Chapter One
Introduction
Context
Effective communication among healthcare personnel is required for favorable healthcare outcomes, patient safety, and high-quality treatment. In the acute admission unit, where patients with complicated medical issues are mostly admitted, effective and clear communication is crucial. The Situation-Background-Assessment-Recommendation (SBAR) tool has been proposed as a useful framework for minimizing mistakes and increasing communication in healthcare.
Nurses are the principal communication connection in the multiplex network of a multidisciplinary healthcare group. Nurses participate in a variety of communication channels, including nurse-patient, nurse-physician, and nurse-nurse. Nurse-to-nurse communication is critical for improving the efficiency and safety of patient care. The handing over communication at the start and conclusion of each shift is the most typical routine type of nurse-to-nurse contact. To maintain continuity of care, outgoing nurses convey pertinent patient information to nurses in other units, new nurses, or the facilities during handover.
Handing over communication may be done interdepartmentally, intradepartmentally, and on a referral basis to other healthcare institutions. Inadequate information or miscommunication during handover can jeopardize patient safety by exposing the patient to unfavorable outcomes and errors, such as delayed patient treatment, medication errors, increased hospital-obtained infections, increased hospital bills, avoidable re-admissions, or death. Misinformation or insufficient communication by healthcare professionals or nurses may result in real or prospective damage to the patient. According to various research, the handing-over procedure by nurses needs to be more organized, error-prone, and informal.
The World Alliance for Patient Safety, the World Health Organization (WHO), the Australian Commission for Safety, the Canadian Council on Health Services Accreditation, the Joint Commission International, and many other national, local, and international healthcare organizations have identified communication as a primary focus. This controversy arose when the Institute of Medicine (IOM) produced a study on patient safety in the year 2000, titled “TO err is human.” The paper raised awareness of hospital mistakes and stated that many might be avoided. As a consequence, the Institute of Medicine advocated for rapid changes in norms, communication, risk assessment, and team performance.
Furthermore, in January 2006, the Joint Commission established a safety target that aimed to improve communication effectiveness among healthcare providers. The safety aim advocated for uniform access to communication as well as the ability to ask and answer to inquiries. Structured communication has since been acknowledged as a core element of health safety and is widely regarded as an important research component worldwide. Several healthcare institutions and hospitals have attempted to reorganize their handover communication in order to comply with World Health Organization and Joint Commission requirements. The research, which was done in Acute Admission Units, Critical Care Units, and Emergency Departments to identify the handover process, found an urgent need for a planned method to delivering patient information by integrating additional, obligatory, and required documentation. The Joint Commission and WHO define structured communication as a process in which content and information about patient safety and care are transmitted clearly from one healthcare worker to the next.
Various handover solutions for structured communication have been established depending on the degree of communication and the situation in which the tool is used. Some of the tools developed to improve communication and patient safety include the Situation, History, Assessment, Recommendations, and Questions (SHARQ), Situation, History, Assessment, Request, Evaluate, and Document (SHARED), Patients, Precaution, Plan, Problems, and Purpose (5Ps), and Situation, Background, Assessment, Recommendation (SBAR), among others.
The situation, Background, Assessment, and Recommendation (SBAR) method is a structured communication technique that is extensively utilized and certified for use in healthcare facilities and hospitals by international accrediting institutes and the World Health Organization. The SBAR tool is intended to help nurses communicate important and accurate patient care and safety information to doctors, as well as to facilitate successful communication during nurse-to-nurse handover. According to researchers, the SBAR tool increases communication, patient information transfer, and safety in non-acute and acute healthcare facilities, including nursing training institutes. The American military created the SBAR tool, which was later adopted by the aircraft industry. This tool was later accepted for use by healthcare professionals, most notably Dr. Michael Leonard, Kaiser Permanente’s medical leader for patient care, to establish a communication paradigm for nurses, physicians, and doctors. SBAR is a certified tool that offers a framework for improving organized communication in hospitals and may be used to nearly any kind of communication between healthcare practitioners. The SBAR tool may be used in nurse-to-nurse communication, doctor-to-nurse communication, debriefing, and handover between physicians. For patient care and safety, it employs forceful communication, situational awareness, and critical language. This blend of nursing and medical communication bridges the gap between the conventional communication strategies of physicians and nurses.
To be successful, a handover or communication tool must be relevant, timely, consistent, accurate, detailed, comprehensive, and succinct. The SBAR, according to the Institute of Healthcare Improvement in the United States, facilitates focused and accessible communication among team members. A comparable research conducted at a rehabilitation facility on the deployment, assessment, and adaption of the SBAR tool revealed that it is still a helpful tool for organizing communication among multidisciplinary rehabilitation teams.
According to the research, a nurse educator used the SBAR instrument to evaluate learners during a post-conference. The study’s findings suggested that the learners gained trust and confidence, which led to the giving of extensive information on patients. The nurse came to the conclusion that the gradual process of learners utilizing SBAR in their exercise would increase their confidence in communicating with physicians, nurses, and doctors. The SBAR tool provides a logical and ordered sequenced technique to increase the learners’ communication abilities, according to research conducted in an academic context utilizing the tool. It also aided the trainees’ critical thinking, problem-solving ability, and confidence.
Structured communication is progressively being introduced and adopted in African hospitals. In South Africa, for example, a healthcare institution used the SBAR tool, which resulted in considerable improvements in communication and patient safety among healthcare personnel. Effective communication is an essential component of patient care policies and safety. Nonetheless, the Ghana Health Services (GHS) advanced strategic policies and objectives to improve patient safety and care, including infection control and prevention, prevention of inappropriate operation sites, enhanced situation reporting systems, and clinical risk management. Although organized dialogue was not totally documented as part of the initiative to improve patient safety, the emphasis was on documentation and case reporting. As a consequence, many Ghanaian healthcare systems avoid using organized communication technologies. As a result, there is a lack in experimental and empirical data in Ghana on the use of structured communication tools such as the SBAR tool. The project aims to provide experimental and empirical proof on the usage of SBAR in Ghanaian hospitals.
1.2 Problem Statement
The major cause of adverse events among healthcare personnel has been identified as miscommunication and misinformation. Effective communication is critical in healthcare systems such as acute admission units, which treat patients with complicated and urgent clinical issues. According to some, the SBAR tool is the most beneficial foundation for decreasing mistakes and boosting communication. Nonetheless, further study is needed to investigate the cultural and utilitarian hurdles to compliance with the SBAR instrument in acute admission units for patients with a National Early Warning Score (NEWS) of five or above.
The present issue is that medical personnel may need assistance in effectively utilizing the SBAR tool for patients. Examining compliance-related issues is critical for improving communication, overall quality of care, and patient safety in acute admission units. For patients with a NEWS score of 5 or above, a thorough investigation of the cultural and utilitarian obstacles to SBAR tool compliance is necessary.
When utilizing the SBAR tool in complex medical conditions, utility hurdles may include ambiguity, lack of knowledge, and time limits. Due to urgent demands and time constraints, healthcare practitioners may be deterred from utilizing the SBAR tool on a consistent basis. Knowledge on how to use the SBAR tool may lead to both right and incorrect use. Furthermore, the urgency of patients with a NEWS score of 5 or above may be the underlying cause of doubt about how to utilize and adapt to the instrument efficiently.
Cultural differences among healthcare providers may result in greater compliance with the SBAR instrument. Power dynamics and hierarchy may inhibit junior personnel from efficiently presenting vital material to senior experts. Communication rules that emphasize speed and brevity may contradict the SBAR tool’s organized approach. Furthermore, nurses, physicians, and doctors may be afraid of negative or blaming repercussions if they disclose concerns about utilizing the SBAR instrument, stopping them from using it completely.
1.3 Main Research Question
This study investigates the variables that restrict SBAR tool compliance in patients with a National Early Warning Score (NEWS) of five or above in an Acute Admission Unit setting. The study’s major research topic is listed below.
What are the cultural and utilitarian hurdles to SBAR tool compliance for patients in an acute admission unit with a NEWS score of 5 or higher?
1.4 Secondary Research Issue
Aside from the major research topic, the study will examine a number of subsidiary research issues.
1) What difficulties do physicians have when applying the SBAR tool for patients with a National Early Warning Score of 5 or higher?
2) What recommendations and strategies may be made to improve compliance with the SBAR tool in patients with a National Early Warning Score of five or higher?
3) How do utility and cultural measures in Acute Admission Units influence SBAR tool compliance?
4) How do healthcare professionals see the value and accuracy of the SBAR instrument in the context of patients with NEWS scores of 5 and above?
5) What are nurses’ thoughts on the implementation of the SBAR tool?
1.5 Design and Methodology
A qualitative study methodology will be used to survey the cultural and utilitarian obstacles that prevent hospitals from using SBAR tools. The qualitative methodology allows for a more in-depth understanding of nurses’ views, attitudes, experiences, and obstacles while utilizing the SBAR tool for patients with a National Early Warning Score of 5 or above.
Semi-structured interviews with nurses working in acute admission units will be used to collect study data. Participants will be able to discuss their SBAR compliance experiences and ideas. The data gathered from the observations and interviews will be processed, enabling a study of the cultural and utility obstacles to SBAR tool compliance to be conducted. The study data will be compiled and analyzed in order to fully comprehend the variables impeding SBAR compliance in acute admission units.
1.6 Importance Of The Research
The outcomes of this study may provide critical information about the cultural and utilitarian hurdles for nurses in SBAR instrument compliance for patients with a NEWS Score of five or above. The SBAR tool’s approval and deployment may increase nurse handover activity; yet, utility and cultural obstacles will impede efficient communication among professionals. The results may persuade hospital administration to remove the hurdles and improve organized communication by utilizing the SBAR tool. This research study may help enhance hospital regulations on the use of SBAR instruments, which will be a better communication tool among healthcare personnel. “The nurses may also be persuaded to give a theoretical framework for teaching nurses on different techniques of handover, as well as to introduce the SBAR tool as a method of handover in nursing practice.” The overall findings of this research will address cultural and utilitarian constraints by employing different approaches to the problem.
Chapter Two
Literature Review
Introduction
Effective communication between healthcare personnel in hospitals is critical for providing high-quality treatment and ensuring patient safety. In hospitals, the Situation, Background, Assessment, and Recommendation (SBAR) tool has been recognized as a useful structured communication tool and framework. Nonetheless, several cultural variables within hospitals or healthcare systems might impede compliance and effective application of the SBAR instrument. This literature review examines the cultural characteristics that impact SBAR tool compliance.
2.2 Cultural considerations
Cultural obstacles are views or attitudes held by healthcare workers about the use of the SBAR instrument. Some healthcare practitioners may consider that utilizing the SBAR instrument contradicts or is unnecessary. Language difficulties may also provide a significant difficulty. Health workers who speak English as a second language may have difficulty communicating successfully using the SBAR tool, particularly if they are inexperienced with medical jargon. Hierarchical structures are also a hindrance. Nurses may experience discrimination and discomfort while utilizing the SBAR tool to transmit medical information to other medical professionals in a higher organizational hierarchy. Addressing these cultural problems necessitates cultivating a culture of enhanced interdisciplinary cooperation as well as establishing a secure space for raising and reporting concerns. Hospitals may encourage SBAR tool compliance, improve outcomes, patient care, and safety, and improve communication in acute admission units by addressing and acknowledging these cultural aspects.
2.2.1 Communication Expectations
SBAR tool compliance may be hampered by current communication practices inside hospitals. In acute admission units, for example, efficiency and swift decision-making are critical characteristics that are emphasized to maintain patient safety. Directness and brevity in communication are highly appreciated due to the necessity for a rapid reaction and feedback. The SBAR tool, on the other hand, requires a precise and systematic approach to information transmission. Resistance may be formed as a result of a mismatch between the SBAR tool’s communication style and current communication standards, which may impede the tool’s gradual adoption.
Power Dynamics and Hierarchy 2.2.2
The hierarchical character of hospitals is one of the major cultural problems impeding SBAR tool compliance. Power dynamics between junior and senior employees may be seen in many hospitals; these discrepancies can impede good communication. Junior staff employees may need assistance providing crucial information using the SBAR tool because they are afraid of questioning senior personnel. The power imbalance precludes transparent and open communication, which is required to properly use the SBAR tool. Again, younger workers may find difficulties in communicating concerns about unfavorable consequences to senior personnel.
2.2.3 Collaboration Across Disciplines
Collaboration of healthcare specialists in many hospital departments is required for the tool’s successful and simple use. Cultural problems, such as a lack of interprofessional teamwork and professional silos, might impede compliance and use of the SBAR tool. Medical practitioners may need assistance in utilizing the SBAR tool to communicate across healthcare professions, especially in facilities where multidisciplinary teamwork is not promoted or encouraged. This cultural barrier may be overcome by improving interprofessional communication and fostering a collaborative culture in which all medical practitioners recognize the importance of the SBAR tool in facilitating multidisciplinary cooperation.
2.2.4 Fear of retaliation and blaming
Medical professionals share a societal dread of blame and vengeance. Healthcare personnel may use the SBAR method to record rising concerns and bad effects as an admission of failure or mistake, which might result in severe repercussions for the reporting individual. Because of this anxiety, medical professionals may avoid utilizing the SBAR instrument to avoid disciplinary proceedings or blame.
Chapter Three
Review of Knowledge and Practice
The Situation-Background-Assessment-Recommendation (SBAR) tool is a constructive communication technology applied in hospitals and healthcare facilities to improve the safety of the patient and better communication among healthcare professionals (Putri et al., 2021). When the SBAR tool is used for patients with a National Early Warning Score (NEWS) of five and above, it is crucial in promoting appropriate and prompt intervention. Nevertheless, the cultural and utility barriers nurses encounter in complying with the SBAR tool still need to be addressed (Adams, 2023). This review analyzes and identifies the current study about cultural and utility barriers to SBAR tool compliance regarding patients with five and above NEWS scores.
The review was searched to describe the utility and cultural barriers to Situation-Background – Assessment -Recommendation (SBAR) tool compliance for patients with a National Early Warning Score (NEWS) of 5 and above. First, the evidence concerning using the SBAR tool was reviewed (Garrett, 2021). This was followed by a search for evidence of the SBAR tool used together with the National Early Warning Score.
Review Strategy
The review evaluates existing studies related to the topic for ten consecutive years and published in English. Literature concerning the utility and cultural barriers to the SBAR tool was reviewed and identified from various books, theses, and articles using electronic databases, including PubMed, Scopus, Science Direct, Google Scholar, and university research repositories. The search terminologies used for review were Situation-Background-Assessment-Recommendation (SBAR) and National Early Warning Score(NEWS) (Park, Allan, and Hill, 2019). More than 50 relevant medical, nursing and even non-medical articles were reviewed and identified.
Relevant publications dated 2019-2023 and those not within the indicated search dates were included. Publications not within the listed years included the previous studies of particular relevance, periodic trends associated with the use of the SBAR tool as research handover, regularly referenced citations about the usage of SBAR research, and the application of NEWS to prevent or lower adverse occasions and texts for statistical examinations (Park, Allan, and Hill, 2019). Research articles talking about but not related to SBAR and NEWS were eliminated from the literature review.
Review Results
Results from a review of the published research articles included utility and cultural barriers to using the SBAR tool.
Utility Barriers
Utility barriers are the practical problems which are faced by healthcare providers when using the SBAR tool. Utility barriers in using the SBAR tool vary depending on the experience of the medical professionals. If the medical professionals are well-trained in how to use the SBAR tool, the communication between members of the health professionals concerning the patient’s health condition will be unaffected (Hogan et al., 2019). Some of the utility barriers faced by health professionals include lack of training, time constraints, the availability of resources, lack of standardization, and resistance from fellow health professionals.
Cultural Barriers
Cultural barriers are healthcare professionals’ beliefs or attitudes toward using the SBAR tool. Some healthcare professionals may believe using the SBAR tool goes against their traditional beliefs or is unnecessary. Language barriers may also be a big challenge as health professionals who communicate in English as a second language may encounter challenges communicating effectively using the SBAR tool, especially if they are unfamiliar with medical terminologies (Hogan et al., 2019). Hierarchical structures also act as a barrier. Nurses may feel discriminated against and uncomfortable using the SBAR tool to communicate medical information to other medical professionals at a higher organizational hierarchy.
The SBAR Communication Tool
The SBAR is an abbreviation of Situation, Background, Assessment, and Recommendation. The situation part provides a brief overview of the patient’s surgical and medical status at the current moment. The background part briefly summarizes the patient’s medical history and surgical condition (Putri et al., 2021). Also, it highlights the information about communication isolation, communication barriers, and allergies encountered by the patient. The assessment part gives an overview of previous laboratory assessments, systemic investigations, specific investigations, and vital symptoms and signs depending on the terms such as surgical site, pain, physical activity, and prophylaxis (Shahid et al., 2022). The recommendation part demonstrates the idea of action, such as the decision to care, treatment changes, and patient discharge.
In practically using the SBAR tool, healthcare professionals should apply good assessment, critical thinking, and clinical judgment skills. The SBAR gives a standard framework as a tool for communication, although there may be differences when presenting information to healthcare units (Putri et al., 2021). The resulting differences are influenced by cultural and utility barriers and environmental factors, as they need to be measurable and easily standardized. Due to this, in 2010, WHO efforts to improve the standardized approach in presenting communication were abandoned. According to the research, the differences in the content can be corrected by introducing a way that each healthcare unit can identify its pertinent information (Shahid et al., 2022). Through this, the SBAR content may be independent depending on each healthcare unit.
The SBAR tool was started in hospitals by a response group at Kaiser Permanente in Colorado in 2002 to boost and promote patient safety. The rapid response group is a group of healthcare staff, mostly Intensive Care Unit(ICU) staff, who give attention to patients presenting with symptoms and signs of clinical deterioration outside the ICU. In this situation, the healthcare professional responding to the patient should be able to provide adequate and appropriate information and content to the rapid response group for quick management and care (Frost, 2022). The main reason for using the SBAR tool was to boost good communication between nurses and doctors.
Contentment In the Application Of SBAR Among Healthcare Professionals
Several surveys have been carried out globally to examine SBAR communication amongst healthcare professionals, hence improving patient safety. According to the research, the use of the SBAR tool was implemented in aesthetic clinics, and it was discovered that the tool significantly improved communication accuracy, hence lowering incident reports. It was reported that SBAR is efficient in promoting interdisciplinary communication and improves communication when there is patient transfer across facilities and units (Frost, 2022). The use of SBAR in a home nursing setting boosted contentment with communication between medical professionals and nurses, improving the safety of clients and care outcomes.
Perception Of The Healthcare Professionals Concerning The SBAR Tool
Healthcare professionals using the SBAR tool have provided the same descriptions of the tool in various countries. In India, research was conducted to examine the views of healthcare professionals concerning the SBAR in developed hospitals. 92% of healthcare professionals expressed contentment with the application of the SBAR tool and demonstrated the equipment as effective, and followed a logical sequence. Additionally, the tool presented enough information and saved time. A similar study in India showed that 80% of healthcare professionals described the tool as easy to understand (Putri et al., 2021). It was also indicated that relevant communication was passed among healthcare professionals.
Another study was conducted in Singapore using the SBAR tool between non-anesthetist and anesthetists. The study was done in a pediatric ICU using pre- and post-intervention to analyze recipient perception. Healthcare professionals demonstrated the SBAR tool as brief, clear, practical, relevant, and with enough information for patient management. According to a study conducted in the USA, healthcare professionals demonstrated the SBAR tool as easy to use brief, transparent means to communicate logically (Nguyen, 2021). SBAR tool enhances patient’s self-care, hence suppressing non-patient-centered practices of delivering.
Feasibility And Acceptability Of SBAR Tool Among Healthcare Professionals
Most healthcare institutions applying the SBAR tool measured its benefits against the traditional healthcare service delivery method. Some healthcare professionals concluded that the SBAR tool is more beneficial because it became easy to understand the content detailed handing over information. Various types of research have been conducted during the application phase, and nearly every finding was approvable (Nguyen, 2021). Even on some occasions, healthcare professionals requested electronic versions of SBAR instead of a sheet of paper.
According to the study, in some healthcare settings, SBAR is presented on sheets of paper; however, many researchers emphasize using an electronic version due to the rapid emergence of paperless healthcare systems globally. For example, a healthcare facility in America substituted the paper SBAR with an electronic SBAR in response to healthcare facilities’ complaints. The electronic SBAR tool was automatically provided whenever healthcare professionals imputed information concerning a certain patient. Through this, there were consistent, efficient, and quick communication methods during the presentation. Healthcare professionals could assess recent patient information from the electronic version (Coolen et al., 2020). Healthcare professionals expressed contentment with using SBAR because it was simple to use, accurate, time-saving, and enhanced patient safety.
According to the research which was done in Australia to support healthcare professionals handing over, it was noted that electron copies had errors. The electron medical data set could not accommodate all relevant information, resulting in the printing of several documents to hand over. It was indicated that for an electronic interface to be successful, it should be adaptable, easy to navigate, flexible, and contain relevant content. A similar study on using an electronic SBAR tool in giving care in a pediatric ICU indicated complete patient information documentation, improving patient safety (Coolen et al., 2020). The electronic SBAR version should replace other ways of handing over, including the bedside and verbal.
Furthermore, some researchers needed help with the use of the SBAR tool. A study conducted in a home care setting showed that healthcare professionals experienced a longer time to complete the SBAR tool. Similarly, they encountered a communication barrier due to the language barrier, which was not corrected by the SBAR tool. Other researchers indicated that healthcare professionals require sufficient education to use the SBAR tool effectively. Another challenge faced was that healthcare professionals were not using the SBAR tool because they did not like it (Falcone, 2022). Again, some healthcare professionals encountered a problem with English proficiency, and some staff noticed missing ward content on the SBAR tool. Due to this, it was indicated that applying the SBAR tool to patients with complicated medical care plans and histories is challenging, especially in critical care settings.
Chapter Three
Methodology
Introduction
This research looks at the usefulness and cultural hurdles that nurses face when it comes to SBAR instrument compliance for patients with a News score of 5 or above. A qualitative research will be conducted in the Acute Admission Unit. The research technique describes how the selected research topic was investigated (Garrett, 2021). The research design, study setting, technique, instrument, data collecting process, data analysis, reliability and validity, methodological rigor, and ethical issues are all part of the methodology.
4.2 Research Design This study
used a qualitative study design to examine the cultural and utility barriers for nurses using the Situation-Background-Assessment-Recommendation (SBAR) tool for patients in an acute admission unit with a National Early Warning Score (NEWS) of five or higher. This study approach entails administering SBAR and subsequently gathering qualitative data (Frost, 2022). The qualitative research study allows for a thorough grasp of nurses’ opinions and experiences.
4.3 Research Environment
The study was conducted at multiple hospitals’ acute admission units. Acute admission units in hospitals are specialized healthcare facilities. The acute admission unit was chosen because to its large patient capacity and the serious condition of the patients admitted, the majority of whom had a National Early Warning Score of five or higher. It accepts nursing professionals from all throughout the country for practice (Frost, 2022). This environment provides an excellent backdrop for investigating the cultural and utility obstacles to SBAR tool compliance.
4.4 Study Population
The research population was chosen through purposeful sampling. The study sample consisted of rotation nurses and registered nurses in the acute admission unit who have sufficient knowledge and understanding of patient care with a NEWS score of five or higher and are actively engaged in the handover practice as team members or team leaders (Frost, 2022). The major goal is to obtain a varied population that will capture different experiences and opinions.
4.5 Criteria for Exclusion
The following people were excluded from the study:
1. Registered nurses who have worked in the acute admission unit for less than two months.
2. Rotation nurses who have spent less than two months on the acute admission unit.
4.6 Criteria for Inclusion
The study included the following inclusion criteria:
- Registered nurses who have worked in the acute admission unit for at least two months.
- Rotation nurses who have spent at least two months on the acute admission unit.
4,7 Sample Size
Based on data saturation, the qualitative sample size in the research study was 13 (Garrett, 2021). Data saturation occurs when people do not provide fresh information to an account.
Table 2: Participant List (Source: Author’s study, 2023)
4.8 Data Collection Methodology
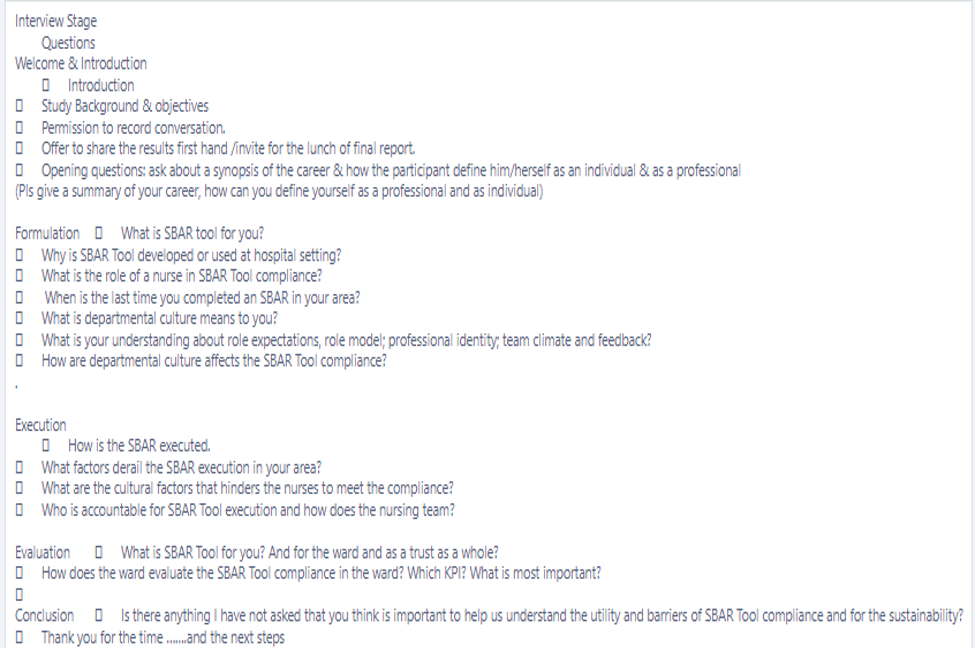
To gather data from the participants, semi-structured interviews were conducted. Rotation nurses and registered nurses who had worked in the acute admission ward for at least two months and were willing to participate were recruited. With the participant’s agreement, the interviews were audio-recorded, and an in-depth investigation of their viewpoints, perceptions, obstacles, and experiences related to SBAR tool compliance was permitted. An interview guide was supplied to guarantee consistency and uniformity throughout interviews while also providing for freedom in exploring emergent topics (Garrett, 2021). Above all, the interviews were done in a relaxed and confidential setting to encourage candid and open feedback. Questions for the interview stage were supplied.
4.9 Data Evaluation
The acquired material was analyzed using thematic content analysis. Thematic content analysis is a method that uses an objective descriptive measure to analyze a phenomena. All interviews were transcribed word for word, and the text was then colored coded to discover common themes and patterns. An comprehensive collection of codes was developed using open coding (Hogan et al., 2019). Through data immersion and ongoing comparison, the codes were then categorized into subthemes, primary themes, and classes based on their differences and similarities (Hogan et al., 2019). To facilitate data management and organizing, qualitative analysis software such as NVivo was employed.
4.10 Rigor in Methodology
In qualitative research, methodological rigor guarantees that the study is carried out rigorously following authorized reasonable interpretation and criteria. The status of qualitative research is referred to as the research’s reliability. The study’s credibility varies according on the degree of independence from biases discovered in the research and the degree to which teachers adhere to the technique used to lower levels of business. The study suggests four primary criteria to establish the framework for evaluating the quality of the qualitative research study (Park, Allan, and Hill, 2019). Transferability, confirmability, dependability, and believability are the four requirements.
The truth value or believability of the study is characterized as the research’s credibility. This relates to the degree to which the researcher is held accountable for adhering to the participants’ viewpoints, experiences, and perceptions. It involves arrangements that promote the participant’s proximity to the researcher. It also includes safeguards to prevent the researcher from influencing how the participant’s opinions and experiences are documented. To ensure the credibility of the study, the selected participants had a minimum qualification of a diploma in nursing, allowing them to better comprehend patient evaluation (Park, Allan, and Hill, 2019). To guarantee credibility, qualitative data were acquired using semi-structured interviews, and interview questions were taken from a prior research and assessed by supervisors.
4.11 Moral Consideration
The School of Nursing letter was used to get ethical permission from the Institutional Review Board (IRB) of the healthcare institution that owns the acute admission unit. All persons who participated provided informed permission while maintaining their secrecy and anonymity. Participants might withdraw from the study at any time without penalty. To guarantee anonymity and confidentiality, the names of the participants were not revealed in the research (Shahid et al., 2022). Several safeguards were put in place to protect the confidentiality and privacy of the obtained data. It was guaranteed that acquired data was encrypted and securely stored.
Chapter Five
Results
Introduction
This chapter discusses the study’s representation, including qualitative analysis. Thematic content analysis was used to assess the qualitative data. Subthemes and themes were created as soon as input was noticed and classified.
5.2 Qualitative Results
5.2.1 Participants
During the research study, 13 nurses from acute admission units were questioned. The interview was done to gather perspectives on cultural and utilitarian obstacles to SBAR tool compliance for patients with a National Early Warning Score of five or above. The total number of female nurses who participated in this exercise was 10, whereas the total number of male nurses who participated in this activity was 3.
The gender distribution shows that the majority of participants were female nurses, with just a few male nurses present. According to the list of participants, women made up 80% of the entire sample size. The higher proportion of female nurses in the research study may be utilized to demonstrate the general gender composition in the different acute admission units or the nursing profession as a whole.
The gender distribution of research participants is critical to examine throughout study analysis and conclusions. Female nurses’ opinions, experiences, and perceptions may provide important insights into the cultural and utilitarian obstacles to SBAR tool compliance. However, it is critical to recognize the gender-related elements that may influence their perceptions.
5.3 Gathering participant feedback
Face-to-face interviews with participants and mobile phone conversation were used to collect feedback. The interview was conducted after the introduction of the SBAR tool. Throughout the research, an interview guide was supplied to guarantee proper flow of replies. The interview outline included 12 core questions, including: What is the SBAR tool for you? Why was the SBAR tool created or is it utilized in a medical setting? What is a nurse’s role in SBAR tool compliance? When was the last time an SBAR in your region was completed? What does the term “departmental culture” imply to you? What do you think about when it comes to job expectations, role models, professional identity, team atmosphere, and feedback? What effect does departmental culture have on SBAR tool compliance? How is the SBAR carried out? What circumstances cause you to abandon the SBAR tool? How does the Ward assess the Ward’s SBAR tool compliance? Which KPI should I use? What matters the most?
5.3.1 SBAR Definition
This interview question encouraged participants to define SBAR based on their knowledge. The findings revealed that all participants knew what SBAR meant. The SBAR tool, according to its broad definition, is a structured communication framework used in healthcare systems to communicate patient information. The SBAR components were emphasized by the 13 participants as Situation-Background-Assessment-Recommendation.
5.3.2 Justification for SBAR Development and Use in Hospitals
Nurses recognized designing and using the SBAR tool to improve patient safety and communication efficiency. SBAR has enhanced patient safety and communication among healthcare personnel, according to eight nurses. SBAR compliance was cited as a hurdle by five of the nurses. Utility and cultural constraints have been identified as impeding SBAR tool effectiveness.
5.3.3 The Nurse’s Role in SBAR Tool Compliance
Participants emphasized a nurse’s role as a facilitator and active user of the SBAR tool. According to the participants, nurses are accountable for appropriately analyzing SBAR forms and encouraging their usage among healthcare professionals.
5.3.4 When was the last time you finished SBAR?
The responses of the individuals varied. Six participants reported that they had just finished SBAR, and five participants stated that it had been a while since they had used SBAR. Two participants said that they had yet to had the chance to utilize the SBAR without help.
5.3.5 The Meaning of Departmental Culture
In general, the participants knew what departmental culture meant. Nine individuals completely comprehended the message, whereas four had a hint but did not entirely get it. Departmental culture, according to their definition, is the collective norms, beliefs, behaviors, and values transmitted among medical practitioners in their specialized units. According to the participants, culture influences the work atmosphere, overall attitude to patient safety, and communication dynamics.
5.3.6 Becoming acquainted with position requirements, role models, personal identity, team atmosphere, and feedback
The importance of role expectations was acknowledged by the participants. Each participant discussed their contributions and roles in the SBAR process. The need of having role models who can successfully explain the usage of SBAR was noted by the participants. Feedback, professional identity, and team atmosphere are all important in creating an open and supportive workplace for SBAR.
5.3.7 Departmental culture and SBAR tool compliance
Participants highlighted a variety of cultural reasons, including hierarchy, fear of retaliation, a lack of interdisciplinary teamwork, and communication norms. All of the aforementioned criteria were identified as impediments to SBAR compliance. Participants underlined that fostering a culture of shared decision-making, psychological safety, and open communication had a beneficial impact on SBAR tool utilization.
5.3.8 SBAR Implementation
The execution of the SBAR tool was described by nurses who participated in the interview as a procedure in which nurses gather important patient information, arrange it into the SBAR format, and transmit it to other medical practitioners during handover.
5.3.9 SBAR Execution Derailment
One of the reasons cited by participants as impeding SBAR tool implementation is a lack of SBAR tool education, awareness, and time restrictions. The nurses also emphasized the difficulties that many patient cases posed upon handover.
5.3.10 Cultural variables that impede nurses’ compliance
Every participant highlighted a cultural problem impeding nurses’ use of the SBAR instrument. Communication norms, hierarchical hierarchies, fear, blame, and restricted interdisciplinary association are among the cultural elements cited. Fear, guilt, and hierarchical systems were identified as the most important cultural influences by 9 individuals. In contrast, four people identified communication norms as the most important cultural aspect.
Accountability for SBAR Tool Implementation
Participants said that all medical practitioners, including nurses, are liable for SBAR implementation. One of the nurses stressed the need of collaborative cooperation, particularly in situations when nurses play a critical role in efficiently relaying SBAR tool information to other medical professionals.
5.3.12 The Ward SBAR tool
The panelists stressed that SBAR’s job in a ward is to improve patient safety. Only 8 participants said that SBAR is a necessary tool for their Ward. SBAR, according to three participants, is critical for the whole hospital system and individual Wards. In contrast, two individuals said that SBAR is beneficial to them personally and in their Wards. Each participant mentioned the use and importance of SBAR in their Ward.
Chapter Six
Discussion
Introduction
This part describes the general discussion of the research study’s findings. The primary purpose of this research study is to examine the utility and cultural barriers for nurses in SBAR tool compliance. A qualitative method was used to collect the data for the research study. The qualitative data were collected using structured interviews, observations, and document analysis. The comprehensive data collected were analyzed using qualitative analysis and findings discussed in this part regarding the relevant research.
Perception of nurses on the use of the SBAR tool
Qualitative results indicated that the participants viewed the SBAR tool as an accurate, simple, concise, and effective tool for communication. The results revealed that all participants had come across the SBAR tool. They confirmed that it provides accurate and brief information, which boosts patient safety and enhances communication among healthcare professionals. The results concerning the use of the SBAR tool were consistent with other studies that analyzed the use of the SBAR tool. According to the study, one of the scientists described the SBAR tool as easy and straightforward to apply in communication among healthcare professionals. In another study, nurses emphasized the SBAR tool as highly efficient, organized, improved, and followed a logical sequence.
Nurses’ concern with the SBAR Tool.
Some nurses in this research study mentioned concerns about the SBAR tool. They expressed the weaknesses of the SBAR tool in various forms. Five participants mentioned that barriers, including cultural and utility barriers, hindered the SBAR tool. The kind of barriers identified by the 5 participants were unique to each other. The barriers included utility barriers and cultural barriers.
Utility barriers
Utility barriers are the practical problems which are faced by healthcare providers when using the SBAR tool. Utility barriers in using the SBAR tool vary depending on the experience of the medical professionals. If the medical professionals are well-trained in how to use the SBAR tool, the communication between members of the health professionals concerning the patient’s health condition will be unaffected (Hogan et al., 2019). Some of the utility barriers faced by health professionals include lack of training, time constraints, the availability of resources, lack of standardization, and resistance from fellow health professionals.
Cultural barriers
Cultural barriers are healthcare professionals’ beliefs or attitudes toward using the SBAR tool. Some healthcare professionals may believe using the SBAR tool goes against their traditional beliefs or is unnecessary. Language barriers may also be a big challenge as health professionals who communicate in English as a second language may encounter challenges communicating effectively using the SBAR tool, especially if they are unfamiliar with medical terminologies (Hogan et al., 2019). Hierarchical structures also act as a barrier. Nurses may feel discriminated against and uncomfortable using the SBAR tool to communicate medical information to other medical professionals at a higher organizational hierarchy.
Feasibility and Acceptability of Implementing SBAR Tool
The qualitative finding indicated that most participants revealed that using SBAR, more detailed information is communicated quickly rather than through the verbal report, which is delivered from memory. Furthermore, participants emphasized that urgent and vital patient information was handed over by use of the SBAR tool. Most of the participants who took part in the interview mentioned that SBAR covers a broad aspect of patient care and safety compared to the current ways of reaching all patient systems. This finding is similar to some of the research studies conducted by other researchers.
According to Nguyen (2021), most healthcare institutions applying the SBAR tool measured its benefits against the traditional healthcare service delivery method. Some healthcare professionals concluded that the SBAR tool is more beneficial because it became easy to understand the content detailed handing over information. Various types of research have been conducted during the application phase, and nearly every finding was approvable (Nguyen, 2021). Even on some occasions, healthcare professionals requested electronic versions of SBAR instead of a sheet of paper.
According to the study, in some healthcare settings, SBAR is presented on sheets of paper; however, many researchers emphasize using an electronic version due to the rapid emergence of paperless healthcare systems globally. For example, a healthcare facility in America substituted the paper SBAR with an electronic SBAR in response to healthcare facilities’ complaints. The electronic SBAR tool was automatically provided whenever healthcare professionals imputed information concerning a particular patient. Through this, there were consistent, efficient, and quick communication methods during the presentation. Healthcare professionals could assess recent patient information from the electronic version (Coolen et al., 2020). Healthcare professionals expressed contentment with using SBAR because it was simple to use, accurate, time-saving, and enhanced patient safety.
Contentment with the SBAR among the nurses
Qualitatively, the SBAR tool is mentioned as an effective tool that boosted handing over. The research results indicate that the participants were contented with SBAR as a communication tool rather than the traditional means of communication among healthcare professionals. This study resonates with findings that uphold that SBAR boosts communication among physicians, nurses, and doctors.
Several surveys have been carried out globally to examine SBAR communication amongst healthcare professionals, hence improving patient safety. According to the research, the use of the SBAR tool was implemented in aesthetic clinics, and it was discovered that the tool significantly improved communication accuracy, hence lowering incident reports. It was reported that SBAR is efficient in promoting interdisciplinary communication and improves communication when there is patient transfer across facilities and units (Frost, 2022). The use of SBAR in a home nursing setting boosted contentment with communication between medical professionals and nurses, improving the safety of clients and care outcomes.
Chapter Seven
Conclusions and Recommendations
Conclusion
This research investigation identified cultural and utilitarian issues that impede SBAR compliance in acute admission units. These elements have an impact on healthcare professional communication and patient safety. The SBAR was characterized by participants as a basic, accurate, brief, well-structured, effective, and speedy communication tool. Participants, however, reported that cultural and utilitarian hurdles impact its efficacy and compatibility. The acceptability and practicality of the SBAR were assessed qualitatively by asking nurses about their SBAR experiences and viewpoints. 75% of nurses supported utilizing the SBAR tool in hospitals because it is practical, accurate, straightforward, and simpler to use, improving the patient’s systemic evaluation. They also discussed various cultural and utility challenges to SBAR tool compliance and how to overcome them. Nurses were pleased with how the SBAR gadget made passing over easier than the previous way. The SBAR is widely acknowledged, but the obstacles to its implementation must be overcome.
Handing over communication may be done interdepartmentally, intradepartmentally, and on a referral basis to other healthcare institutions. Inadequate information or miscommunication during handover can jeopardize patient safety by exposing the patient to unfavorable outcomes and errors, such as delayed patient treatment, medication errors, increased hospital-obtained infections, increased hospital bills, avoidable re-admissions, or death. Misinformation or insufficient communication by healthcare professionals or nurses may result in real or prospective damage to the patient. According to various research, the handover procedure for nurses is generally unstructured, error-prone, and informal.
Handing over communication may be done interdepartmentally, intradepartmentally, and on a referral basis to other healthcare institutions. Inadequate information or miscommunication during handover can jeopardize patient safety by exposing the patient to unfavorable outcomes and errors, such as delayed patient treatment, medication errors, increased hospital-obtained infections, increased hospital bills, avoidable re-admissions, or death. Misinformation or insufficient communication by healthcare professionals or nurses may result in real or prospective damage to the patient.
Effective communication among healthcare personnel is required for favorable healthcare outcomes, patient safety, and high-quality treatment. In the acute admission unit, where patients with complicated medical issues are mostly admitted, effective and clear communication is crucial. The Situation-Background-Assessment-Recommendation (SBAR) tool has been proposed as a useful framework for minimizing mistakes and increasing communication in healthcare.
7.2 Recommendations
Based on the study findings, the following is advised to nurses and other healthcare workers working in hospitals.
The research study suggests that hospitals overcome cultural and utility hurdles to SBAR compliance in a variety of methods.
The research study underlines the need of SBAR adoption by Ward nurses in order to enhance handover practice.
It is also suggested that nurse managers guarantee that electronic SBAR copies are accessible in order to fulfill the hospital’s criteria.
The research suggests that healthcare institutions adjust their patient safety policies to incorporate SBAR as well.
Chapter Eight
Strength and Limitations
Strengths
The research findings and outcomes of this study are applicable to nursing policy, medical nursing policy, education, future research investigations, and management.
8.2 Limitations
One of the study’s drawbacks is that it was done in a hospital, therefore findings and conclusions may need to be adjusted and an actual picture of the usage of the SBAR instrument provided. It should be noted that the sample size of nurses was 13. Because of the tiny sample size, the data gathered may only reflect a subset of the nursing population. As a consequence, the findings and conclusions can only be utilized to generalize the outcomes in a few acute admission facilities.
Chapter Nine
Ethical issues
The School of Nursing letter was used to get ethical permission from the Institutional Review Board (IRB) of the healthcare institution that owns the acute admission unit. All persons who participated provided informed permission while maintaining their secrecy and anonymity. Participants might withdraw from the study at any time without penalty. To protect anonymity and confidentiality, the names of the participants were not revealed in the research. Several safeguards were put in place to protect the confidentiality and privacy of the obtained data. It was guaranteed that acquired data was encrypted and securely stored.
Chapter Ten
Reflection
Undertaking the research study on the cultural and utility obstacles for nurses accessing Situation, Background, Assessment, and Recommendation tools for patients with a National Early Score of 5 and higher in the acute admission units has been an eye-opening experience. Throughout the research study process, some key thoughts and insights have surfaced.
The need of excellent communication in hospitals has been reinforced as a fundamental understanding. The SBAR tool, a structured communication tool in hospitals, has the potential to enhance patient safety and quality of treatment. Nonetheless, this research study has revealed cultural limitations that persist in hospitals. These cultural hurdles impede the SBAR tool’s deployment and uptake. Fear of being held accountable, the hierarchical character of hospitals, and communication norms have all been identified as variables influencing SBAR tool compliance.
Reference List
Adams, J.R., 2023. Management of Sepsis with the Quick Sequential Organ Failure Assessment (Doctoral dissertation, Grand Canyon University).
Coolen, E., Engbers, R., Draaisma, J., Heinen, M. and Fluit, C., 2020. The use of SBAR as a structured communication tool in the pediatric non-acute care setting: bridge or barrier for interprofessional collaboration? Journal of interprofessional care, pp.1-10.
Falcone, M.L., 2022. Factor Structure and Construct Validity of a Hospital Survey on Patient Safety Culture Survey Using Exploratory Factor Analysis (Doctoral dissertation, University of Missouri-Saint Louis).
Frost, E.A., 2022. Factors and Barriers Preventing the Proper Use of the Modified Early Warning Score on Medical-Surgical Units (Doctoral dissertation, McKendree University).
Garrett, S.L., 2021. Implementation of the National Early Warning Score in a Military Hospital.
Hogan, H., Hutchings, A., Wulff, J., Carver, C., Holdsworth, E., Welch, J., Harrison, D. and Black, N., 2019. Interventions to reduce mortality from in-hospital cardiac arrest: a mixed-methods study. Health Services and Delivery Research, 7(2), pp.1-110.
Nguyen, T.D., 2021. Effectiveness of sbar communication tool on patient safety: an integrative review. Tạp chí Khoa học Điều dưỡng, 4(1), pp.147-154.
Park, L., Allan, J. and Hill, B., 2019. Data gathering and patient monitoring. Learning to care: the nursing associate. Edinburgh: Elsevier, pp.223-236.
Putri, I.A., Supranoto, Y.T.N., Nurrahim, H. and Erisadana, R.N., 2021. The Role of SBAR Communication Tools Implementation for Clinical Handover Among Medical Personnel in Emergency Department: A Systematic Review and Meta-analysis of Hospital Setting Studies. Journal of Asian Medical Student Association, 9(1), pp.12-13.
Shahid, S., Thabane, L., Marrin, M., Schattauer, K., Silenzi, L., Borhan, S., Singh, B., Thomas, C. and Thomas, S., 2022. Evaluation of a modified SBAR report to physician tool to standardize communication on neonatal transport. American Journal of Perinatology, 39(02), pp.216-224.
Coolen, E., Engbers, R., Draaisma, J., Heinen, M. and Fluit, C., 2020. The use of SBAR as a structured communication tool in the pediatric non-acute care setting: bridge or barrier for interprofessional collaboration? Journal of interprofessional care, pp.1-10.
Uhm, J.Y., Ko, Y. and Kim, S., 2019. Implementation of an SBAR communication program based on experiential learning theory in a pediatric nursing practicum: A quasi-experimental study. Nurse education today, 80, pp.78-84.
Leonard, C. and Zomorodi, M., 2019. Bringing the R back to SBAR: a focused heart failure SBAR tool. Home Health Care Management & Practice, 31(3), pp.179-185.
Shahid, S., Thabane, L., Marrin, M., Schattauer, K., Silenzi, L., Borhan, S., Singh, B., Thomas, C. and Thomas, S., 2022. Evaluation of a modified SBAR report to physician tool to standardize communication on neonatal transport. American Journal of Perinatology, 39(02), pp.216-224.
Jean-Baptiste, D.M., Wassef, M., Bolyai, S.S. and Jenerette, C., 2022. Individuals with Sickle Cell Disease Using SBAR as a Communication Tool: A Pilot Study. International Journal of Environmental Research and Public Health, 19(21), p.13817.
Kay, S., Unroe, K.T., Lieb, K.M., Kaehr, E.W., Blackburn, J., Stump, T.E., Evans, R., Klepfer, S. and Carnahan, J.L., 2023. Improving Communication in Nursing Homes Using Plan-Do-Study-Act Cycles of an SBAR Training Program. Journal of Applied Gerontology, 42(2), pp.194-204.
Rehm, C., Zoller, R., Schenk, A., Müller, N., Strassberger-Nerschbach, N., Zenker, S. and Schindler, E., 2021. Evaluation of a paper-based checklist versus an electronic handover tool based on the situation background assessment recommendation (SBAR) concept in patients after surgery for congenital heart disease. Journal of Clinical Medicine, 10(24), p.5724.
Carolyn Jurns, D.N.P., 2019. Using SBAR to communicate with policymakers. Online Journal of Issues in Nursing, 24(1), pp.1-7.
Stevens, N., McNiesh, S. and Goyal, D., 2020. Utilizing an SBAR workshop with baccalaureate nursing students to improve communication skills. Nursing Education Perspectives, 41(2), pp.117-118.
Lo, L., Rotteau, L. and Shojania, K., 2021. Can SBAR be implemented with high fidelity, and does it improve communication between healthcare workers? A systematic review. BMJ open, 11(12), p.e055247.
Jeong, J.H. and Kim, E.J., 2020. Development and evaluation of an SBAR-based fall simulation program for nursing students. Asian Nursing Research, 14(2), pp.114-121.
Brust-Sisti, L.A., Sturgill, M. and Volino, L.R., 2019. Situation, background, assessment, recommendation (SBAR) technique education enhances pharmacy student communication ability and confidence. Currents in Pharmacy Teaching and Learning, 11(4), pp.409-416.
Ghonem, N.M.E.S. and El-Husany, W.A., 2023. SBAR Shift Report Training Program and its Effect on Nurses’ Knowledge and Practice and Their Perception of Shift Handoff Communication. SAGE Open Nursing, 9, p.23779608231159340.
Adam, M.H., Ali, H.A., Koko, A., Ibrahim, M.F., Omar, R.S., Mahmoud, D.S., Mohammed, S.O.A., Ahmed, R.A., Habib, K.R., Ali, D.Y. and Adam, M.H.M., 2022. The Use of the Situation, Background, Assessment, and Recommendation (SBAR) Form as a Tool for Handoff Communication in the Pediatrics Department in a Sudanese Teaching Hospital. Cureus, 14(11).
Davis, B.P., Mitchell, S.A., Weston, J., Dragon, C., Luthra, M., Kim, J., Stoddard, H. and Ander, D., 2023. Situation, Background, Assessment, Recommendation (SBAR) Education for Health Care Students: Assessment of a Training Program. MedEdPORTAL, 19, p.11293.
Tschetter, M.M., 2020. Implementation of SBAR tool in a Rural Hospital.
Thomas, M., 2023. SBAR for Nursing Students to Communicate Confidently (Doctoral dissertation, Regis College).
Mahmoud, R., 2022. Using the SBAR Report Tool for Bedside Shift Reporting to Reduce Medication Errors (Doctoral dissertation, Grand Canyon University).
Abdelwahid, A.E. and Attia, N.M., 2020. Effect of SBAR training program on baccalaureate nursing students’ self-confidence in shift reporting. International Journal of Research in Nursing, 11(1), pp.1-9.
Rose-Park, D., 2022. Educating Nurses on SBAR Tool Implementation for End-of-Shift Reporting (Doctoral dissertation, Walden University).
Esposito, M.R., 2022. CN54 The implementation of NEWS2 Score in oncology patients and nursing handover with SBAR method: A pilot study. Annals of Oncology, 33, p.S1369.
Ruhomauly, Z., Betts, K., Jayne-Coupe, K., Karanfilian, L., Szekely, M., Relwani, A., McCay, J. and Jaffry, Z., 2019. Improving the quality of handover: Implementing SBAR. Future Healthc J, 6(Suppl 2), pp.54-54.
Salem, M., 2019. An Educational Intervention to Improve the Caregivers’ Understanding of the SBAR Tool Used for Patient Handover during Hospital Transfer Processes. Adv Practice Nurs, 4(157), p.2.
Appendices
Appendix A
 write
write