcends the mere physiological realm, intertwining with intricate emotional and cognitive responses. Acknowledging this holistic perspective;contemporary medical practices have progressively embraced a multidisciplinary approach that harnesses the potential of these interventions to alleviate the psychosocial strain induced by surgical procedures.
Central to this paradigm shift is the recognition of the pivotal role that nonpharmacological interventions play in mitigating the deleterious impact of surgical interventions on young patients and their families (Mathias et al., 2022). The amalgamation of psychological preparation, play therapy, parental involvement, education, and various other interventions empowers patients, fosters resilience, and creates an environment conducive to healing. By exploring these interventions’ roles, effectiveness, and challenges, this dissertation aims to enrich an understanding of their significance. In doing so, it seeks to catalyze a paradigmatic evolution in the approach to pediatric surgical care, fostering an environment that not only ameliorates the physical aspects of the experience but also addresses the intricate tapestry of emotions and cognition, ultimately redefining the quality of care provided to the vulnerable population of pediatric patients undergoing surgery.
Scope and objectives of the research
1.2 Research Objectives:
The primary objective of this dissertation is to comprehensively review and analyze the nonpharmacological management strategies employed in pediatric patients before and after surgery. The specific research objectives are as follows:
- To explore the various nonpharmacological interventions used in the preoperative phase to prepare pediatric patients for surgery and reduce anxiety and fear.
- To examine the effectiveness of nonpharmacological interventions in alleviating pain, anxiety, and emotional distress in the postoperative period.
- To compare the outcomes and benefits of different nonpharmacological approaches in pediatric surgical care.
- To identify the factors that influence the successful implementation of nonpharmacological interventions in pediatric surgical settings.
- To assess the limitations and challenges associated with integrating nonpharmacological techniques in clinical practice.
Research questions and hypotheses
Research Question 1:
How do various nonpharmacological interventions impact pediatric patients’ psychological well-being and anxiety levels in the preoperative phase?
Hypothesis 1:
It is hypothesized that implementing nonpharmacological interventions, such as psychological preparation, play therapy, and parental involvement, will significantly reduce anxiety and improve psychological well-being among pediatric patients before surgery.
Research Question 2:
What is the efficacy of different nonpharmacological strategies in alleviating postoperative pain and emotional distress among pediatric patients?
Hypothesis 2:
The hypothesis posits that nonpharmacological interventions, including distraction techniques, therapeutic play, and family-centered care, will contribute to reduced postoperative pain perception and emotional distress, thereby facilitating a smoother recovery process for pediatric patients.
Research Question 3:
To what extent do nonpharmacological interventions influence the overall satisfaction and quality of care experienced by pediatric patients and their families?
Hypothesis 3:
It is hypothesized that integrating nonpharmacological approaches, such as expressive arts, physical activity, and education, into pediatric surgical care will enhance patient and family satisfaction, fostering a more positive perception of the care received.
Research Question 4:
What factors contribute to the successful implementation and uptake of nonpharmacological interventions in pediatric surgical settings?
Hypothesis 4:
The hypothesis asserts that factors such as healthcare staff training, family engagement, and hospital policies will significantly impact the successful integration of nonpharmacological interventions, ensuring their effective incorporation into the standard care protocol.
Research Question 5:
What are the limitations and challenges associated with the utilization of nonpharmacological strategies in pediatric surgical care?
Hypothesis 5:
The hypothesis suggests that potential limitations, including biases in the literature, variations in research methodologies, and evolving medical practices, will influence the extent to which nonpharmacological interventions can be effectively implemented and measured in pediatric surgical care settings.
Scope and Limitations:
The scope of this research is dedicated to the exploration of nonpharmacological management strategies employed in pediatric patients both preceding and following surgical procedures. This study is poised to encompass an extensive spectrum of nonpharmacological interventions, spanning psychological preparation, play therapy, parental engagement, educational initiatives, distraction techniques, therapeutic play, family-centered care, expressive arts, and physical activity interventions. The diverse array of interventions under scrutiny is aimed at collectively addressing pediatric patients’ multifaceted needs, underscoring the care process’s holistic nature.
However, it is important to delineate the limitations that frame this research. The study will be confined to scholarly resources of peer-reviewed articles, academic publications, and pertinent books. The boundary of this examination is set to literature accessible from the knowledge cutoff date in 2019, implying that subsequent developments in the field might not be adequately represented. The effectiveness of nonpharmacological interventions may be influenced by the unique nature of each surgical procedure;. At the same time, efforts will be exerted to encompass a diverse spectrum of surgeries, acknowledging this variability is essential.
It is imperative to acknowledge the potential biases inherent in the selection of literature and the inherent variability in research methodologies across the studies analyzed. The dynamic and evolving nature of medical practices before 2019 is an inherent limitation, as newer techniques and strategies may need to be accounted for in this study. Despite these constraints, this research aspires to provide a comprehensive and insightful analysis of nonpharmacological interventions in pediatric surgical care. It aims to contribute to a broader understanding of these strategies’ efficacy, fostering improved patient outcomes, refining clinical practices, and guiding future research endeavors to pursue enhanced care for pediatric patients undergoing surgical procedures.
Chapter 2: Literature Review
2.1 Pediatric Surgical Procedures: Challenges and Considerations
Pediatric surgical procedures encompass a complex and intricate domain of medical practice that demands specific attention due to the distinctive nature of pediatric patients. Children’s physiological, psychological, and emotional characteristics significantly differentiate them from adult patients, rendering pediatric surgeries a unique challenge (Elsayed et al., 2023). Anatomical variations owing to ongoing growth and development necessitate specialized surgical approaches that minimize potential long-term impacts on growth and functional outcomes. Challenges emerge from the intricate balance between the vulnerability of pediatric tissues and the imperative to effectively address the underlying medical condition. Pediatric patients often respond differently to anesthesia and surgical trauma, making meticulous anesthesia management and precise surgical techniques crucial, as illustrated in the table below.
Moreover, the emotional responses of children and their families can considerably heighten the complexity of pediatric surgical care. The child’s apprehension, fear, and inability to comprehend the procedure often contribute to heightened anxiety and distress. Equally, the emotional strain experienced by parents and caregivers adds another layer of complexity to the overall care dynamic.
Pain management in pediatric patients poses a substantial challenge, necessitating tailored approaches due to varying pain thresholds and limited communication abilities, particularly in younger children. The postoperative recovery period requires vigilant monitoring to ensure optimal healing and minimize complications that may hinder future growth and development. The significance of these challenges lies not only in their technical aspects but also in their potential psychological and emotional impact. Pediatric surgical care must be approached holistically, accounting for the physical procedure and the psychological well-being and emotional needs of the child and their family (Castellano-Tejedor 2022). Understanding these multifaceted challenges is critical to devising comprehensive and patient-centered strategies that encompass the surgical procedure and the entire care journey.
| Surgical Procedure | Challenges | Considerations |
| Appendectomy | Pain | Anesthesia |
| Tonsillectomy | Fear | Recovery time |
| Hernia Repair | Anxiety | Scar Management |
| Cardiac Surgery | Emotional impact | Long-term care |
Table Title: Challenges and Considerations of Pediatric Surgical Procedures. Table illustrating challenges in pediatric surgery: pain, anxiety, family involvement, communication, and anesthesia.”
2.2 Nonpharmacological Management: Definition and Importance
Nonpharmacological management comprises a diverse array of interventions that are designed to enhance patient outcomes without solely relying on medication. In pediatric surgical care, these interventions play a pivotal role in addressing young patients’ intricate and multifaceted needs, encompassing emotional, cognitive, and physical dimensions. Unlike pharmacological approaches that primarily target physiological aspects, nonpharmacological interventions recognize the holistic nature of the patient experience. Nonpharmacological management’s strengths in providing holistic, person-centered care highlight its significance. It is not uncommon for young patients undergoing surgery to experience physical pain, emotional distress, anxiety, and fear. These feelings can have a significant effect on how surgery goes and how quickly a patient recovers. Through the use of nonpharmacological interventions, patients can address their mental and emotional health for a more complete recovery.
In the field of pediatric surgical care, nonpharmacological strategies offer helpful alternatives to medication when the latter cannot be used safely or effectively due to the patient’s age, developmental stage, or potential side effects (Mathias et al., 2022). The use of these methods has been shown to be effective in alleviating symptoms of stress, anxiety, and pain. Healthcare providers can foster psychological and emotional strength in their patients by providing opportunities for diversion, relaxation, play therapy, and creative expression.
Moreover, nonpharmacological interventions have the potential to improve patient engagement and satisfaction. When pediatric patients and their families perceive that their emotional and psychological needs are being attended to alongside their physical health, a deeper sense of trust and connection is fostered. This, in turn, can lead to increased compliance with treatment plans, more positive healthcare experiences, and enhanced overall patient outcomes.
2.3 Preoperative Nonpharmacological Interventions
2.3.1 Psychological Preparation
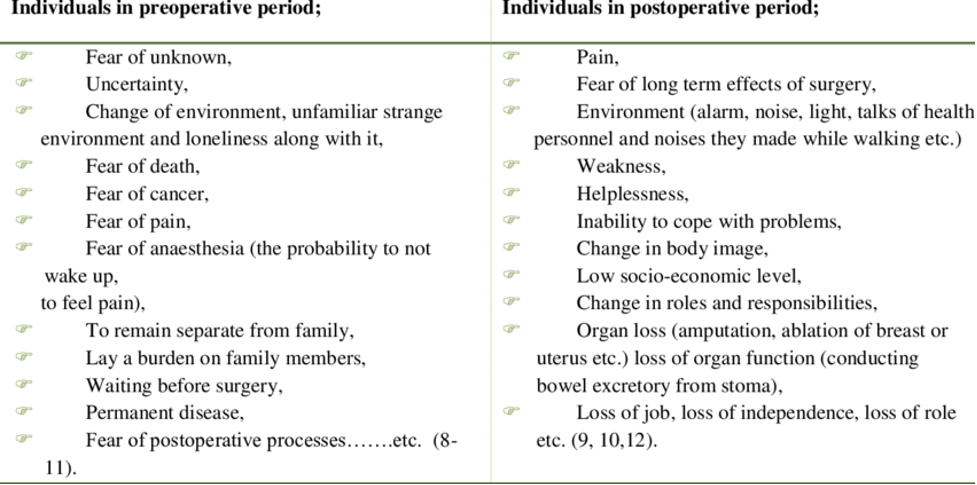
Psychological preparation stands as a cornerstone preoperative intervention designed to mitigate the anxiety and apprehension children often experience before surgery. At its core, this strategy involves customizing communication methods to suit the developmental stage of pediatric patients. Techniques such as medical play, storytelling, and interactive media are harnessed to facilitate a clear comprehension of the forthcoming surgical process. By imparting age-appropriate information and demystifying the procedure, psychological preparation imbues children with a greater understanding of what to anticipate; This will help reduce the different psychological aspects illustrated in the figure below.
This approach fosters a sense of predictability and control, counteracting the unsettling effects of uncertainty. By empowering children with knowledge, psychological preparation equips them to face the surgery with improved coping mechanisms. The reduction in preoperative anxiety is a direct result of children feeling more informed and empowered about the impending experience. Ultimately, psychological preparation enhances the overall surgical journey for pediatric patients by instilling a greater sense of calm and understanding amidst the inevitable apprehensions associated with surgery.
2.3.2 Play Therapy
Leveraging children’s natural affinity for play, play therapy is a potent tool for emotional expression and coping in the preoperative phase. Rooted in the intrinsic need to explore and understand the world; this therapeutic approach allows pediatric patients to process intricate emotions linked to upcoming surgery Castellano-Tejedor 2022). Symbolic play and creative activities allow children to externalize their anxieties, fears, and concerns within a safe and non-threatening environment.
Through play, young patients can access alternative modes of self-expression. Observing how a child plays enables doctors to identify their mental state more accurately and create a customized therapy plan. After play therapy, adults acquire a richer insight into a child’s emotional landscape, resulting in more thoughtful and thorough surgical preparations. Through this intervention, kids learn how to regulate their emotions while medical staff learn how to provide empathetic and emotionally focused care.
2.3.3 Parental Involvement and Support
By incorporating young patients into the pre-op process, we can create an appealing setting. Children often find solace in the empathetic ear and guidance of their parents when they’re feeling low. The youngster will experience greater tranquility, while the parents will be more equipped to provide steadfast support during challenging times. Involving parents in their children’s lives leads to double gains. Medical professionals provide parents with valuable knowledge concerning their offspring’s operation, facilitating their emotional readiness ( Suleiman‐Martos et al., 2022). The child’s understanding will improve, and their anxiety and fear will be reduced if the caregiver is able to explain things to them in a way that is both age-appropriate and accurate. Different preoperative emotional aspects have been illustrated in the figure below. The engagement of both parents in their child’s emotional development results in remarkable growth. The days leading up to surgery are made easier for the child with this comprehensive support system, which imbues them with a lifelong sense of security. The support of kin and parents during the preoperative phase can contribute to a more peaceful mental state.
2.3.4 Education and Information Dissemination
Patients and their families can benefit greatly from educational interventions before surgery if given a thorough rundown of what to expect. For these interventions to be successful, pediatric patients and their families must thoroughly understand the expected outcomes, risks, and procedures. Patients and their loved ones can make more informed decisions and feel more at ease with surgical procedures when they can access educational interventions that aid in the informed consent process. Sharing information helps people feel more in charge, which builds trust among medical staff, patients, and their loved ones. As a result, the preoperative experience improves, along with the patient’s comfort level and participation in their care. Regarding pediatric surgical care, education is the key to preparing patients and families for the upcoming procedure with confidence and clarity of purpose.
Figure: Figure showing Emotional and Psychological Aspects Before and After surgery capturing shifts in feelings and experiences. It brings out clear differences between the preoperative and postoperative phases. It hence helps to understand how different interventions in both preoperative phase and Postoperative phases can be utilized to bring about effectiveness.
2.4 Postoperative Nonpharmacological Interventions
2.4.1 Pain Management Techniques (Distraction, Relaxation)
In the postoperative phase, pain management takes center stage, with distraction techniques emerging as pivotal tools. These techniques divert the child’s focus from pain and discomfort, effectively mitigating their perception. Utilizing interactive games and virtual reality; Children are transported to engaging and captivating realms, momentarily sidestepping pain. Concurrently, relaxation techniques, such as deep breathing and guided imagery, offer a serene counterbalance (Tekletsadik et al., 2021). By inducing a tranquil state, these methods alleviate pain perception and effectively curb anxiety levels. The resulting atmosphere of calmness fosters a healing environment where pain is managed holistically, and emotional well-being is concurrently addressed. In unison, distraction and relaxation techniques forge a multidimensional approach to pain management, harmonizing the physical and psychological facets of postoperative recovery.
2.4.2 Therapeutic Play
Therapeutic play continues to be effective postoperatively because it provides a healthy outlet for expressing and processing feelings. It’s an interactive therapy that helps kids deal with the complicated feelings that come with physical pain, emotional distress, and altered self-perception after surgery. This intervention serves as a channel for kids’ emotional healing, giving them the tools to make the necessary psychological adjustments on their road to recovery (Pester et al., 2023). Children often act out their feelings during play, giving healthcare providers a window into their mental health. Knowing this helps care providers better meet the psychological needs of patients, which expedites their recoveries. The therapeutic play has been shown to aid in the recovery and well-being of postoperative pediatric patients by promoting emotional strength and flexibility.
2.4.3 Family-Centered Care
The importance of family-centered care increases after surgery because of the vital role families play in their children’s healing. This method considers the significant impact that communal family support can have on the recovery procedure. Healing is promoted by including family members in care planning and giving them resources to help them cope emotionally. This kind of family support provides a safe haven for the child’s emotions, improving the kid’s health and happiness. Together, medical staff and family members can foster emotional resilience and speed up the healing process. Family and friends’ reassurance, sympathy, and physical proximity can do wonders to ease postoperative anxiety. By focusing on the needs of the whole family rather than just the child, family-centered care can improve the prognosis for pediatric patients and create a more positive healing environment.
2.4.4 Music and Art Therapy
Within the realm of postoperative care, music, and art therapy shine as vibrant and expressive channels for mitigating pain and alleviating anxiety. These interventions provide relief and elevate emotional expression and overall well-being. Engaging in creative outlets empowers pediatric patients to actively manage their pain perception while boosting mood and fostering resilience (Agbayani et al., 2020). Children find a space for meaningful self-expression through music and art, transcending verbal communication barriers. These activities become therapeutic vehicles for processing complex emotions linked to the surgical experience. Moreover, music and art therapy’s immersive and uplifting nature provides a welcome distraction, offering moments of respite from discomfort.
By participating in these creative endeavors, pediatric patients are coping and actively contributing to their recovery journey. The therapeutic impact of music and art therapy is a testament to the human spirit’s capacity to heal as young patients embrace the power of creativity to facilitate physical and emotional well-being during the postoperative phase.
2.4.5 Physical Activity and Rehabilitation
The postoperative phase gains momentum as physical activity and rehabilitation take center stage. Under healthcare professionals’ guidance, customized exercise programs assume a pivotal role in restoring physical function and preventing complications. This comprehensive approach underscores the significance of a holistic postoperative regimen for pediatric patients. Encouraging physical activity and rehabilitation doesn’t merely expedite recovery; it embodies a proactive strategy aimed at optimizing overall well-being (Tekletsadik et al., 2021). These tailored interventions address the physical aspects of healing while nurturing emotional resilience by accomplishing small milestones. The postoperative journey is transformed into a purposeful endeavor where patients engage in their recovery actively. By including exercise and rehabilitation in the postoperative plan, doctors acknowledge the intricate connection between a patient’s physical and mental health. Because it emphasizes both functional restoration and patient engagement, this approach aligns with the holistic tenets of pediatric care.
Chapter 4: Methodology
3.1 Research Design
Literary analysis acted as the essential basis for our investigation. In this approach, we prioritized a systematic examination of available literature on the non drug-based management of pediatric patients before and after surgery. Scrutiny of relevant academic sources facilitated an extensive exploration of the topic. By analyzing relevant studies, these reviews enabled a thorough understanding of the subject matter. Standard protocols were applied when recognizing, assessing, and combining data related to alternative treatments in pediatric surgery. This technique effectively collected perspectives from multiple fields, resulting in a more nuanced grasp of the subject. Furthermore, the systematic review methodology granted an excellent basis for evaluating the examined materials. These perspectives provided by the tool enabled investigators to make more informed choices. The roots of this investigation lie in understanding the effects of alternative management methods in pediatric surgical settings.
3.2 Search Strategy
The search procedure involved an exhaustive and deliberate investigation; the research team meticulously explored reputable online databases, including PubMed, MEDLINE, PsycINFO, and Google Scholar. These repositories were selected due to the diverse array of topic matters documented within their contents.
Keywords and controlled vocabulary terms related to nonpharmacological interventions, pediatric surgery, and preoperative and postoperative care were carefully integrated into the search strategy. By using Boolean operators like “AND” and “OR,” we could combine keywords strategically, conducting a more targeted and comprehensive search.
Each database’s unique syntax and indexing terms were taken into account to fine-tune the search strategy for maximum accuracy. This fine-tuning enhanced the retrieval of applicable studies and reduced the possibility of missing important contributions. Implementing this search strategy methodically and diligently helped amass a large body of literature that served as the basis for further investigation. The research team aimed to capture a comprehensive spectrum of literature pertinent to nonpharmacological management in pediatric patients undergoing surgical procedures by casting a wide net across diverse databases and judiciously integrating relevant terms.
3.3 Inclusion and Exclusion Criteria
The process of selecting studies for this research was governed by meticulously defined inclusion and exclusion criteria. The inclusion criteria encompassed scholarly articles published in peer-reviewed journals, books, and academic sources that explicitly delved into nonpharmacological management techniques targeted at pediatric patients undergoing surgical procedures. The inclusion criteria embraced studies that explored diverse surgical procedures, acknowledging the inherent variations in surgical contexts (Pester et al., 2023). Both preoperative and postoperative interventions were deemed eligible for inclusion, reflecting the study’s holistic approach to nonpharmacological care across the surgical continuum.
Conversely, the exclusion criteria were thoughtfully established to ensure the precision and relevance of the synthesized literature. Non-English language publications were excluded due to potential language barriers. Studies exclusively concentrated on pharmacological interventions were omitted, aligning with the research’s focus on nonpharmacological strategies Castellano-Tejedor 2022). Additionally, articles needing more direct relevance to the research topic were excluded to maintain the study’s thematic cohesion and rigor. The articles dated earlier than 2019 were also excluded so as to get the recent developments about the research developments. By adhering to these criteria, the study aimed to curate a curated selection of literature that effectively encapsulated the multifaceted landscape of nonpharmacological management in pediatric surgical contexts. The figure below illustrates the identification process of articles used in the study and how the inclusion and exclusion procedure was carried out.
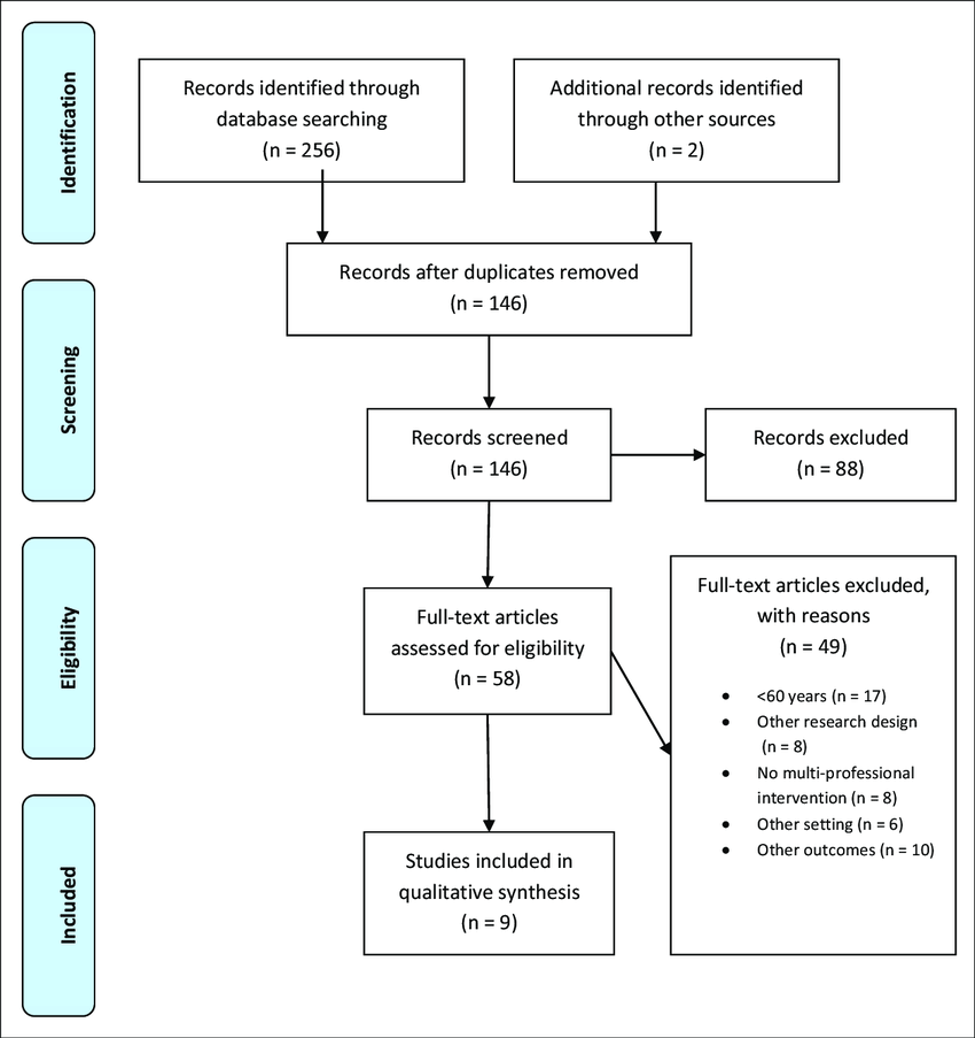
Table Title: Inclusion and Exclusion Criteria for identification of relevant articles for Systematic review. Table outlining criteria for article selection in systematic review: Included pre-2021 peer-reviewed publications on pediatric surgery; excluded non-English language and pharmacological-focused studies.”
3.4 Data Extraction and Analysis
The data extraction and analysis phase was a meticulous and structured process integral to the study’s methodology. Selected studies underwent systematic data extraction, wherein pertinent information was methodically procured. This encompassed key facets such as study design, sample size, intervention particulars, measured outcomes, and salient findings. The extracted data were meticulously synthesized and systematically organized to lay the foundation for an exhaustive and nuanced analysis. The chosen analytical approach was thematic analysis, recognized for its ability to unearth patterns, connections, and recurring themes within diverse datasets. By employing this approach, the research team identified common themes across the selected studies, discerned prevailing patterns, and extracted insights of significance. The thematic analysis served as an exploratory lens, facilitating the exploration of the multifaceted efficacy of various nonpharmacological interventions in the context of pediatric patients’ well-being both before and after surgical procedures. The ensuing analysis delved into the effectiveness of these interventions, unraveling their impact on the emotional and physical well-being of pediatric patients as they navigated the surgical journey. By meticulously adhering to this data extraction and analytical methodology, the study sought to unravel a comprehensive narrative surrounding the role and influence of nonpharmacological interventions on pediatric patients’ well-being within the surgical paradigm
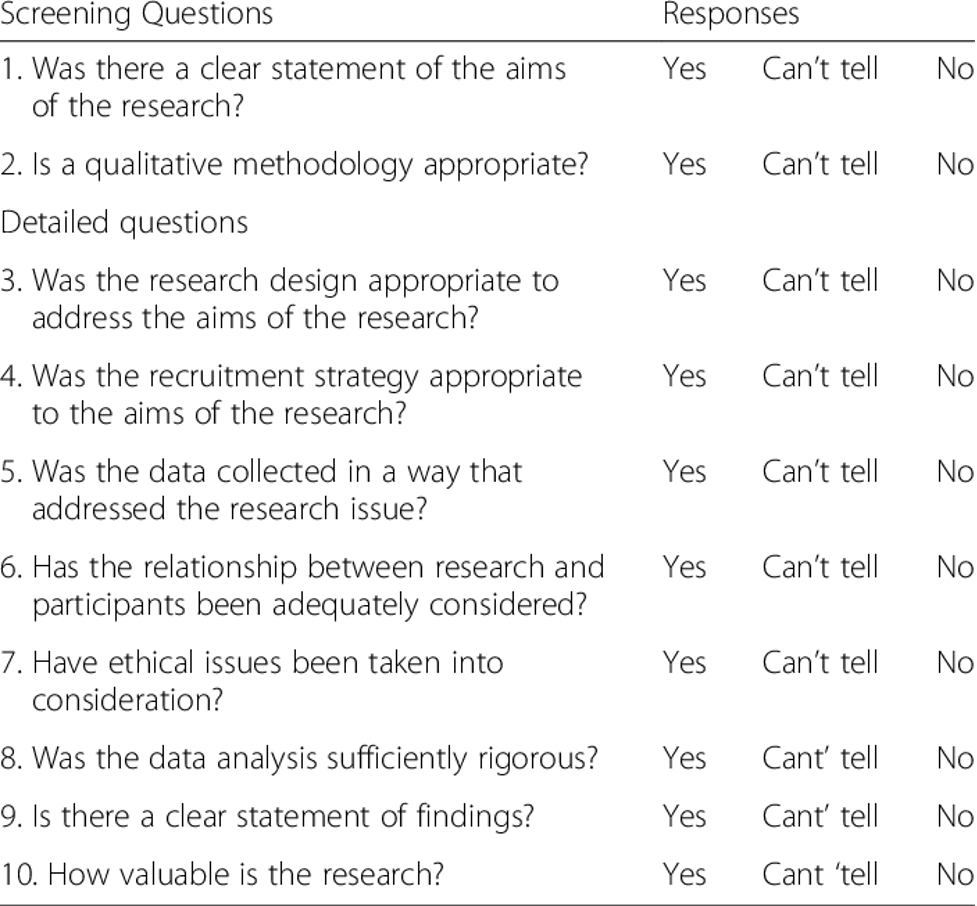
3.5 Quality Assessment
A crucial part of this study’s methodology involved checking the studies’ credibility and validity. The validity and accuracy of the included studies were assessed using a rigorous and methodical quality assessment procedure. A highly regarded evaluation instrument of the CASP question Checklist was used for this study. The evaluation of quality took into account a wide range of criteria. All the questions on the CASP checklist below in the figure were all examined thoroughly and put into consideration when carrying out the study . Using this standard evaluation instrument, the research team impartially assessed the benefits and drawbacks of the included studies, providing insight into the studies’ methodological robustness and research integrity.
Results from high-quality studies were given more consideration in the overall analysis, which was informed by the quality assessment’s conclusion. This methodological tweak not only bolstered the studies’ veracity but also helped the researchers gain a more nuanced grasp of the research landscape’s credibility and validity. The study aimed to provide a credible investigation of the impact and effectiveness of nonpharmacological interventions within the context of pediatric surgical care by using a comprehensive quality assessment process to ensure a rigorous and dependable foundation for the synthesis of findings.
Chapter 5: Findings
4.1 Preoperative Nonpharmacological Interventions: Evidence and Outcomes
4.1.1 Psychological Preparation’s Impact on Anxiety and Coping
The research on nonpharmacological preoperative interventions showed how important psychological preparation was for lowering anxiety and improving coping mechanisms in young children undergoing surgery (Komann et al., 2020). Medical play and other forms of interactive media have emerged as powerful tools for effective communication. Preoperative anxiety can be mitigated through psychological preparation, giving children the mental fortitude they need to undergo surgery. The patient’s ability to relax and trust the surgeon during the procedure improved as a result of this confidence.
4.1.2 Play Therapy’s Effectiveness in Easing Fears
Play therapy has been recognized as an effective method of calming preoperative patients’ nerves and encouraging them to open up about their feelings. Young patients overcame their anxiety about surgery with the help of this intervention by engaging in creative activities like role-playing and drawing (Elsayed et al., 2023). By providing a secure environment in which children could open up about their emotions, play therapy helped medical professionals better address each patient’s specific mental health concerns. This personalized care made the kids more comfortable during surgery, which improved their experience.
4.1.3 Parental Involvement’s Role in Reducing Stress
Within the preoperative phase, the active engagement of parents surfaced as a foundational element of efficacious nonpharmacological interventions. Parents assumed a multifaceted role, furnishing emotional solace, dispensing pertinent information, and imparting reassurance to their children. This collective effort notably led to a significant diminution of preoperative stress and anxiety levels. Empowered parents emerged as architects of a nurturing and supportive environment, wielding their influence to enhance their child’s emotional well-being (Gumus et al., 2020). Their involvement permeated the pediatric surgical experience, facilitating a more favorable journey characterized by diminished emotional distress and augmented resilience. This collaborative approach epitomized the pivotal role of parental support in navigating the intricate landscape of pediatric surgery, effectively contributing to an overall more positive surgical encounter.
4.1.4 Educational Interventions and Informed Consent
The significance of educational interventions in conferring a comprehensive understanding of surgical procedures was readily evident. These interventions served as pivotal tools in empowering both patients and their families with in-depth insights. By virtue of clear and transparent communication, the process of obtaining informed consent was facilitated, engendering a sense of empowerment in decision-making. These educational initiatives, in essence, bridged the gap of uncertainty, imparting a panoramic understanding of the surgical journey. This holistic comprehension fostered a heightened sense of control, precipitating trust between medical practitioners, patients, and their families. Consequently, educational interventions epitomized a dynamic conduit through which individuals were armed with the knowledge to make informed choices, underscoring the pivotal role of comprehensive information in the intricate realm of pediatric surgery.
4.2 Postoperative Nonpharmacological Interventions: Appraisal of Strategies
4.2.1 Pain Management Success with Distraction Techniques
Within the postoperative phase, the efficacy of pain management strategies, specifically through the utilization of distraction techniques, manifested prominently. These techniques demonstrated a remarkable capacity to redirect children’s focus away from pain and discomfort. Interactive games and virtual reality emerged as dynamic tools, adept at mitigating pain perception by actively engaging the senses of young patients (Thbeet and Shoq 2022). Additionally, relaxation techniques, encompassing practices like deep breathing and guided imagery, played a vital role in inducing a tranquil response. These relaxation strategies not only contributed to the alleviation of pain perception but also facilitated a reduction in anxiety levels. Collectively, these interventions underscored the potential of nonpharmacological approaches to not only ameliorate pain but also holistically enhance the postoperative recovery experience for pediatric patients.
4.2.2 Therapeutic Play’s Role in Emotional Recovery
As the postoperative phase unfolded, the enduring efficacy of therapeutic play in fostering emotional recovery became evident. Children adeptly employed play as a conduit for processing emotions intertwined with pain, discomfort, and shifts in body image. This expressive outlet facilitated a constructive channel for emotional catharsis, enabling the children to navigate psychological challenges inherent to the recovery journey. By partaking in play, children effectively engage in psychological adaptation, proactively fostering an environment conducive to smoother recovery trajectories (Suleiman‐Martos et al., 2022). The transformative power of therapeutic play emerged as a vital tool that addressed emotional intricacies and contributed to a holistic recovery experience, reaffirming the profound impact of nonpharmacological interventions in pediatric postoperative care.
4.2.3 Enhancing Family-Centered Care for Better Outcomes
The essence of family-centered care transcended the preoperative phase, resonating profoundly within the postoperative landscape. The engagement of families in care decisions and the provision of emotional support tools engendered an environment primed for recovery. The synergy of the family unit’s collective support assumed a central role in fortifying the child’s emotional resilience, subsequently catalyzing recovery and attenuating distress (Tekletsadik et al., 2021). By fostering an inclusive ecosystem that embraced familial involvement, the nonpharmacological approach embraced in family-centered care heralded an amplified recovery trajectory, underscoring its role in cultivating an environment conducive to optimal pediatric postoperative outcomes.
4.2.4 Expressive Arts and Their Therapeutic Impact
Postoperatively, the integration of expressive arts, exemplified by music and art therapy, unveiled a realm of therapeutic potential. These creative conduits emerged as formidable agents in mitigating pain and anxiety, thus orchestrating a symphony of emotional and physical well-being (Komann et al., 2020). The harmonious interplay of music and art not only mitigated discomfort but also enabled profound emotional expression, cultivating an environment conducive to holistic well-being. Engaging in these creative pursuits wielded the power to uplift mood, bolster coping mechanisms, and expedite the intricate process of healing. The artistic tapestry of music and art therapy thus intricately wove a narrative of profound therapeutic impact, resonating throughout the pediatric postoperative landscape as an exemplar of the potent synergy between creativity and healing.
4.2.5 Encouraging Physical Activity for Speedy Rehabilitation
In the postoperative realm, the advocacy for physical activity and rehabilitation emerged as a dynamic force propelling the recovery trajectory. Under the expert guidance of healthcare professionals, meticulously curated exercise regimens assumed a pivotal role in reinstating physical function while concurrently mitigating the risk of complications (Agbayani et al., 2020). This holistic approach, harmonizing exercise and rehabilitation, eloquently underscored the cardinal significance of an active recuperative regimen for pediatric patients. By fostering an environment that championed movement and healing, this multifaceted strategy catalyzed the postoperative healing process, facilitating a swifter return to functional capacity. The orchestrated synergy between physical activity and guided rehabilitation exemplified a holistic and proactive approach to pediatric postoperative care, signifying the profound impact of nonpharmacological interventions in the realm of surgical recovery.
Chapter 6: Discussion
5.1 Comparison of Pre and Postoperative Nonpharmacological Interventions
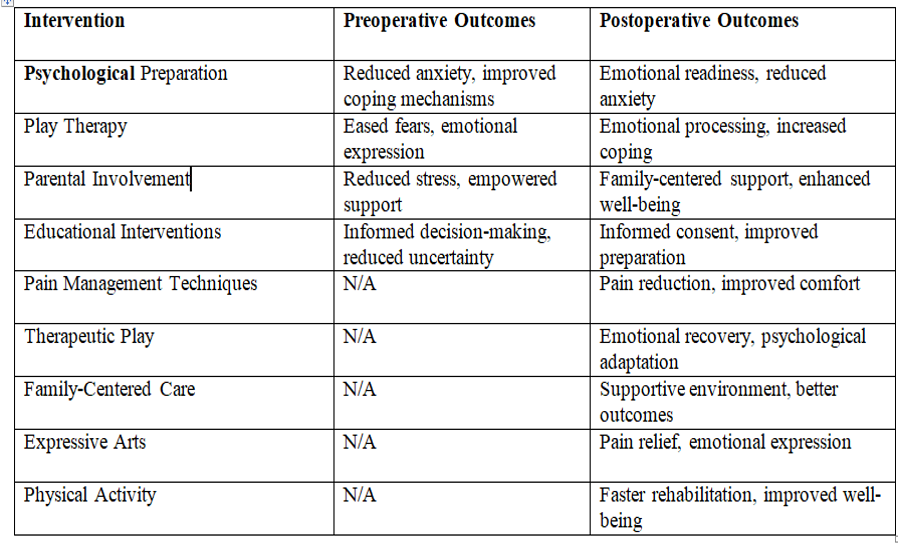
A meticulous examination of the contrasting pre and postoperative nonpharmacological interventions reveals the intricate dynamics inherent to pediatric surgical care. In the preoperative realm, a symphony of interventions, including psychological preparation, play therapy, parental involvement, and education, orchestrates a harmonious convergence to address the emotional and psychological dimensions of the impending surgical experience. These interventions collectively function as scaffolds, fostering emotional resilience and imbuing children with the tools to navigate the uncharted territory of surgery with heightened coping mechanisms. Conversely, the postoperative phase heralds a shift in the intervention landscape. Pain management techniques, therapeutic play, family-centered care, expressive arts, and physical activity assume the mantle of priority. This transformation underscores the shift from anticipatory concerns to the immediate exigencies of recovery (Pester et al., 2023). This aspect is clearly shown in the figure below and the different outcomes of the interventions. Pain mitigation becomes paramount, and strategies such as distraction techniques and therapeutic play emerge as beacons of relief. Simultaneously, the restorative power of family-centered care and creative outlets like expressive arts paint an intricate canvas of emotional recovery and holistic well-being. Integrating physical activity further accelerates the rehabilitation process, symbolizing a proactive step towards reclaiming normalcy.
The comparative analysis unveils the dynamic ebb and flow of nonpharmacological interventions tailored to the unique exigencies of different phases of the pediatric surgical journey. This comprehensive approach aligns with the holistic nature of pediatric care, amplifying the significance of a patient-centered paradigm that extends from the precipice of anticipation to the pinnacle of recuperation. The nuanced orchestration of these interventions promises a more seamless trajectory for pediatric patients, fostering a continuum of care that is both holistic and deeply resonant with their individual needs.
Table: Key Findings of Preoperative and Postoperative Interventions. “Table summarizing significant outcomes from preoperative and postoperative interventions, highlighting their impact on pediatric patients’ surgical experience and recovery.”
5.2 Factors Influencing the Effectiveness of Nonpharmacological Approaches
The effectiveness of nonpharmacological approaches in pediatric surgical care is intricately woven into a tapestry of multifaceted factors that intersect with the unique needs and characteristics of each patient. Among these influential elements, patient age stands as a key determinant. Developmental considerations are paramount, as interventions must be tailored to match the cognitive, emotional, and social capacities of children at different stages of growth. A strategy that resonates with a preschooler might not necessarily engage a teenager, thus emphasizing the importance of age-appropriate customization. Closely intertwined with age, cognitive development exerts its influence. The ability to comprehend, process, and engage with interventions differs across age groups, impacting their potential efficacy ( Suleiman‐Martos et al., 2022). Equally influential is the individual’s disposition and preferences. Recognizing that each child possesses a distinct personality and set of preferences, interventions must be flexible enough to cater to these individual inclinations, optimizing engagement and responsiveness.
Beyond the individual, family dynamics shape the terrain of effectiveness. Familial involvement, support, and receptiveness to interventions profoundly influence their impact. Cultural considerations play a significant role, as interventions must align with cultural norms and beliefs to ensure meaningful engagement and acceptance. Healthcare provider expertise and communication skills also emerge as critical factors, as a practitioner’s ability to guide, explain, and execute interventions affects their reception by patients and families. Crucially, tailoring interventions to the specific surgical context is paramount. Different surgical procedures entail varied physical and emotional challenges, demanding interventions that resonate with the specific nuances of each situation. Adapting interventions to encompass the immediate postoperative period, including the type and location of incision, can significantly enhance their relevance and efficacy.
Chapter 7: Conclusion and Recommendations
6.1 Summary of Findings
In this study, I have taken the time to carefully and thoroughly investigate the use of nonpharmacological interventions in pediatric surgical care. Prior to and following surgical procedures, the primary focus was on understanding the profound significance and far-reaching impact of these interventions for young patients. The scope of the systematic review included many different types of interventions that are all important parts of the pediatric surgical process.
Nonpharmacological interventions are a rich tapestry spanning the spectrum of pediatric surgical care, and the study’s findings reflected this. Play therapy and other forms of preoperative psychological preparation have emerged as game-changing tools, equipping young patients with the emotional fortitude and coping mechanisms they will need to successfully undergo surgery. Parents’ participation and widespread education helped foster a well-informed and encouraging setting.
The effectiveness of pain management, therapeutic play, family-centered care, expressive arts, and physical activity is now being studied after surgery. The convergence of these interventions produced a holistic recovery strategy that considered the many facets of the patient’s condition (Thbeet and Shoq 2022). These interventions facilitated not only pain reduction but also emotional rehabilitation and a quicker physical recovery. To sum up, the results of this dissertation show that nonpharmacological interventions have tremendous potential in the field of pediatric surgical care. These interventions have the potential to radically improve the surgical experience for young patients by addressing their emotional and psychological needs as well as their physical well-being.
The authors of this study have demonstrated the transformative power of a patient-centered and holistic approach to pediatric surgical care by systematically exploring a wide range of interventions and carefully reviewing the existing literature. Both the importance of these interventions and the urgent need to incorporate them into the broader healthcare landscape are brought into focus by the results. Ultimately, these results are a call to action for the medical establishment to alter the status quo of pediatric surgical care by recognizing the many advantages of nonpharmacological interventions.
6.2 Contribution to Pediatric Surgical Care
The findings of this study, taken as a whole, illustrate the substantial and game-changing role that nonpharmacological interventions play in the field of pediatric surgical care. The findings show that these interventions are not optional extras but rather crucial building blocks for an integrative and patient-centered healthcare strategy. Psychological preparation and play therapy are two examples of effective preoperative interventions that help young patients face the prospect of surgery with emotional strength. Psychological preparation gives patients a sense of control over the surgical process through individualized communication, reducing anxiety and promoting coping mechanisms. However, play therapy uses the child’s natural tendency to use play as a means of emotional expression to help them work through their worries in a nurturing setting.
Parental involvement and education emerge as pillars that fortify the foundation of pediatric surgical care. The inclusion of parents not only reassures the child but also provides a vital source of emotional support. Education equips families with knowledge, enabling informed decision-making and reducing uncertainties surrounding the surgical journey. In the postoperative phase, the continuum of care is upheld through interventions aimed at nurturing recovery and rehabilitation. Pain management techniques, such as distraction and relaxation, tangibly alleviate discomfort while promoting emotional well-being. Therapeutic play enables children to express and navigate their emotions, facilitating emotional healing. The emphasis on family-centered care acknowledges the significance of the family unit in the recovery process, fostering an environment of emotional support and comfort (Mohamed Bayoumi et al., 2020). Expressive arts and physical activity provide creative outlets that positively impact mood and accelerate rehabilitation.
The holistic approach endorsed by these interventions epitomizes a comprehensive understanding of pediatric surgical care—one that accounts for the intricate interplay of emotional and physical dimensions. By addressing not only the surgical procedure but also the broader experience, these interventions foster an environment of healing that encompasses the entirety of the child’s well-being.
Implications for Clinical Practice and Future Research
The insights gleaned from the study cast a spotlight on the transformative potential of nonpharmacological interventions within the landscape of pediatric surgical care. The integration of these interventions into clinical practice holds profound implications for optimizing patient outcomes and fostering a holistic healing milieu. The study underscores the value of adopting a family-centered approach, acknowledging the pivotal role of families as integral components of the care journey. In clinical practice, the findings advocate for a paradigm shift towards a comprehensive care model that embraces nonpharmacological interventions (Gumus et al., 2020). Incorporating psychological preparation, play therapy, parental involvement, education, pain management strategies, therapeutic play, family-centered care, expressive arts, and physical activity within the treatment repertoire can revolutionize the patient experience. The integration of these interventions aligns with a patient-centered ethos, empowering children and families, mitigating anxiety, and accelerating recovery.
Future research avenues are illuminated by the study’s revelations. Refining intervention protocols emerges as a logical progression, delving deeper into the intricacies of tailoring interventions to individual patient characteristics, surgical contexts, and developmental stages. Investigating the long-term impact of nonpharmacological interventions on patient outcomes is crucial, shedding light on sustained benefits, potential challenges, and areas for enhancement.
Additionally, the exploration of novel techniques and innovations is pivotal. The landscape of nonpharmacological interventions is dynamic, with emerging technologies and creative approaches continually redefining the possibilities. Research into these uncharted territories can unearth novel avenues for intervention, shaping the evolution of pediatric surgical care.
References
Mathias, E.G., Pai, M.S., Guddattu, V. and Bramhagen, A.C., 2022. Nonpharmacological interventions to reduce anxiety among children undergoing surgery: A systematic review. Journal of Child Health Care, p.13674935211062336.. https://journals.sagepub.com/doi/abs/10.1177/13674935211062336
Thbeet, H. and Shoq, A.H., 2022. Effectiveness of Nonpharmacological Pain Management On Children Post-Surgery. Mosul Journal of Nursing, 10(3), pp.206-211. https://mjn.mosuljournals.com/article_175556_13601.html?lang=ar
Pester, B.D., Yoon, J., Yamin, J.B., Papianou, L., Edwards, R.R. and Meints, S.M., 2023. Let’s Get Physical! A Comprehensive Review of Pre-and Post-Surgical Interventions Targeting Physical Activity to Improve Pain and Functional Outcomes in Spine Surgery Patients. Journal of Clinical Medicine, 12(7), p.2608. https://www.mdpi.com/2077-0383/12/7/2608
Suleiman‐Martos, N., García‐Lara, R.A., Membrive‐Jiménez, M.J., Pradas‐Hernández, L., Romero‐Béjar, J.L., Dominguez‐Vías, G. and Gómez‐Urquiza, J.L., 2022. Effect of a game‐based intervention on preoperative pain and anxiety in children: A systematic review and meta‐analysis. Journal of Clinical Nursing, 31(23-24), pp.3350-3367. https://onlinelibrary.wiley.com/doi/abs/10.1111/jocn.16227
Gumus, K., Musuroglu, S., Ozlu, Z.K. and Tasci, O., 2020. Determining the use of nonpharmacologic methods by surgical nurses for postoperative pain management and the influencing professional factors: A multicenter study. Journal of PeriAnesthesia Nursing, 35(1), pp.75-79. https://www.sciencedirect.com/science/article/pii/S1089947219302679
Komann, M., Weinmann, C., Schwenkglenks, M., & Meissner, W. 2019. Nonpharmacological Methods and Postoperative Pain Relief: An Observational Study. Anesthesiology and Pain Medicine, In Press(In Press). https://doi.org/10.5812/aapm.84674
Agbayani, C.-J. .G., Fortier, M. A., & Kain, Z. N. 2020. Nonpharmacological methods of reducing perioperative anxiety in children. BJA Education, 20(12), 424–430. https://doi.org/10.1016/j.bjae.2020.08.003
Castellano-Tejedor, C. 2022. Nonpharmacological Interventions for the Management of Chronic Health Conditions and Non-Communicable Diseases. International Journal of Environmental Research and Public Health, 19(14), 8536. https://doi.org/10.3390/ijerph19148536
Mohamed Bayoumi, M.M., Khonji, L.M.A. and Gabr, W.F.M., 2021. Are nurses utilizing nonpharmacological pain management techniques in surgical wards? PLoS One, 16(10), p.e0258668. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0258668
Elsayed, Z.E.H., Elhalafawy, S.E.H. and Elsharkawy, M.H., 2023. Upgrading Nurses’ Knowledge, Attitude and Self-Efficacy Toward Pharmacological and Nonpharmacological Pain Management in Children. Tanta Scientific Nursing Journal, 30(3), pp.63-76. https://journals.ekb.eg/article_307374_de199fff146b0b72dd3e51da1a4bd55d.pdf
Tekletsadik, E.A., Desta, A.A. and Workneh, B.S. (2021). Knowledge, Attitude, and Associated Factors towards Nonpharmacological Pain Management among Nurses Working at Amhara Region Comprehensive Specialized Hospitals, Ethiopia. Critical Care Research and Practice, 2021, pp.1–11. https://doi.org/10.1155/2021/7374915
 write
write