Background/introduction
The term ‘breast cancer’ refers to several sub-types whose expressions differ in clinical presentation, gene expression, and the nature of genetic and molecular features. Although a rare case among males, this type of cancer, which manifests as malignant growths on breast tissues, is not exclusive only to women. Burden Breast represents the most common type of cancer in most cases and is the second leading cause of death from all cancers among most women. It is also the leading cause of death in women ranging between 40 and 59 years old (Angahar, 2017). Understanding the complex bio-molecular and genetic aspects of breast cancer leads to comprehending what makes it a disease. In addition, an analysis of recent information and figures gives insight into the scale of such a phenomenon in society. This exploration aims to understand the complicated elements of breast cancer, including its pathophysiology, epidemiology, burden, present studies as well and newly emerging treatment methods, all of which constitute the groundwork upon which battling cancer is based today.
Pathophysiology of the disease
Breast cancer is an intricate disease that results from DNA damage as well as exposure of certain genes to estrogen on some occasions. The genetic predisposition cannot be overlooked either. Having faulty or overactive tumor suppressor genes, for example, BRCA1 and BRCA2, especially when there is a family background of breast cancer, increases the probability significantly (Pandrangi et al., 2022). Under natural conditions, the immunity system can tag and destroy cells with anomalous DNA or growth rates but fail to contain breast-cancer tumor proliferation as is usually the case.
Estrogen is one of the hormones involved in multiple biological systems, and it contributes greatly to the physiopathology of breast cancer. During their pre-menopause stage, women mainly produce estrogens in their ovaries, wherein gonadotropin–releasing hormone (GnRH) is secreted and stimulates the discharge of LH and FSH. FSH stimulates estrogen production in the growing ovarian sacs, affecting LH production in the brain (Pandrangi et al., 2022). Following the menopause, the ovaries begin producing very small amounts of estrogen. Some factors, such as early menstruation cancers and late menopause, have a great influence on this disease, showing the significance of hormonal secretion during breast growth and tumor generation. However, some basal-like tumors belong to a group called triple-negative breast cancers that are without estrogen receptor, progesterone receptor, and HER2 expression. About one out of three basal-like breast carcinomas do not meet the triple negative definition as they are differentiated on the basis of genetic expression profiles. Such basal-like tumors are characterized by high levels of expression of some markers (CK5, CK14, caveolin-1, and caix), but low levels of others (estrogen receptor (ER), progesterone receptor, and HER2)
Additionally, lipoproteins are abnormally synthesized by breast cancer cells, leading to inadequate uptake of lipids, which are a source of cholesterol in mammalian cells, resulting in a disrupted membrane formation process, energy utilization, and lipid signaling. Such critical biological activities are involved in cellular metabolism, differentiation, progression, and motility of the cells (Pandrangi et al., 2022). Changes in lipoproteins, plasma cholesterol, and pro-inflammatory signal transductions are also associated with these changes. The role of lipids in breast cancers has mainly focused on epidemiological evidence. Though no causal relations have been demonstrated yet, it highlights how intricate lipid metabolism can be as a cancer treatment risk factor or as a modulatory mechanism.
Data and Statistics
The global incidence of breast cancer is overwhelming and growing, amounting to approximately one million newly diagnosed cases per year among females worldwide and almost one-third (1/3) of all malignancies among women globally (Angahar, 2017). It is also the number one type of cancer among women worldwide and the second-most frequent tumor overall after respiratory cancers. Importantly, about 55% of these instances take place in underdeveloped nations indicating extensive prevalence of breast cancer in different settings.
Breast cancer is the most common of the diagnosed invasive cancers in American women of any race and ethnicity. For instance, in 2018, it was expected that close to 266,000 individuals would be diagnosed with invasive breast cancer and more than 64,000 persons would have non-invasive breast cancer. In January 2018, there were approximately 3.1 million women in the US alone with personal histories of breast cancer (active or expired) (Feng et al., 2018). There has been a stable trend in the incidence rate of all types of breast cancer despite the decline from 2000 to 2003, including ER-positive ones amongst the US women population.
Around 95% of the identified cases are reportedly among women of age more than 40 years. A woman is likely to get an invasive breast cancer diagnosis within the time range of 10 years or more, which underscores its prevalence since its chance lies between 4-13% (1 out of every 8) (DeSantis et al., 2019). At age-specific analysis, women aged 70 years old are at the highest risk of a breast cancer diagnosis, whereas women aged 80 years old are at the highest risk of breast cancer death.
Additionally, in the United States, disparities in breast cancer diagnosis and outcomes exist across racial and ethnic lines. Among others, the Hispanic ethnicity and the black race both of which indicate later-stage breast cancer diagnoses. In most cases, black women get these more aggressive forms of breast cancer that present themselves as estrogen receptor-negative tumors. It is worth noting that the percentage of triple-negative tumors (ER-negative, PR-negative, and HER2-negative) is greater among premenopausal black women than in white counterparts (2.8% annually). There is an elevated incidence rate of HR-positive breast cancer among black and AIAN women; however, the rate for HR-negative tumors has significantly dropped across all ethnic/racial groups, suggesting new trends in specific types of breast cancer in the diverse population.
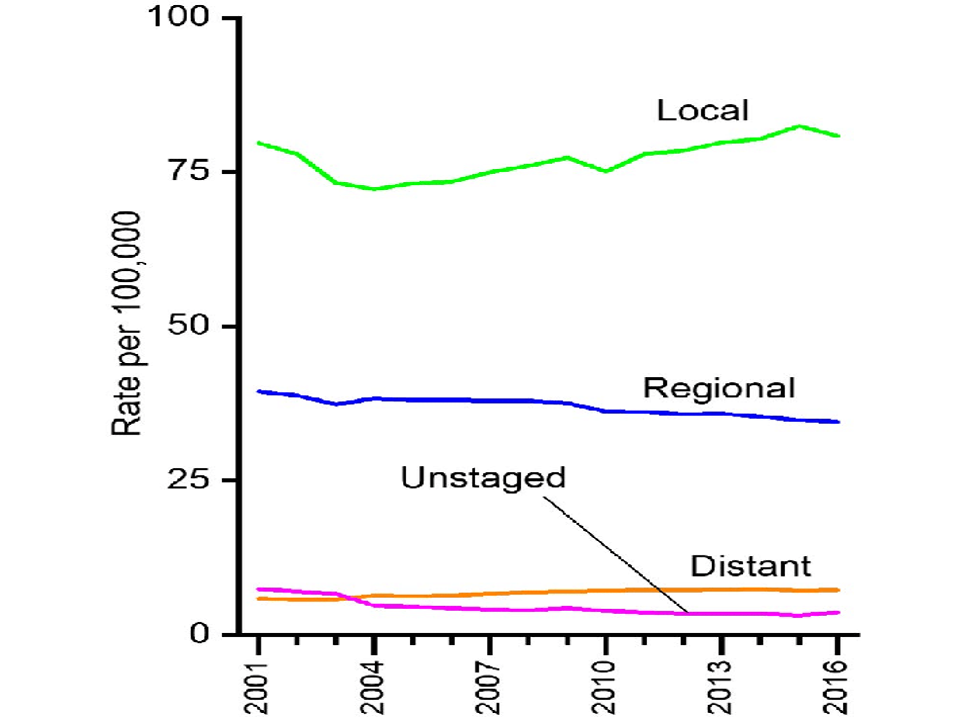
Fig 1: Analysis of Female Breast Cancer Incidence Rates at Diagnosis, United States, from 2001 to 2016 (DeSantis et al., 2019)
Recent research and possible treatment
In detecting breast cancer, a complicated illness with different approaches can be done by employing mammograms or specific X-rays. However, breast cancer can also be detected early with uncommon lumps that women identify themselves with or together with physicians (Angahar, 2017). Changing the appearance of either the skin or the nipple is very rare, yet one of the early signs that can be encountered by some patients who are suffering from breast cancer, hence demonstrating a wide spectrum of expression for the disease.
Treatment options for breast cancer are diverse and depend on different parameters, such as the severity of the disease and the general health condition of a person. These options include surgical techniques such as lumpectomy, meaning removal of the lump, or mastectomy implying that the whole breast is removed and the adjoining tissue (Tong et al., 2018). The surgeon decides based on the stage and type of the specific cancer, but only after consultation with the patient’s physician.
One of the major treatment options for cases relating to hormonal receptor breast cancers and hormone therapies is known as endocrine therapy, which acts either by suppressing or reducing hormone levels. Some of the notable drugs in this class include tamoxifen, which is a product that blocks the entry of estrogen into this receptor, aromatase inhibitors that suppress the hormones derived in the ovary that lead to estrogen depletion, and luteinizing hormone (Tong et al., 2018). This calls for the administration of the above medicines in sequence until a rapid response or clinical resistance necessitates the incorporation of chemotherapy. There are variable reports of response to combining varying endocrine drugs for improved anticancer effects. In general, most people believe that patients with endocrine therapy-naive advanced breast cancer and those with very sensitive endocrine tumors will get the maximum benefit from combination endocrine therapy.
Triple-negative breast cancer (TNBC) is more challenging as it poses a complex picture that is difficult to address due to its inherent aggressiveness and resistance to treatment compared to HRM+ and HER2+ breast carcinomas. The only established approach in therapy for TNBC is standard chem therapy showing up 22% as the highest CR of chem (Tong et al., 2018). However, TNBC occurs more often in breast cancer recurrences and distant metastases compared to non-NBC tumors. The lack of well-defined molecular targets leads to poor therapeutic options in TNBC, thus highlighting the necessity of exploring new therapeutic targets and formulating potent targeted agents. This importance implies that TNBC is very intricate, making it necessary to develop even more targeted approaches that could combat this extremely aggressive breast cancer form.
Discussion
Numerous epidemiologic studies show that being physically active regularly is a major way of lowering one’s risk for breast cancer. Interestingly, the Women’s Health Initiative Cohort Study, wherein 74,171 women between 50 and 79 were involved, gave credible insights. At age 35 years, there was noted 14% decrease in the risk of breast cancer among women involved in intensive exercise as compared with those being physically inactive (Coughlin, 2019). However, slightly reduced similar risk reduction levels were noted at age 18 and 50 years for vigorous exercise. Furthermore, in terms of the time spent on physical activity, it was found that prolonged periods were more effective than short ones. This could be explained by physical activity-related changes in body composition, insulin resistance, and some additional sex steroid hormones that altogether form a general concept about the influence of physical activity on lowering the risk for breast cancer.
Other predisposing factors include age at menarche, parity, and age at first live birth. As with other cancers associated with reproductive factors, younger age at menarche and null parity and older age at first full-term pregnancy in breast cancer are well-recognized risks. Breast cancer is a disease that has a history of development in women before menopause. Cell proliferation and DNA damage are also influenced by reproductive hormones like estradiol, which could promote cancer. Women who had menarche beyond the age of 14 years were found to have a 6% lower level of circulating estradiol compared to those who reached puberty below the age of 12 years (Coughlin, 2019). Older women are at increased risk of developing breast cancer, with null parity being emphasized as a protective factor—pregnancy-inflicted persistent modification of the mammary gland results in decreased susceptibility to carcinogenic factors. Notably, an earlier age at first recorded childbirth is seen as protective. The interrelationship between reproductive factors and breast cancer risk helps to understand the complex biology involved in the formation of this condition.
Diet greatly affects breast cancer risk due to some nutrients that increase cancer risk. The intake of high fat becomes a contributing factor that increases the chances of developing breast cancer in women (Coughlin, 2019). The consumption of diets rich in fat, caffeine, and red meats increases the incidence of breast cancer risk. In contrast, evidence suggests that a diet rich in fruits and vegetables can effectively protect against the onset of breast cancer. Also, taking the necessary daily amount of phytoestrogens, calcium, and vitamin D can diminish the risk of developing breast cancer. The nutritional considerations emphasize the role played by lifestyle choices in breast cancer outcomes, to adopting healthy diets can aid in reducing breast cancer risk.
The presence of a positive family history of breast cancer is considered one of the most established risk factors for the disease. When a woman has one first-degree relative with breast cancer, her risk increases about twice as much. This risk increases as the age of the relative at the time of diagnosis rises up and if there are many more first degree relatives also diagnosed with breast cancer. About 20% of women who suffer breast cancer have a close family member with the same condition (Coughlin, 2019). However, less than ten percent and hardly more than five percent of hereditary Breast Cancer that stems from a first-degree relative has an autosomal pattern. In such cases, separate traits like duality, early onset, and involvement of several generations have been observed. Thus, it is important to mention that most breast cancers constitute non-genetic types and do not link with high-rate gene mutation. By understanding the peculiarities involved in the family history of breast cancer risk assessment, it becomes easier for patients and healthcare professionals to develop patient-specific methods of prevention, screening, and identification.
Conclusion
The risk of breast cancer depends on many different things that cause the illness to appear complex and multi-faceted. These factors include genetic predisposition and reproductive history, lifestyles, and exposure to the environment, among others, that must be understood for efficient preventive measures, early detection, and targeted treatments. Interacting genetic and environmental factors emphasize the role of comprehensive risk profiling and customized strategies for preventing and controlling breast cancer. Research keeps improving as we know more about genes, how they interact, and how our physical activities and eating patterns contribute. Although there is a component of familial susceptibility and mutations in tumor suppressor genes, an overwhelming proportion of breast cancers is non-familial and, therefore, requires a global approach to prevention. Therefore, in the battle against breast cancer in the world, it is vital efforts to spread information about healthier lifestyles and improve diagnosis, screening methods, and treatment programs. Enabling information on risks and promoting a teamwork methodology between health workers, research experts, and the community is instrumental in lowering the impact of this prevalent and fatal condition.
References
Angahar, L. T. (2017). An overview of breast cancer epidemiology, risk factors, pathophysiology, and cancer risk reduction. MOJ Biol Med, 1(4), 92-96.
Pandrangi, S. L., Chittineedi, P., Chikati, R., Mosquera, J. A. N., Llaguno, S. N. S., Mohiddin, G. J., … & Maddu, N. (2022). Role of lipoproteins in the pathophysiology of breast cancer. Membranes, 12(5), 532.
DeSantis, C. E., Ma, J., Gaudet, M. M., Newman, L. A., Miller, K. D., Goding Sauer, A., … & Siegel, R. L. (2019). Breast cancer statistics, 2019. CA: A cancer journal for clinicians, 69(6), 438–451.
Feng, Y., Spezia, M., Huang, S., Yuan, C., Zeng, Z., Zhang, L., … & Ren, G. (2018). Breast cancer development and progression: Risk factors, cancer stem cells, signaling pathways, genomics, and molecular pathogenesis. Genes & diseases, 5(2), 77-106.
Tong, C. W., Wu, M., Cho, W., & To, K. K. (2018). Recent advances in the treatment of breast cancer. Frontiers in oncology, 8, 381990.
Coughlin, S. S. (2019). Epidemiology of breast cancer in women. Breast Cancer Metastasis and Drug Resistance: Challenges and Progress, pp. 9–29.
 write
write