Abstract
Drug addiction problems are severe in society today. Many intervention measures are required to meet the need to stop the patients’ addiction. Drug addicts habitually take the same drug for a while and relapse after intervention measures. The association of drug addiction to the functions and parts of the brain significantly impacts the research of drug addiction in the subject of neural science. Neuroscience research has demonstrated that addiction is a chronic, relapsing brain disorder caused by repeated drug exposure in persons susceptible to the disease due to their genetic composition, upbringing, or social stress impacts. This study’s scientific question is how addiction alters neural networks in the brain. Addiction is a chronic disease that changes people. This research attempts to answer the scientific question/problem of determining how alterations in neural networks in the brain can be caused by addiction. The paper will discuss the role of various brain regions and neurotransmitters in addiction, such as dopamine, mesolimbic pathways, and the amygdala. The main finding to take away from this research is that addictive drug use can alter neural pathways in the brain, which can result in addiction. The reward system in the brain undergoes modifications when medicines increase dopamine release. They like it and feel good about it. These modifications may persist over time and result in decisions motivated by the desire to buy drugs. Addiction can also result from hereditary and environmental factors. Addicts are more prone to develop in families with a history of addiction.
Key Words: Addiction, Neural Pathways, prefrontal cortex, Amygdala, and Mesolimbic Pathways
Introduction
Background Information
In modern society, addiction is among the world’s major public health problems, associated with many negative impacts, such as chronic diseases. Extreme conditions lead to mental health conditions. Drug addiction is a complex disorder that can cause a chronic disorder characterized by the compulsive need to seek and use drugs despite the negative and harmful effects of drug abuse (Uhl et al., 2019). It leads to negative emotional states such as anxiety, dysphoria, or irritability when an individual cannot access the drug. Many neurotransmitters, including dopamine, glutamate, endogenous opioids, serotonin, gamma-aminobutyric acid (GABA), noradrenaline, and nitric oxide, all play important parts in the physiological underpinnings of addiction (Uhl et al., 2019). These neurotransmitters are frequently imitated by addictive substances to produce the desired effects.
According to the DSM-5 of 2013, addiction is encompassed under the common term of a substance use disorder, with addiction being severe. Even though several factors contribute to the development and maintenance of addiction, changes in the brain’s neural pathways are the key factor contributing to addiction (Strathearn et al., 2019). The key areas of the neural pathways involved in addiction include; the mesolimbic reward pathways, the amygdala, and the prefrontal cortex (Strathearn et al., 2019).
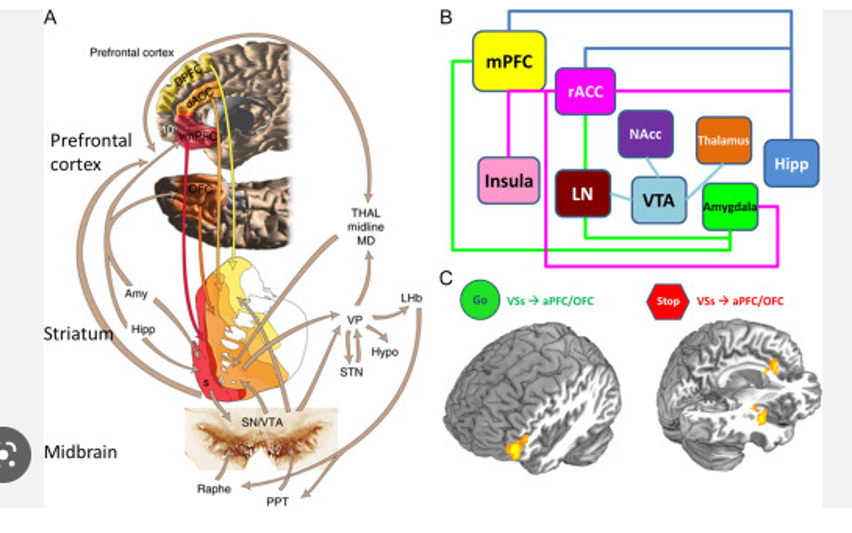
The mesolimbic reward pathways, which comprise the prefrontal cortex, the nucleus accumbens, and the amygdala, refer to a pathways system in the brain responsible for regulating motivation and rewards. This pathway is important because it regulates several cognitive processes, such as fear and learning (Serafini et al., 2020). When an individual abuses drugs, these drugs hijack the pathway leading to the release of excess dopamine, which causes euphoria, hence the reinforcement of drug use (AL et al., 2020). As individuals abuse drugs over time, the drugs cause the function and structure of this pathway to change which may lead to addiction. The prefrontal cortex, responsible for impulsive control and decision-making, may become less effective in controlling drug-seeking behaviors when an individual is addicted to drugs. The amygdala is responsible for emotional processing, and it can contribute to drug addiction by reinforcing the use of drugs to respond to emotional triggers or stress (Strathearn et al., 2019).
The relationship between having alterations in the brain’s neural pathways and addiction The specific medications that have a greater impact on addiction require additional study. There is a literature gap in addressing the exact areas of the brain and the addictions that affect the area of the brain part (AL et al., 2020). Further research is needed to comprehend how genes, environment, and brain neural networks contribute to drug addiction. The paper will review the literature on addiction neural pathways to understand the research findings better. The main research questions focus on the brain reward system, dopamine’s role, and addiction’s impact on other neurotransmitters (Drug, 2014). The information learned will help in developing and recommending necessary intervention measures. The information will fill the gaps in knowledge surrounding addiction and neural pathways.
Research Question
This research paper aims to investigate how changes in neural pathways such as the prefrontal cortex, the amygdala, and the mesolimbic reward pathway contribute to the development of addiction. It will further investigate how this knowledge can be used to develop more effective intervention plans for addiction.
Problem Statement
The main purpose of this research paper is to explore the relationship between neural pathways and addiction, particularly focusing on how the underlying mechanisms of neural pathways lead to addiction. Addiction is a major global public health issue with widespread negative social and health impacts affecting millions globally. Despite much literature being published about the relationship between the two, much is still not understood about how the underlying mechanisms of neural pathways cause addiction. The central problem that will be addressed in this research paper is the need to understand better how the brain neural pathways involved in addictive behavior relate to one another and how they influence the development of addiction. Reviewing the existing literature makes it possible to identify gaps in the current knowledge pool and highlight which areas require future research. The ultimate goals of this paper are to provide deeper insights into the underlying mechanisms of addiction and provide potential implications for treatment.
The motivation for studying the Research Topic
Addiction remains a devastating and complex condition affecting millions of individuals globally; therefore, understanding the neural mechanisms of addiction can help develop better intervention and treatment options for handling addiction. Additionally, addiction is associated with negative economic and social negative consequences such as productivity loss, healthcare costs, and critical health conditions. By studying this relationship, it is possible to gain insights into addiction’s economic and social costs and develop policies and intervention strategies to reduce them. Therefore, the motivation behind studying this relationship is to understand how the negative consequences of addiction can be reduced and how it can be treated.
Literature Review
Several studies have been conducted to understand the relationship between neural pathways and addictions. These studies form a basis under which more research on the topic can be carried out, and they contribute more knowledge about the relationship. Most of the available literature has focused more on how changes in neural pathways of the mesolimbic reward pathways, such as the amygdala and the prefrontal cortex, contribute to the development and maintenance of addiction (Serafini et al., 2020). The mesolimbic reward pathway, the neural pathway responsible for dopamine release, is a neurotransmitter in the brain associated with pleasure and reward.
Various behavioral and physiological changes in the brain occur due to the complicated condition known as addiction. It is characterized by compulsive substance usage and seeking out despite negative effects. According to neuroscience, addiction alters brain neuronal circuits and neurotransmitter systems (Drug, 2014). This literature review examines addiction-related brain circuits and their function. Addiction research focuses on the brain reward system. In reaction to pleasure, the nucleus accumbens (NAc) releases dopamine. Cocaine and amphetamines increase NAc dopamine release, making people feel euphoric and want more drugs. According to other research, chronic drug use can permanently alter the reward circuit, reducing dopamine receptors and intrinsic reward sensitivity. Addiction may also result from the stress circuit. Dopamine produces corticotropin-releasing factors in response to stress. The experiments on animal addiction models found that dopamine stimulates drug-seeking behavior and brain dopamine release. The addict may experience greater emotional repulsion and longing.
The reward system in the active brain plays a crucial role in the natural selection of activities such as eating, drinking, engaging in sexual activity, etc., and maintaining these activities. According to Serafini et al. (2020), several psychotropic drugs, particularly those that stimulate the brain’s reward system, are linked to compulsive and repetitive behaviors. Serafini et al. (2020) explain that dopaminergic cells that fire in the ventral tegmental area (VTA) and extend to the prefrontal cortex from the nucleus accumbens make up the mesocorticolimbic dopaminergic pathway in the brain.
The pleasurable feelings from increased dopamine are the major driver of addiction. Users of drugs are not more susceptible to the rewarding effects of the substance, despite the widespread belief to the contrary. The study by AL et al. (2020) has shown that people addicted to substances see substantially smaller increases in their dopamine levels than people who are not addicted to the same substances. A lack of dopamine reduces the brain’s receptivity to rewards, which leads to a diminished level of enjoyment.
Another important component of the neural pathway that significantly impacts the development and maintenance of addiction is the prefrontal cortex. This cortex is a brain region responsible for regulating emotions, decision-making, and control of impulses (Strathearn et al., 2019). According to Takahashi et al. (2021), chronic use of drugs leads to changes in the prefrontal cortex which causes an individual to have a reduced ability to make decisions, an unstable emotional state, and an inability to control impulses. This study further argues that due to the decreased activity in this region, individuals will continue using drugs to help them feel better, leading to addiction.
It has been noted by Uhl et al. (2019) that changes in the prefrontal cortex often lead to cue-induced cravings, which can cause relapses in people getting treated for addiction. Several interventions can help treat addiction caused by decreased prefrontal cortex activity, as discussed by Horseman & Meyer (2019). Their study suggests that effective prefrontal cortex-induced addiction treatment should target the cortex. Some of the intervention or treatment plans may include cognitive-behavioral therapy.
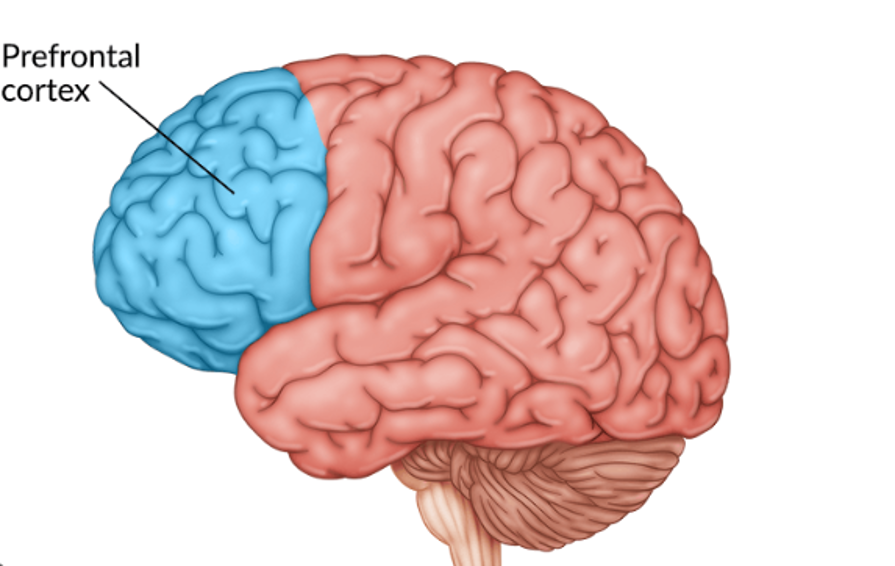
Studies have indicated that persistent drug use might decrease Prefrontal cortex activity and worse decision-making. The Prefrontal cortex is crucial for executive processes like decision-making and impulse control. This could be a factor in the obsessive drug-seeking behavior that characterizes addiction. Drug addiction alters a variety of neuronal circuits in the brain, and the underlying processes causing these changes have been investigated in a number of first-hand research investigations (MacNicol, 2016). In 2016, Koob and Volkow revealed their research on how the brain functions that cause addiction. They believed switching from receiving good rewards to receiving poor ones was necessary to transition from taking drugs to becoming addicted. According to scientists, chronic drug use throws the reward system out of whack. The brain’s stress and anti-reward circuits are activated as a result. This cycle will continue as long as the person continues to use drugs. The obsessive drug-seeking behavior exhibited in addiction may be explained by switching from positive to negative reinforcement.
The amygdala is a brain region responsible for emotions and memories. Emotions such as fear, happiness, sadness, and anxiety are processed in the amygdala. Continued drug use changes the function and structure of this region by reinforcing the use of drugs as individuals process emotions (Strathearn et al., 2019).
Therefore, from the above literature review, it is evident that changes in some of the neural pathways in the brain, such as the amygdala, prefrontal cortex, and the mesolimbic reward pathway, all contribute to the development and maintenance of an addiction. Another part of the brain involved in addiction is the prefrontal cortex (PFC). Studies have indicated that persistent drug use might decrease PFC activity and worse decision-making. The PFC is crucial for executive processes like decision-making and impulse control. This could factor in the obsessive drug-seeking behavior that characterizes addiction (MacNicol, 2016). Drug addiction alters a variety of neuronal circuits in the brain, and the underlying processes causing these changes have been investigated in a number of first-hand research investigations. In 2016, Koob and Volkow revealed their research on how the brain functions that cause addiction. They believed switching from receiving good rewards to receiving poor ones was necessary to transition from taking drugs to becoming addicted. According to scientists, chronic drug use throws the reward system out of whack. The brain’s stress and anti-reward circuits are activated as a result. This cycle will continue as long as the person continues to use drugs. The obsessive drug-seeking behavior exhibited in addiction may be explained by switching from positive to negative reinforcement.
Integration of the study findings
From the above literature review, several studies support the research hypothesis that changes in the neural pathways, such as the amygdala, prefrontal cortex, and mesolimbic reward pathway, can significantly contribute to addiction. From the literature review above, it is evident that repeated use of drugs affects the function of the mesolimbic reward pathway, reducing an individual’s sensitivity to natural rewards and dopamine levels; hence they have to seek artificial rewards such as drug use.
The literature review has also added knowledge to the current understanding of some plans and interventions to help manage and treat addiction. From the review, it is evident that to treat addiction effectively, it is important to adopt treatment plans that target the specific part of the brain that has contributed to addiction. Treatment plans such as exposure, behavioral-cognitive and behavioral therapies can all be used in treating and managing addiction and preventing relapsing. Therefore, these studies have provided significant findings and evidence that help better understand the relationship.
The research question examined how changes in the neural pathways, such as the prefrontal cortex, the amygdala, and the mesolimbic reward pathway, contribute to the development of addiction. The important research publications on neural pathways and addiction provide a comprehensive understanding of the subtle changes that occur in the brain during addiction. Prolonged drug use can result in permanent changes to the reward system, stress route, and prefrontal cortex, all involved in addiction.
According to the findings, addiction also involves a change from positive to negative reinforcement. Persistent drug use dysregulates the reward system and activates the stress and anti-reward pathways. Targeting these modifications may be a viable method for developing effective medicines. Targeting these changes may be a potential strategy for creating efficient treatments. Alterations in synaptic plasticity and epigenetic pathways may also contribute to the persistent nature of addiction.
The combination of these research results emphasizes the necessity for a thorough knowledge of the brain mechanisms behind addiction and the significance of creating focused therapies that address the various pathways implicated in addiction. It may be able to create interventions for this complicated condition that are more successful by targeting the underlying changes in the brain that occur during addiction. Therefore, health professionals can benefit from this research because they can understand how addiction occurs and develops and the plans and strategies to treat this complex disorder. However, neuroscience issues keep evolving; therefore, more research is needed to continue explaining how the brain’s neural pathways interact with one another and how they cause addiction.
Conclusion
This research paper has explored the complicated relationship between addiction and neural pathways. The paper has discussed how various neural pathways, such as the mesolimbic reward pathway, amygdala, and prefrontal cortex, play a significant role in developing and maintaining an addiction. Specifically, the paper has explored how the changes in mesolimbic reward pathways, prefrontal cortex, and amygdala cause addiction due to a reduction in dopamine levels, unstable emotional state, inability to control impulses, and the inability to process emotions significantly.
The research paper findings show that drug addiction is a complex disorder that alters the normal functions of the brain’s neural pathways, and it is not a sign of moral weakness or personal choice. Other research articles have evaluated that addiction also involves a change from positive to negative reinforcement. The target of these elements, especially the neural pathways linked with addiction, would help develop effective treatments. Before developing the treatment methods needed, plans that address the specific part of the brain that facilitates addiction should be laid first. Therapy methods such as behavioral-cognitive, behavioral, and exposure assist in treating and preventing addiction. This research reveals that continued drug use might affect brain networks that lead to addiction, but it is unclear if therapy can restore these changes. Addiction’s long-term impacts on the brain and behavior and whether neural circuit therapies might cure them could be studied. Research might also examine the effects of combining medications and behavioral therapy to target numerous brain circuits and improve recovery odds.
Therefore, in summary, the paper has highlighted how changes in neural pathways cause addiction by providing deeper insights into the biological mechanisms that drive this relationship. By identifying the specific neural pathways involved in addiction, the study opens more opportunities for effective treatment plans for millions of individuals struggling with addiction. The research can potentially improve many lives of people struggling with addiction, improving society’s well-being and overall health.
References
AL, O., EX, F., RIMENTAL, P., BASIC, M. E. I., & IEN, S. (2020). Etiology of Addiction and Dopamine. Journal of Experimental and Basic Medical Sciences, 1(1), 28-31.
Horseman, C., & Meyer, A. (2019). Neurobiology of addiction. Clinical obstetrics and gynecology, 62(1), 118–127.
Serafini, R. A., Pryce, K. D., & Zachariou, V. (2020). The mesolimbic dopamine system in chronic pain and associated affective comorbidities. Biological psychiatry, 87(1), 64-73.
Strathearn, L., Mertens, C. E., Mayes, L., Rutherford, H., Rajhans, P., Xu, G., … & Kim, S. (2019). Pathways relating the neurobiology of attachment to drug addiction. Frontiers in psychiatry, 10, 737.
Takahashi, T. T., Ornello, R., Quatrosi, G., Torrente, A., Albanese, M., Vigneri, S., … & Martelletti, P. (2021). Medication overuse and drug addiction: a narrative review from an addiction perspective. The journal of headache and pain, 22(1), 1-11.
Uhl, G. R., Koob, G. F., & Cable, J. (2019). The neurobiology of addiction. Annals of the New York academy of sciences, 1451(1), 5–28.
The drug, in. (2014). Neuroscience. Nih.gov; National Academies Press (US). https://www.ncbi.nlm.nih.gov/books/NBK232964/
MacNicol, B. (2016). The biology of addiction. Canadian Journal of Anesthesia/Journal Canadien D’anesthésie, 64(2), 141–148. https://doi.org/10.1007/s12630-016-0771-2
 write
write