Abstract
Dementia has been portrayed as a major challenge among the disadvantaged aging people in the United Kingdom, particularly in England, the largest country in the region. As a result, much emphasis has been embraced by the England government and its health ministry to combat the challenges. Several services have been made available to the groups despite the research showing the effectiveness of the services to be wanting. Even though the services are entailed at supporting the groups and individuals with dementia, some have at some point proved less successful as projected. The diseases have been associated with several risk factors, which include physical inactivity, obesity, smoking, depression, low social contact, and diabetes, among other factors. Different methods have been used to come out with the evidence, including accumulating several available research studies. While not all the services were effective, the fewer effective ones were recommended for the persons with dementia to keep socially, physically, and cognitively active in later life and midlife. Providing family care interventions with long-lasting effects on anxiety and depression symptoms was recommended as they are cost-effective, increase the quality of care, and save money.
Introduction
Over the past years, the World Health Organization (WHO), in conjunction with other countries’ ministries of health, has realized the increased health concerns among people of different ages. The move to uncover the increased health concerns has been achieved through research that has been conducted. As a result, there has been a list of diseases, with dementia being one of the prioritized diseases (Bamford et al., 2021, p.411). Even though it may seem that dementia is not much severe to human health, there are its related issues that may need much care; otherwise, it could be a threatening disease to human health. While different authors may define the disease differently, the definition, according to the National Health Service (NHS) of England, is that it entails a group of related symptoms or a syndrome that is associated with the declining functioning of the human brain (Chester et al., 2019, p.63). The human brain consists of billions of nerve cells that send signals throughout the body. It works by sending messages through the spins and across the vast network of nerves contained in the body to distance extremities. Other messages are kept within the brain. As people age, they get exposed to various health issues, with dementia being one of the health issues. These diseases affect people’s health by damaging the brain cells, which are key in relaying messages in the form of signals from the brain to other body nerves (Bamford et al., 2021, p.501). As the cells become damaged, it means that the ability of the brain nerves to communicate and transfer signals to different nerves has been impacted. As a result, feelings, behavior, and thinking are affected by the brain’s inability to communicate normally due to memory loss. While the disease is common to people of every age, it is considered most common among aging people.
According to Clarkson et al. (2021, p.99), the disadvantaged groups in England, such as migrants, refugees, asylum seekers, homeless people, and gypsies, are among the most vulnerable people to dementia disease. As these populations age, their brain functioning and relaying signal messages through the nerves is lowered greatly. As a result, there is a need to have much concern in these populations to reduce the disease. As the England government and the ministry of health focus most effective services to meet the needs of the disadvantaged people in the region, it needs first to determine the definition of the diseases and the various types in which the disease exists. Smith et al. (2018, p.161) show the most common types of dementia to be frontotemporal dementia, Alzheimer’s disease, Lewy body dementia, vascular dementia, and mixed dementia. Even though those mentioned above are considered the most common and non-reversible type of dementia, other disorders exist attached to dementia. These include Huntington’s disease, Parkinson’s disease, traumatic brain injury (TBI), and Creutzfeldt-Jakob disease. Some conditions of dementia that are reversible with treatment include endocrine abnormalities and metabolic problems, infections and immune disorders, nutrition deficiencies, brain tumors, medication side effects, and subdural hematomas (Cunningham et al., 2020, p.2801). With the disease covering a wide range of disorders, there has been the need for England’s ministry of health and government to establish the best services that can help reduce the increasing rate of the disease while also caring for the disadvantaged people affected by the disease.
Some of the prominent services that the NHS of England have offered to people with dementia include physiotherapy, foot care (podiatry), hearing care (audiology), speech and language therapy, eye tests (optometry), and support from Older People’s Mental Health team (Davies et al., 2020, p.1659). The physiotherapy services have been provided to help restore the function and movement of the people who have been affected by disability, illness, and injury. These have been enlisted as some of the factors behind dementia. Thus, to ensure they do not severely impact people’s movement and function, the NHS embraced these physiotherapy services. As the services help prevent further injuries, they also improve physical activity (Delgado et al., 2021, p.464). Some of the conditions that may require physiotherapy include joints, bones, and soft tissue such as neck pain and back pain; brain and nervous systems like movement probe caused by multiple sclerosis (MS), Parkinson’s disease, and stroke; heart and circulation like rehabilitation for heart attack; and breathing and lungs like cystic fibrosis and COPD (Wittenberg et al., 2020, p.266). These services are provided by specially trained practitioners called physiotherapists. They work in medicine and settings, such as some sports charities, clubs, teams, and workplaces, some GP surgeries, community health centers or clinics, and hospitals. Working as part of a multidisciplinary team, the physiotherapists do not focus on an individual aspect of illness or injury, but they consider the body as a whole (Burgon et al., 2019, p.259). Some of the approaches that the physiotherapist uses in providing the services to dementia people include education and guidance where they provide influential advice that can impact one’s daily life and prevent injuries. Another approach is tailored exercise, movement, and physical activity advice which are recommended to help improve morbidity and general health and strengthen specific body parts (Chester et al., 2019, p.68). Manual therapy is also used to encourage better body movement, and also therapist uses their hands to relieve stiffness and pain.
The hearing test is a free service in England and is provided to dementia people by the audiologist (hearing specialist). The services are made available at opticians and in large pharmacies. For foot care (podiatry), the services offered aimed to enhance exercises by dealing with common foot problems. According to Heger et al. (2019, p.21), the services are offered to healthcare professionals who have been trained to treat and diagnose abnormal conditions of the lower limbs and feet. They help keep people active and mobile, treat infections, and relieve pain. The National Institute for Health and Care Excellence (NICE) guidance advocates for the footcare services related to rheumatoid arthritis, peripheral arterial disease, diabetes, and other long-term conditions to be made available in NHS (Eyles et al., 2021, p.8). Besides, the NHS offers NHS continuing healthcare to support the disadvantaged population affected by dementia. This service provides free care to the disadvantaged populations for all the services they receive in their local council and at their home or in a care home. The program is considered to have been made successful through the local clinical commissioning group (CCG) funding. Even though the service is offered to dementia patients, having the disease does not mean it qualifies for the service. According to Clarkson et al. (2021, p.109), it depends on the severity and the complexity of the patient’s needs. Similar to the NHS continuing healthcare is the NHS-funded nursing care that caters to the cost of the dementia populations at nursing homes.
Services to the disadvantaged population in England and those diagnosed with dementia are not limited to charities and voluntary organizations (Chenoweth et al., 2021, p.11). For many years, these organizations have shown great support for eradicating diseases in various ways. Some have gone the extra mile in providing free tests and diagnoses to disadvantaged populations, especially those in remote and rural areas. Others have also provided funding support to the services entailed at supporting the population’s care. There is the Dementia UK which offers advice and support to the disadvantaged populations living with dementia disease through the admiral nurses, who are considered the dementia experts and registered nurses (Carey et al., 2018, p.311). Another organization is Alzheimer’s Research UK which conducts research and answers questions about dementia. It provides guidance and help to the populations hence improving the life quality of such people. The Lewy Body Society has helped in funding research for dementia, and its mission has been to raise awareness to the disadvantaged populations with dementia and offer education to both the populations and the medical professions (Carey et al., 2018, p.309). There are other services that dementia patients have been attached to. Some of the social services entailed supporting dementia persons include access to day centers, aids and adaptations, meals on wheels, laundry services, and cares to help in dressing and washing (Buckner et al., 2019, p.1241).
Generally, this research aims at assessing the effectiveness of dementia services in meeting the needs of the disadvantaged groups in England. While the national government and the NHS of England provide a wide range of dementia support to the disadvantaged populations, not all of them have proved successful (Ahmed et al., 2018, p.1283). The objectives behind the research are to determine the gaps within the health services for the people living with dementia to help in more enactment for improvements. Additionally, the research objective will be to determine the extent to which the disadvantaged groups in England are vulnerable to dementia compared to their counterparts and recommend the best approaches to the existing disparity, if any, is found.
Presentation and Evaluation of Data
The fact on the dementia diseases and the effectiveness of the services England has offered to disadvantaged groups have well been portrayed in research sources. The benefits and the effectiveness are accessible to both the qualitative and quantitative evidence. According to Wittenberg, Barraza-Araiza, and Rehill (2019, p.311), there has been evidence of the current rise in the number of people with dementia. The predictions of dementia prevalence on its future trends vary based on the underlying geographical regions and assumptions. However, there is a positive projection that the case might increase as people age. Compared to the cohort from other countries like France, and the USA, there are considerably higher age-specific incidences of dementia in England (Nguyen et al., 2021, p.15). However, there has been a low incidence of dementia in recent years due to lifestyle changes, health care, socio-economic and education. As physical activities reduce, there are increased incidences of diabetes and obesity, which are the risk factor for dementia. It is suggested that modeling the UK lifestyle might see the cases of dementia increase to 57% from 2016 to 2040 (Pujades-Rodriguez et al. p.91). Besides, models also suggest that both the number of individuals with complex care needs and independent ones are projected to increase in the future. For potentially modifiable dementia risks, a life-course model was described in a commission in 2017 (Vohra et al., 2021, p.79). The life course is essential, especially in consideration for risks such as hypertension and obesity in future midlife dementia, but blood pressure and weight fall in later life among individuals developing or with dementia, so blood pressure and lower weight might signify risk absence and illness.
Around 676000 people in England are estimated to have dementia. In the whole United Kingdom (UK), it is estimated that more than 850,000 have dementia showing England to be leading among the four UK countries (Wales, Scotland, and Northern Ireland) (Hossain, and Khan, 2020, p.1633). As the disease increases, there is also an increase in the number of carers in England, with an estimated range of 540000 carers (Ayton et al., 2021, p.194). It is reported that for every five people, three of them report having cared for dementia patients in their lifetime. This shows there are many concerns on the people with dementia in the country, prompting the government and other agencies to take appropriate and immediate action. As the need for carers increases, many people have seen themselves cutting their working hours while others leave their job completely to provide care to family members diagnosed with dementia. According to Murphy et al. (2021, p.954), among those reported to have cut their working hours range around 66000 with 50000 people having left their work to live and provide care to the dementia patients.
As Hall et al. (2018, p.9) state, there exist some dementia protection mechanisms which may involve either maintaining or increasing cognitive reserve despite neuropathological and pathology damage. The noted varying susceptibility to disease and age-related changes and those not consistently used may exhibit different description terms. As Rand et al. (2021, p.601) mention, a reserve can further be divided into a cognitive reserve, brain maintenance (lifestyle or genetics reducing pathology development and brain changes over time), and neurobiological brain reserve (such as the number of synapses and neurons at a given timepoint) as enabling adaptability preservation of everyday functioning or cognition despite brain pathology. The figure shows the brain’s possible mechanisms for enhancing cognitive reserve and reducing potential risk factors in dementia.
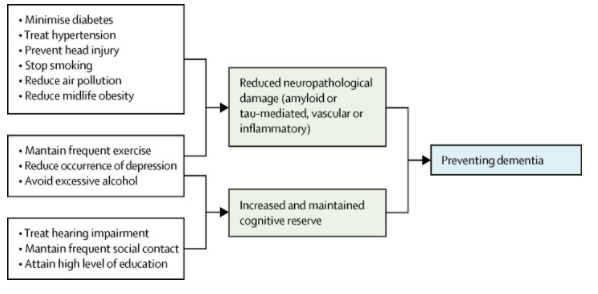
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7392084/figure/fig2/
Education and other early life factors are highly associated with impact to the people ability of cognition. Old age and midlife risk factors trigger neuropathological developments, influencing age-related cognitive decline (Burgon et al., 2019, p.288). This is consistent with the hypothesis that older women are more vulnerable to developing dementia diseases than men of the same age. This is also because older women are considered less educated than older men (Wittenberg et al., 2020, p.266). Some of cognitive mechanisms are increased connectivity in frontal and temporal brain areas. Without even cognitive impairments, there is the possibility of sustaining a higher burden of neuropathology among people with good physical health (Collins, Silarova, and Clare, 2019, p.317). The need for change for cognitive reserve might be obstructed by the drivers such as inequality, poverty, and culture. This has been a major common challenge among the disadvantaged families in England. Many of them live under poverty and exhibit a challenging life of inequality in healthcare. According to Davies‐Kershaw et al. (2018, p.1827), risk factors for dementia among disadvantaged families remain a major challenge. The table below shows the list of the risk factors exhibited din in early life (education), midlife (alcohol misuse, traumatic brain injury, hearing loss, obesity, and hypertension), and in later life (air pollution, diabetes, social isolation, physical inactivity, depression, and smoking).
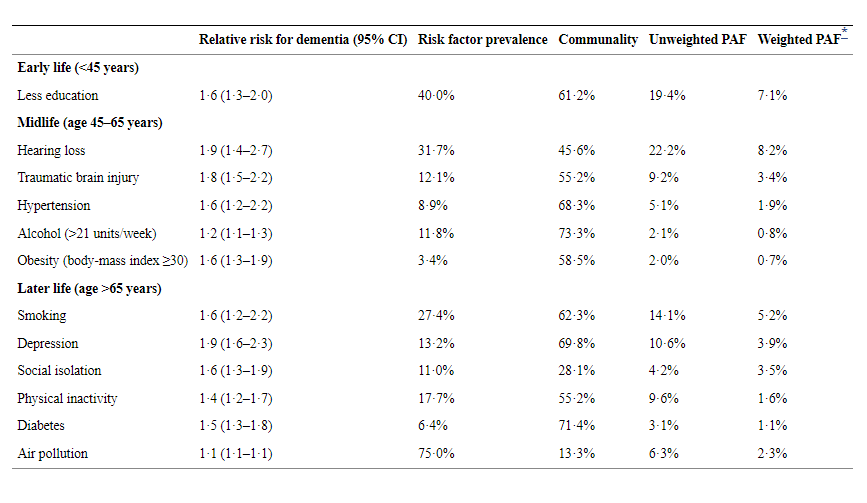
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7392084/
According to the information obtained from Quality and Outcomes Framework, England has seen a rise of 10% for the people diagnosed with cancer from the year 2008/2009 (232000 cases) to 2015/2016 (344000) (Bartlett, 2021, p.11). This presents a large rise in disease, considering that it can have a negative impact on a large population in the country. The increase was well spread, with every sector providing services to the dementia people reporting an increase with time. In 2015, two of the care providers of care homes reported an increase of 13% (22000 cases from 450 homes) and 10% (900 from cases15 homes) (Darlington et al., 2021, p.1717). Additionally, Islington in England reported a 2% for care home residents. However, the proportion of the dementia patients admitted on anti-psychotic medication among the acute hospital inpatients fell from 21% to 11% between the years 2014 to 2018, with those taking drugs reducing from 12% to 8% (Davies et al., 2020, p.1660).
The effectiveness of the support services for the dementia disease in England has not much achieved the projected goals, but it has at some point proved successful. Livingston et al. (2020, p.419) denotes that for the past years, the England government and the ministry of health have shown to embrace a positive and more dementia-friendly environment and establish senior clinical leads resulting in improved awareness of dementia diseases among staff in acute hospitals. Low consumption of anti-psychotic medications, for example, has helped reduce adverse incidents like stroke, accelerated cognitive decline, Parkinsonism, and falls. During 2014/1015, approximately 3.1% (474000) individuals were recorded to have been diagnosed with dementia (Tampubolon et al., 2015, p.1130). Since this rate was recorded, hospitals have gone an extra mile to fight the diseases through various approaches. Encouraged by financial incentives, the hospital has increased the diagnosis rates. This required the patients above 75 years and those staying three days or more and without preexisting dementia diagnosis to be assessed (Carey et al., 2018, p.299). According to Arsenault-Lapierre et al. (2021, p.722), despite the support services that were provided to reduce dementia cases, England recorded a rise from 5.5% to 7.4% in 2016/2017, which amounted to over 50,000 referrals. Between 2013 and 2014, the proportion of acute hospitals with dementia care pathways rose from 6% to 36%, as did the proportion with a senior clinical leader, increasing from 44% to 81% (Ahmed et al., 2018, p.1281). The progress on the effectiveness of the support services to the disadvantaged populations with dementia appears slow in some areas.
Staff training has been a key factor behind the improvement and effectiveness of dementia support services. For the past years, the proportion of hospitals with strategies to identify their staff and provide training on dementia prevention and treatment skills has increased from 23% to 78% (Arsenault-Lapierre et al., 2021, p.731). Those with the mandatory training requirements for all staff are approximately 5% to 59% (Heger et al., 2019, p.33). This shows great success towards eradicating the dementia disease.
To evaluate the effectiveness of the dementia support services among disadvantaged people in England, research was conducted involving 131 publications, with 13 being evaluated as low quality, 62 of the publications considered medium quality, and 56 of high quality. The evaluations were presented in a table format summarizing the quality and quantity of the literature ascertained. The types of findings included groupings under headings and sub-topic headings. The table shows the type, quality, and quantity of literature by the topic heading.
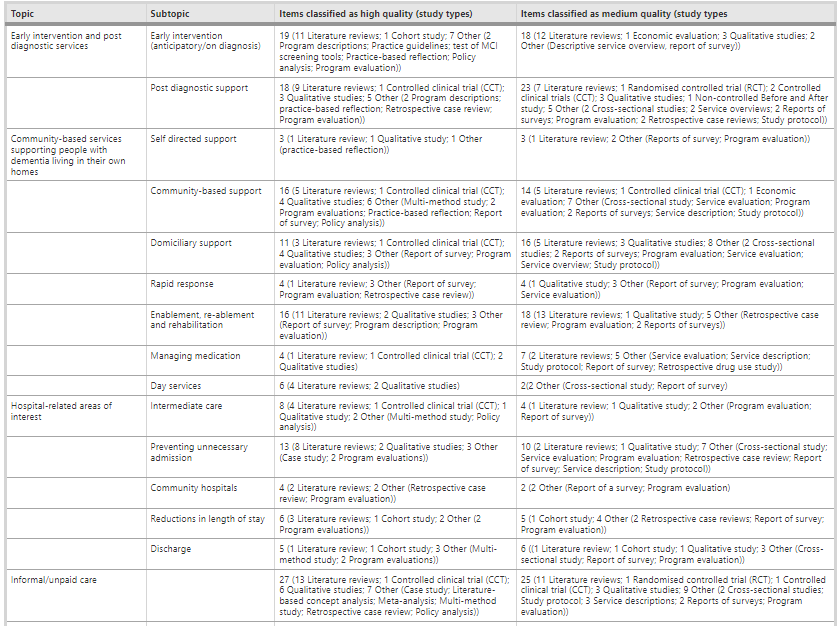
Source: https://bmcgeriatr.biomedcentral.com/articles/10.1186/s12877-015-0053-9/tables/2
As seen in the above table, the findings were presented by topics, and it was found that there is interconnectedness between the support area for dementia people, and the considerable thematic overlap evidenced this in the literature. For this reason, some sources had connections to more than one topic. Besides, recent research by Hall et al. (2018, p.7), have identified an existing gap between the actual population with a dementia diagnosis and the predicted number with dementia based on the region’s prevalence rate. Responding to this disparity, NHS England and NHS Scotland have both dedicated targets to recuperate the immediate provision of post-diagnostic support and improve or maintain dementia diagnosis rates (Bartlett, 2021, p.11). The post-diagnostic support in Scotland ought to consider the Alzheimer Scotland’s 5 Pillars model, which ensures dementia people and their families get support and information they need; maintain community connections, make timely decisions, plan for future decision making and understand and manage symptoms. In a study conducted by Mayrhofer et al. (2021, p.2438), among the three groups, Asia, Whites, and the blacks in England, it was evidenced that the black ethnic groups had higher incidence of dementia compared to the rest of the groups. According to the authors, women in this group had a stronger association than men. Besides, the Asia ethnic groups had a higher incidence of dementia than the whites. The table below depicts the incidences of dementia among the three groups.
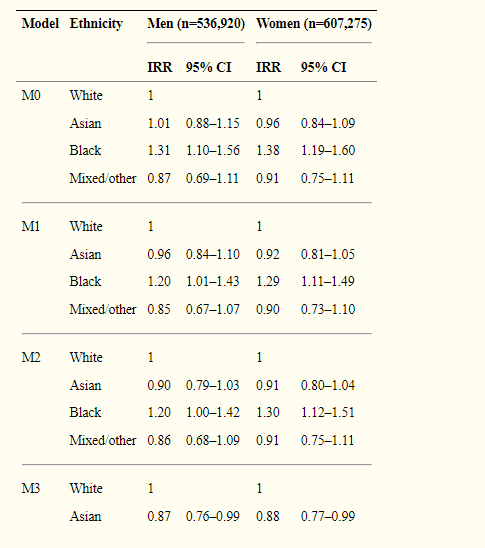
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6087031/
The post-diagnostic support for dementia individuals has been considered a more recent one, and hence there have been limited studies on the inventions. However, some reviews have indicated both the accessibility and focus as an experience of post-diagnostic support. For example, research by Wheatley et al. (2021, p.2231) showed that individuals diagnosed with frontotemporal dementia have challenges engaging and finding suitable community and home-based services as a result of lack of knowledge and understanding of frontotemporal dementia. For some years, non-pharmacological have been used for medication as an alternative intervention. Martin et al. (2021, p.109) proposed the benefits of information and communication technology to people with dementia as it compensates for disability. Cognition-focused interventions were confined to have small effects and were inconsistent on general cognitive ability. The support of paid carers such as post-diagnostic was reported to exhibit challenges. Research conducted by Weetch, O’Dwyer, and Clare (2021, p.1599) focusing on bio-medical support needs showed that England nurses, pharmacists, and doctors don’t receive adequate training on treatment drugs for aging people. Despite the UK Community Psychiatric Nurses (CPNs) reporting rehabilitation delivery to mental problems as part of their job, they claimed to have limited knowledge on aids and memory rehabilitation strategies for people with dementia (Collins, Silarova, and Clare, 2019, p.311).
Another study focused on day care services as a provision area for minority people with dementia. Despite limited recent research, many of the available ones have explored reasons for leaving day services or refusing to attend day services and questioned how such services could be of value. A study by Ayton et al. (2021, p.185) found substantial evidence among the asylum seekers and the immigrants with dementia who lived with dementia being unable to cooperate and embrace the day care opportunities. Many of these people gave several reasons behind individual perceptions of failure to enjoy the day services linked to questions about being institutionalized, losing independence, and meeting new people. The researchers suggested the possibility of undiagnosed depression among those declining the day care. Another study conducted by Hossain and Mughal (2021, p.214) concerning the day services showed that a third of refugees with dementia in England gave up within one year, and a further third dropped within four months. High physical care levels and behavioral disturbances need short-term uptake predictors of the services, resulting in questioning the value of tendering day care to individuals with behavioral disturbances (Darlington et al., 2021, p.1121). The value of day care was also questioned in a systematic review conducted. This was after a lack of reliable evidence on the adverse effects or benefits of respite on care recipients and delays in entry to residential care. The available evidence by Vohra et al. (2021, p.311) showed caregivers perceived day care benefits for themselves and their relatives, concluding on limited positive effects on carers’ burden and physical or mental health.
Community-based services supporting disadvantaged people living in England and with dementia entail those services available at the community level, such as residential respite care facilities, support for carers, and information provision. In a systematic review by Stamou et al. (2021, p.1131), the relative detriments of varying community-based support models were deemed to have very limited comparative evidence calling for rigorously evaluated models for comparison and assessment. As noted by Livingston et al. (2020, p.431) respite care lacks evidence or has little evidence that it benefits individuals diagnosed with dementia, is more cost-effective compared to other supports forms, or delays their residential care transition. However, an assisted vacation intervention evaluation for the gypsies diagnosed with dementia found lasting and immediate benefits for the carers and persons with dementia. Making information accessible to the people can help make timely decisions about accessing services and better understand local provisions. However, since people do not know where to get the services’ information from, Stanyon et al. (2021, p.151) suggested that they rely on primary care physicians or general practitioners (GP). Several reviews and studies identify lack of evidence in technology utilization in the context of intervention and living with dementia. There is limited knowledge and recognition of the role of e-health technology as an intervention in supporting people with dementia and addressing the unmet needs as perceived by dementia individual and their carers (Farina et al., 2021, p.1119). Despite the limited evidence base, it is assumed that technology-based interventions are significant in reducing carer burden, improving safety at home, and reducing the home-based care overall cost for people with dementia (Burgon et al., 2019, p.301). Currently, there is evidence emerging on the benefits of horticulture therapy and other physical and outdoor activity interventions as part of the remit for the minority groups in the UK and particularly those with dementia, although more vigorous interventions evaluation is needed. Gage et al. (2021, p.421) show joint working in support for nutrition by services for support and monitoring to have value, especially to the people with advanced dementia who need care.
Critique of the Findings and Data from The Literature
Despite the literature presenting different findings in different capacities, some critiques have trailed the findings. Some critiques have been posed on the estimation to the great challenges on true prevalence. As argued by Heward et al. (2021, p.522), it could be imprecise to distinguish mild cognitive impairments from dementia, and changes in international definitions mean the alteration to the boundary. While the influence of professional judgment can be reduced by the availability of clinical criteria, it does not disregard this source of variation. Secondly, there was an inevitable prevalence in reviewing the population survey results based on the experts’ consensus view in the past. As critiqued by Heger (2019, p.21), there might exist a big variation currently considering that the estimated number of disadvantaged populations in England and those with dementia have been reassessed in light of aging study and cognitive functioning. This finding results in the suggestion by the latest expert group that there are approximately 40,000 people with early-onset dementia and 686000 with dementia (Chenoweth et al., 2021, p.7).
The diagnosis rate between clinical commissioning groups is also reported to exhibit variations from 39% to 75%, though given the uncertainties, there needs to consider the cautions of such estimations (MacLeod et al., 2021, p.111). If this is real, then it may echo the utilization of memory assessment services and their availability created with the drive for dementia diagnosis. Despite some national surveys, the extent of waiting and provision times remains uncertain, as does their efficiency and effectiveness (Delgado et al., 2021, p.459). Little may be recognized about changes with time as attributed by the differences in the methodologies used between surveys, even though the number of asylum seekers and refugees in England attending dementia services was reported to increase by 5% from 2010 to 2017 (Nguyen et al., 2021, p.13). The mean waiting time in 2012 was 5.2 weeks, even though the recent reports on anecdotal suggest their increase. Individuals diagnosed with primary care have increased more than those referred to specialist clinics, and as a result, it becomes more complicated to interpret data on memory assessment services (Wittenberg, Barraza-Araiza, and Rehill, 2019, p.566). Despite embracing hospital care, its improvement benefits lack clear evidence. However, the recent initiatives are likely to improve care for disadvantaged people with dementia. The scope for further improvements remains equally apparent. As noted by Giebel, Morley, and Komuravelli (2021, p.331), studies in 56% of the hospital showed that personal assessment for both the immigrants and refugee care needs were not identified, and the care aspects in relation to social, emotional and mental health necessities were deprived in 42% of the hospitals.
While some researchers have not identified an increased use and provision of psycho-social therapies among the disadvantaged populations in the UK, there is growing evidence on its effectiveness in intervening with people with dementia. Lepore et al. (2021, p.109) state that individuals with mild to moderate dementia benefit from cognitive stimulation therapy and enhance their self-reported life quality. Further, long-term therapy use appears to be significantly effective and beneficial (Hall et al., 2018, p.6). Other therapies with less scientific evidence showed promise include reminiscence therapy, music therapy, cognitive behavior therapy, and cognitive rehabilitation. According to Potter et al. (2021, p.1651), medication prescriptions aimed at alleviating the symptoms of dementia have been estimated to increase 50% since 2010. Clinical benefits evidence of memantine, rivastigmine, donepezil, galantamine, and other drugs have also increased even though they are limited by the dementia severity where medications are effective, small effect sizes, short duration of trials, and unsatisfactory attention to the paid adverse effects (Carey et al., 2018, p.221).
Another systematic review by Murphy et al. (2021, p.949) found modest effects of respite care in improvement in carer’s mental and physical health than those populations diagnosed of dementia, implying limited or no evidence that it delays institutional care admission. Despite the available research on minority groups in the UK, there is very little attempt by the service providers to engage the minority communities. As highlighted by Delgado et al. (2021, p.461), there was also the feeling that the disadvantaged individuals with dementia, compared to the end-of-life care, are less consulted than carers for a group not diagnosed with dementia despite the evidence that end-of-life admission of individuals with dementia is particularly detrimental.
The mini-mental state examination has been used among people with dementia in assessing their cognitive abilities. According to Darlington et al. (2021, p.1119, the assessment entails many questions that are used to assess one’s cognitive ability. Despite the mini-mental state examination being widely used, it is posed with contradictory to the modern ethos amongst other limitations. Created by Hug and Folstein in 1975, the author claimed that the method was valid, reliable, quick, and acceptable to testers and patients (Parveen et al., 2021, p.393). However, a recent study conducted by Ayton et al. (2021, p.191) to retest the method’s validity and reliability found that the method lacked a standardized score and had too many cutoff points, too many easy times, and low reliability. As a result, the authors argued and concluded that cognitive screening assessment might not be effective when used on its own. They, however, did not acknowledge the reliability and validity parameters changed since the publishing of the test. Further, Hoe et al. (2021, p.62) found that despite using the method among the highly educated individuals, it did not yield optimal classification accuracy with a cutoff point score of 24.
Discussion
The diagnosis review’s findings for different disadvantaged groups in England suggest variable experiences accenting the essence of recognizing and addressing the needs and experience diversities. According to the post-diagnostic support, the review hints that multi-component, cognitive rehabilitation, training, stimulation, education, and other locally based interventions may be beneficial in championing for persons with dementia and the family carers (Smith et al., 2018, p.161). The literature highlights the Community Psychiatric Nurses (CPNs) as exhibiting under-utilized potentials and stresses key practitioners’ knowledge gap (Weetch, O’Dwyer, and Clare, 2021, p.1601). Overall, there is limited evidence that community-based services support the minority groups of England with dementia living in their homes, and hence more specific England research is needed to provide clear information. However, the field of support and care to dementia have identified newly emerging concerns such as the use of technology in support for dementia, use of multidisciplinary, fast response teams, and take up and use of self-directed support (Gage et al., 2021, p.422).
From the literature review, it could be suggested that the dementia support services with the best outcome are associated with services that are tailored to individual needs, flexible, responsive, and timely. However, according to Livingston et al. (2020, p.441), dementia services like community-based support are considered a rapidly changing landscape, implying the need for knowledge areas. For an instant, the shift from institutionalized and hospital-based forms of care to support is well underway, but its research in preventive services has not kept pace with the changes (Leverton et al., 2021, p.9). As persons with dementia need more support services to stay longer, the pressure on dementia services to accommodate the changing needs increases with time to promote more productive working ways, apprehend changes from the views of individuals diagnosed with the disease and their carers, and into service design. Many authors revealed the healthcare-related areas of interest need additional research. According to Sawan et al. (2021, p.3), some involve identifying and exploring what is more beneficial in delaying or preventing the dementia onset, testing, and developing more effective end-of-life care methods.
Additionally, there are limited and local positive effects on many one-off interventions, but its compelling to the evidence on the likelihood of a successful multi-component approach. The success of this one-off brings a key unanswered question on whether their success is due to the engagement vehicle they provide rather than their actual content (Collins, Silarova, and Clare, 2019, p.318). Another major issue with the ineffectiveness of the dementia services among the disadvantaged groups is informal or unpaid care which reasserts the vital role of unpaid carers and the need to have them supported to carry on with their work (Chirico et al., 2021, p.3422). Some of the issues neglected in this area include the continence and the end-of-life care, both being difficult and sensitive for addressing dementia carers at home. Besides, there is an essential issue of supporting and identifying people without informal care. This area exhibits a relative paucity of research, and it is thus important for the policy not to assume that individuals always have support from their own networks or carers are always present. A study by Heger (2019, p.17) emphasized the connection with refusal day care with the importance of ascertaining their view as unimportant.
In the review course, issues and themes connected to all or most of the areas contemplated have been identified. For instance, despite the dementia studies from social sciences and humanities having significant contributions, it was found that much of the literature was characterized by a focus upon management and their symptoms and thus adhering to a bio-medical model of dementia (Hoe et al., 2021, p.52). Some signs of change were, however, exhibited. In particular, the recommendations and study designs have growing recognition on the essence of engaging carers and people with the disease in policy, delivery, and research.
The recognition for the disadvantaged people with dementia in England has been a major concern in more recently emerging themes. For example, there is a shred of increasing research evidence concerning the challenges and needs encountered by the individuals diagnosed with the disease in rural and remote communities in the UK (Tampubolon et al., 2018, p.1129). Further, the research evidence has grown among people with different experiences of different forms of dementia. Majority of these groups have no access to service and support, and most include minority ethnic communities like Asians, black, and others (Csipke et al., 2018, p.191). Changing policy and economic landscapes, improved understanding of dementia prevalence, and demographic change are all acting as drivers for services innovation globally, and they at large influence both the extent and the pace of change. According to Mayrhofer et al. (2021, p.2439), when the evidence base exhibits some weaknesses, it may pose challenges to both the practitioners who needs guidance about evidence-based services delivery or design them to comfort people in communities with dementia, their carers, and those people responsible for reviewing such services.
Recommendations
Despite the dementia services among the disadvantaged people in England living with dementia entailed minimizing the disease and the challenges, the effectiveness of the services has remained a major concern (Rand et al., 2021, p.122). As a result, several interventions are recommended to ensure the effectiveness of the services. One of the key recommendations significant to dementia people is keeping socially, physically, and cognitively active in later life and midlife. Using hearing aids, for example, help reduce hearing loss and its related risks (Frost et al., 2021, p.1389). Further, sustained exercise in both later life and midlife decreases the risk of cardiovascular, diabetes, and obesity, reducing dementia. Even though behavior changes may not be possible to some extent, avoiding behavior associated with depression can greatly help reduce the chances of dementia (Delgado et al., 2021, p.458). It is recommended that for the support of persons with dementia, there is the need to consider holistic post-diagnostic care, which should address mental and physical health, support, and social care (Martin et al., 2021, p.171). As people battle with dementia, they might also have other illnesses that need to be considered to ensure the persons are not exposed to potentially preventable hospitalization, which might make them struggle to look after their health. Besides, some family care interventions may have long-lasting effects on anxiety and depression symptoms, are cost-effective, increase the quality of care, and might save money (Parveen et al., p.390).
The prevalence of dementia among the disadvantaged populations in England has called for the need to furnish the staff with education and training. As reported from the review, many of the staff were noted to have limited skills in attending and caring for people with dementia (Hossain, and Khan, 2020, p.1631). As a result, it has made the services’ success a challenge. The support and care providers need to be trained on outcome-focused and person-centered care for individuals with dementia. Some of the essential skills needed to attend to people with dementia include recognizing the symptoms and signs of dementia and the expected changes with the progression of the condition (Farina et al., 2021, p.1121). Staff providing support and delivering care to populations with dementia needs to be provided with mentoring and face-to-face training. Last but not least, more emphasis needs to be considered when it comes to medications. According to Carey et al. (2018, p.255), some of the medication associated with increased anticholinergic burden needs to be avoided due to cognitive impairment. People need to look for alternatives and consider minimizing the use of medicine with negative health effects (Giebel, Morley, and Komuravelli, 2021, p.501). While some of the medicine used in reducing dementia effects have been said to be good, they have negative impacts as they can result in other health problems associated with dementia disease.
Bibliography
Ahmed, S., Hughes, J., Davies, S., Stewart, K., Orrell, M., Clarkson, P., Challis, D. and HoSt‐D (Home Support in Dementia) Programme Management Group, 2018. Specialist services in early diagnosis and support for older people with dementia in England: Staff roles and service mix. International journal of geriatric psychiatry, 33(9), pp.1280-1285.
Arsenault-Lapierre, G., Henein, M., Rojas-Rozo, L., Bergman, H., Couturier, Y. and Vedel, I., 2021. Primary care clinicians’ knowledge, attitudes, and practices concerning dementia: They are willing and need support. Canadian Family Physician, 67(10), p.731.
Ayton, D.R., Gardam, M.L., Pritchard, E.K., Ruseckaite, R., Ryan, J., Robinson, S.J., Brodaty, H., Ward, S.A. and Ahern, S., 2021. Patient-Reported outcome measures to inform care of people with Dementia—A systematic scoping review. The Gerontologist, 61(5), pp.e185-e194.
Bamford, C., Wheatley, A., Brunskill, G., Booi, L., Allan, L., Banerjee, S., Harrison Dening, K., Manthorpe, J., Robinson, L. and PriDem study team, 2021. Key components of post-diagnostic support for people with dementia and their carers: A qualitative study. PloS one, 16(12), p.e0260506.
Bartlett, R., 2021. Inclusive (social) citizenship and persons with dementia. Disability & Society, pp.1-17.
Buckner, S., Darlington, N., Woodward, M., Buswell, M., Mathie, E., Arthur, A., Lafortune, L., Killett, A., Mayrhofer, A., Thurman, J. and Goodman, C., 2019. Dementia friendly communities in England: A scoping study. International Journal of Geriatric Psychiatry, 34(8), pp.1235-1243.
Burgon, C., Darby, J., Pollock, K., van der Wardt, V., Peach, T., Beck, L., Logan, P. and Harwood, R.H., 2019. Perspectives of healthcare professionals in England on falls interventions for people with dementia: a qualitative interview study. BMJ open, 9(2), pp.257-302.
Carey, I.M., Anderson, H.R., Atkinson, R.W., Beevers, S.D., Cook, D.G., Strachan, D.P., Dajnak, D., Gulliver, J. and Kelly, F.J., 2018. Are noise and air pollution related to the incidence of dementia? A cohort study in London, England. BMJ open, 8(9), p.e022404.
Chenoweth, L., Williams, A., Fry, M., Endean, E. and Liu, Z., 2021. Outcomes of person-centered care for persons with dementia in the acute care setting: A pilot study. Clinical gerontologist, pp.1-15.
Chester, H., Kampanellou, E., Davies, L., Davies, S., Giebel, C., Hughes, J., Challis, D., Clarkson, P. and HOST-D (Home Support in Dementia) Programme Management Group, 2019. Carer preferences for home support services in later stage dementia. Aging & mental health, 23(1), pp.60-68.
Chirico, I., Chattat, R., Dostálová, V., Povolná, P., Holmerová, I., de Vugt, M.E., Janssen, N., Dassen, F., Sánchez-Gómez, M.C., García-Peñalvo, F.J. and Franco-Martín, M.A., 2021. The Integration of Psychosocial Care into National Dementia Strategies across Europe: Evidence from the Skills in DEmentia Care (SiDECar) Project. International journal of environmental research and public health, 18(7), p.3422.
Clarkson, P., Challis, D., Hughes, J., Roe, B., Davies, L., Russell, I., Orrell, M., Poland, F., Jolley, D., Kapur, N. and Robinson, C., 2021. Components, impacts and costs of dementia home support: a research programme including the DESCANT RCT. Programme Grants for Applied Research, 9(6), pp.1-132.
Collins, R., Silarova, B. and Clare, L., 2019. Dementia primary prevention policies and strategies and their local implementation: A scoping review using England as a case study. Journal of Alzheimer’s Disease, 70(s1), pp.S303-S318.
Csipke, E., Moniz-Cook, E., Leung, P., Yates, L., Birt, L., Walton, H., Hogervorst, E., Mountain, G., Charlesworth, G. and Orrell, M., 2018. Promoting Independence in Dementia (PRIDE): Feasibility trial of the PRIDE social intervention for living well and independently with mild dementia.
Cunningham, N., Cowie, J., Watchman, K. and Methven, K., 2020. Understanding the training and education needs of homecare workers supporting people with dementia and cancer: A systematic review of reviews. Dementia, 19(8), pp.2780-2803.
Darlington, N., Arthur, A., Woodward, M., Buckner, S., Killett, A., Lafortune, L., Mathie, E., Mayrhofer, A., Thurman, J. and Goodman, C., 2021. A survey of the experience of living with dementia in a dementia-friendly community. Dementia, 20(5), pp.1711-1722.
Davies, N., Iliffe, S., Hopwood, J., Walker, N., Ross, J., Rait, G. and Walters, K., 2020. The key aspects of online support that older family carers of people with dementia want at the end of life: a qualitative study. Aging & mental health, 24(10), pp.1654-1661.
Davies‐Kershaw, H.R., Hackett, R.A., Cadar, D., Herbert, A., Orrell, M. and Steptoe, A., 2018. Vision impairment and risk of dementia: findings from the English Longitudinal Study of Ageing. Journal of the American Geriatrics Society, 66(9), pp.1823-1829.
Delgado, J., Jones, L., Bradley, M.C., Allan, L.M., Ballard, C., Clare, L., Fortinsky, R.H., Hughes, C.M. and Melzer, D., 2021. Potentially inappropriate prescribing in dementia, multi-morbidity and incidence of adverse health outcomes. Age and Ageing, 50(2), pp.457-464.
Eyles, E., Redaniel, M.T., Purdy, S., Tilling, K. and Ben-Shlomo, Y., 2021. Associations of GP practice characteristics with the rate of ambulatory care sensitive conditions in people living with dementia in England: an ecological analysis of routine data. BMC Health Services Research, 21(1), pp.1-10.
Farina, N., Williams, A., Clarke, K., Hughes, L.J., Thomas, S., Lowry, R.G. and Banerjee, S., 2021. Barriers, motivators and facilitators of physical activity in people with dementia and their family carers in England: dyadic interviews. Aging & mental health, 25(6), pp.1115-1124.
Frost, R., Rait, G., Aw, S., Brunskill, G., Wilcock, J., Robinson, L., Knapp, M., Hogan, N., Harrison Dening, K., Allan, L. and Manthorpe, J., 2021. Implementing post diagnostic dementia care in primary care: a mixed-methods systematic review. Aging & Mental Health, 25(8), pp.1381-1394.
Gage, H., Jones, B., Stamou, V., La Fontaine, J., Williams, P., O’Malley, M., Parkes, J., Carter, J. and Oyebode, J., 2021. Services for people with young onset dementia: The ‘Angela’project national UK survey of service use and satisfaction. International Journal of Geriatric Psychiatry, 36(3), pp.411-422.
Giebel, C., Morley, N. and Komuravelli, A., 2021. A socially prescribed community service for people living with dementia and family carers and its long‐term effects on well‐being. Health & Social Care in the Community.
Hall, A.J., Burrows, L., Lang, I.A., Endacott, R. and Goodwin, V.A., 2018. Are physiotherapists employing person-centred care for people with dementia? An exploratory qualitative study examining the experiences of people with dementia and their carers. BMC geriatrics, 18(1), pp.1-10.
Heger, I., Deckers, K., van Boxtel, M., de Vugt, M., Hajema, K., Verhey, F. and Köhler, S., 2019. Dementia awareness and risk perception in middle-aged and older individuals: baseline results of the MijnBreincoach survey on the association between lifestyle and brain health. BMC public health, 19(1), pp.1-37.
Heward, M., Board, M., Spriggs, A., Emerson, L. and Murphy, J., 2021. Impact of education intervention on trainer dementia knowledge and confidence to utilise innovative training approaches: A national pre-test–post-test survey. Nurse Education Today, 97, p.104-694.
Hoe, J., Ledgerd, R., Toot, S. and Orrell, M., 2021. Crisis and Assessment of Need in Dementia. Camberwell Assessment of Need for the Elderly: CANE, p.62.
Hossain, M.Z. and Khan, H.T., 2020. Barriers to access and ways to improve dementia services for a minority ethnic group in England. Journal of evaluation in clinical practice, 26(6), pp.1629-1637.
Hossain, M.Z. and Mughal, F., 2021. Dementia and revivalist Islam: New perspectives to understanding dementia and tackling stigma. Journal of Evaluation in Clinical Practice, 27(2), pp.213-217.
Lepore, M., Edvardsson, D., Meyer, J. and Igarashi, A., 2021. How long-term care quality assurance measures address dementia in Australia, England, Japan, and the United States. Aging and Health Research, 1(2), p.100-113.
Leverton, M., Burton, A., Beresford-Dent, J., Rapaport, P., Manthorpe, J., Azocar, I., Giebel, C., Lord, K. and Cooper, C., 2021. Supporting independence at home for people living with dementia: A qualitative ethnographic study of homecare. Social psychiatry and psychiatric epidemiology, pp.1-14.
Livingston, G., Huntley, J., Sommerlad, A., Ames, D., Ballard, C., Banerjee, S., Brayne, C., Burns, A., Cohen-Mansfield, J., Cooper, C. and Costafreda, S.G., 2020. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. The Lancet, 396(10248), pp.413-446.
MacLeod, C.A., Bu, F., Rutherford, A.C., Phillips, J., Woods, R. and CFAS WALES research team, 2021. Cognitive impairment negatively impacts allied health service uptake: investigating the association between health and service use. SSM-population health, 13, p.100-120.
Martin, A., Smith, R., Wright, T., Hulbert, S. and Hatzidimitriadou, E., 2021. Integrated dementia care: A qualitative evidence synthesis of the experiences of people living with dementia, informal carers and healthcare professionals. Archives of gerontology and geriatrics, 97, p.104-171.
Mayrhofer, A.M., Shora, S., Tibbs, M.A., Russell, S., Littlechild, B. and Goodman, C., 2021. Living with young onset dementia: Reflections on recent developments, current discourse, and implications for policy and practice. Ageing & Society, 41(11), pp.2437-2445.
Murphy, C., De Laine, C., Macaulay, M., Hislop Lennie, K. and Fader, M., 2021. Problems faced by people living at home with dementia and incontinence: causes, consequences and potential solutions. Age and Ageing, 50(3), pp.944-954.
Nguyen, H., Phan, H.T., Terry, D., Doherty, K. and McInerney, F., 2021. Impact of dementia literacy interventions for non-health-professionals: systematic review and meta-analysis. Aging & Mental Health, pp.1-15.
Parveen, S., Smith, S.J., Sass, C., Oyebode, J.R., Capstick, A., Dennison, A. and Surr, C.A., 2021. Impact of dementia education and training on health and social care staff knowledge, attitudes and confidence: a cross-sectional study. BMJ open, 11(1), p.e390-399.
Potter, C.M., Peters, M., Cundell, M., McShane, R. and Fitzpatrick, R., 2021. Use of the Long-Term Conditions Questionnaire (LTCQ) for monitoring health-related quality of life in people affected by cognitive impairment including dementia: pilot study in UK memory clinic services. Quality of Life Research, 30(6), pp.1641-1652.
Pujades-Rodriguez, M., Assi, V., Gonzalez-Izquierdo, A., Wilkinson, T., Schnier, C., Sudlow, C., Hemingway, H. and Whiteley, W.N., 2018. The diagnosis, burden and prognosis of dementia: A record-linkage cohort study in England. PLoS One, 13(6), p.e0199026.
Rand, S.E., Silarova, B., Towers, A.M. and Jones, K., 2021. Social care‐related quality of life of people with dementia and their carers in England. Health & social care in the community.
Sawan, M.J., Wennekers, D., Sakiris, M. and Gnjidic, D., 2021. Interventions at hospital discharge to guide caregivers in medication management for people living with dementia: a systematic review. Journal of General Internal Medicine, pp.1-9.
Smith, R., Drennan, V., Mackenzie, A. and Greenwood, N., 2018. Volunteer peer support and befriending for carers of people living with dementia: an exploration of volunteers’ experiences. Health & social care in the community, 26(2), pp.158-166.
Stamou, V., Fontaine, J.L., O’Malley, M., Jones, B., Gage, H., Parkes, J., Carter, J. and Oyebode, J., 2021. The nature of positive post-diagnostic support as experienced by people with young onset dementia. Aging & mental health, 25(6), pp.1125-1133.
Stanyon, M., Streater, A., Coleston-Shields, D.M., Yates, J., Challis, D., Dening, T., Hoe, J., Lloyd-Evans, B., Mitchell, S., Moniz-Cook, E. and Poland, F., 2021. Development of an evidence-based best practice model for teams managing crisis in dementia: Protocol for a qualitative study. JMIR Research Protocols, 10(1), p.e147-181.
Tampubolon, G., Nazroo, J., Keady, J. and Pendleton, N., 2018. Dementia across local districts in England 2014 to 2015. International journal of geriatric psychiatry, 33(8), pp.1127-1131.
Vohra, N., Hadi, M.A., Khanal, S., Kurmi, O.P. and Paudyal, V., 2021. Impact of deprivation, dementia prevalence and regional demography on prescribing of antidementia drugs in England: A time trend analysis. British Journal of Clinical Pharmacology.
Weetch, J., O’Dwyer, S. and Clare, L., 2021. The involvement of people with dementia in advocacy: a systematic narrative review. Aging & Mental Health, 25(9), pp.1595-1604.
Wheatley, A., Bamford, C., Brunskill, G., Booi, L., Dening, K.H. and Robinson, L., 2021. Implementing post-diagnostic support for people living with dementia in England: a qualitative study of barriers and strategies used to address these in practice. Age and ageing, 50(6), pp.2230-2237.
Wittenberg, Barraza-Araiza, L. and Rehill, A., 2019. Projections of older people with dementia and costs of dementia care in the United Kingdom, 2019–2040. London: London School of Economics.
Wittenberg, R., Hu, B., Jagger, C., Kingston, A., Knapp, M., Comas-Herrera, A., King, D., Rehill, A. and Banerjee, S., 2020. Projections of care for older people with dementia in England: 2015 to 2040. Age and Ageing, 49(2), pp.264-269.
 write
write