1.0 Introduction
Child obesity is a growing concern that demands significant attention at a global level as the data presented in the annual public health report 2016 stated that in an average group of 30 children, 4 children fall in the category of overweight and 5 are obese due to low physical activity and food consumption (Cambridge Insight, 2016). In essence, this essay is specifically focused on discussing the local health concern of child obesity in the United Kingdom (UK) and especially in the locality of Cambridgeshire; also, the essay has reviewed the role of nurses in addressing the health issue of child obesity in Cambridgeshire.
2.0 Virtual Research of the Local Health, Social Services and Health Service for Determining key areas of Public Health Concern
-
Local health, and Health, and Social Services in the Cambridgeshire in the United Kingdom (UK)
As per the study conducted by Vignola, Nazmi and Freudenberg (2021), the Cambridgeshire locality in the United Kingdom has registered a number of health issues relating to obesity, which has been found mostly in children. The main reason behind the health issue has been the involvement of ultra-processed food like bread, cookies, ice creams, chocolates, snacks and sugary items. In a similar context, Ribner and Mcharg (2021) have justified the implications of social media in the health aspects of children and adults. In addition, the authors have significantly focused on moral panic and obesity in children. In a particular context, as examined by Arirvatham et al. (2019), the participants/people living in Cambridgeshire mostly relate to adulthood, ranging from 40 years and above and are not much knowledgeable about the health concerns. The key-indicating sphere in Cambridgeshire is that the county is full of the natural resources needed for the development that may lead to innovation in informatics and public life science. However, since the county is divided regionally, there is a regional barrier in the regions’ development that results in fewer health care prospects and amenities among the people in Cambridgeshire.
-
Social and Health Data of the Cambridgeshire
According to Arirvatham et al. (2019), the population in Cambridgeshire is lower form the rest of the regions in the UK and has a higher quota of the adult population. The local authority share of the different regions in Cambridgeshire is divided into seven domains, i.e. income, employment, education, health, crime, housing and service barriers, human ecosystem. However, these domains assert certain deprivations on different regions of Cambridgeshire County. Apart from this, the ethnic share of the population in Cambridgeshire is not at par compared to other regions in the UK. Evidence illustrating the social and health care environment is given in the picture below:
-
Statistical Demonstration of the Social and Health Care Status in Cambridgeshire
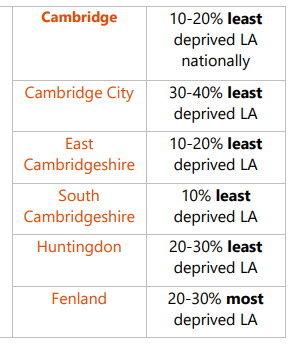
Figure 1: Showing status of a different region of the Cambridgeshire County concerning the domains stated in the statement
Source: (Arirvatham et al., 2019)
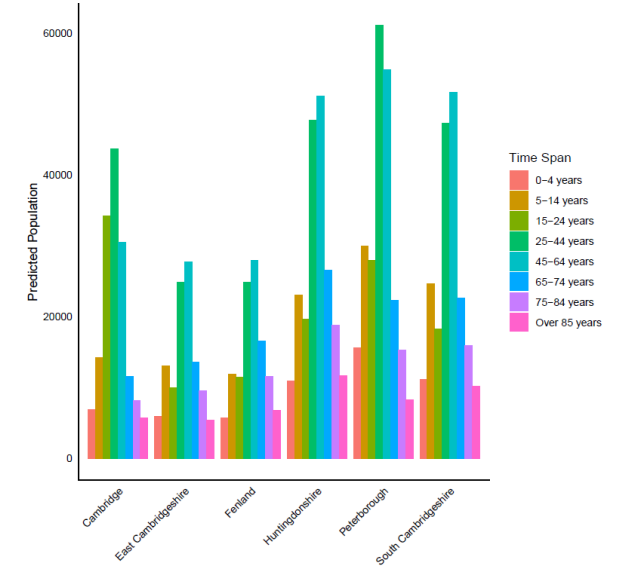
Figure 2: Showing population growth in Cambridgeshire County
Source: (Arirvatham et al., 2019).
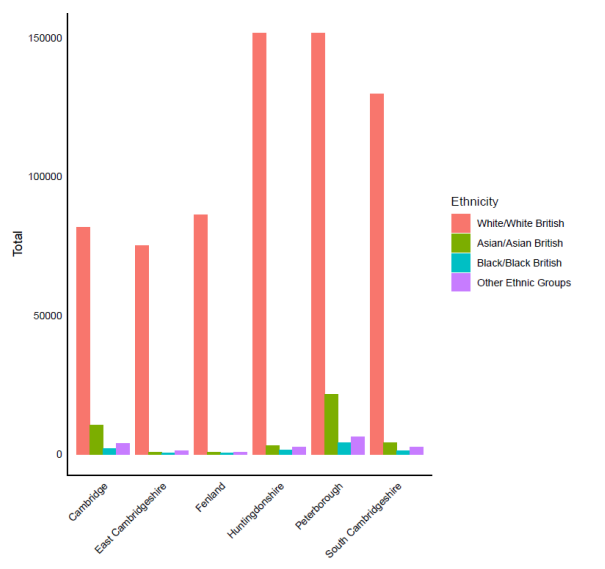
Figure 3: Showing regional ethnic population in Cambridgeshire
Source: (Arirvatham et al., 2019).
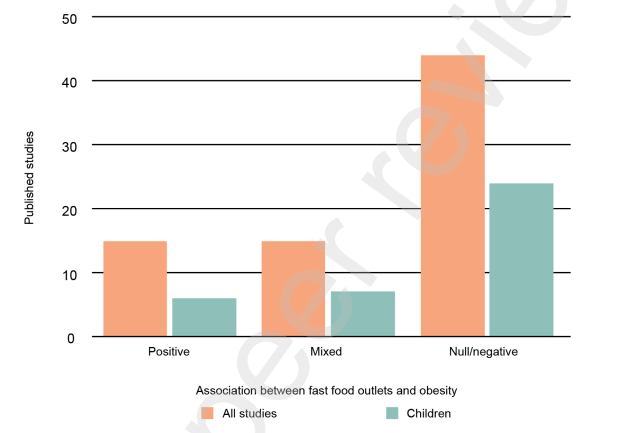
Figure 4: Showing impact of fast food on child obesity
Source: (Snowdown, 2018)
-
Discussion of Statistics Highlighting the need for Public Health Care and Implication on the Healthcare
According to Fletcher-Etherington (2021), the public health care in Cambridgeshire needs health improvements policies by choosing healthy determinants of nutrition to reduce the inequalities of the population’s health in the County, within and outside England. In addition, issues related to willingness to go to school, employment rate, and hospitalisation in case of emergencies demand great attention for their prevalence in Cambridgeshire. These issues affect the children and health outcomes directly and pose significant threats to adults and obesity. In the words of Snowdown (2018), child obesity has risen at a 4-1 ratio in such children who live nearer to the fast-food outlets in Cambridgeshire. Similarly, the author has stated that about 40% of studies have indicated accusations of fast food in generating obesity in children.
In the viewpoint of Ibrahim et al. (2020), several measures need to be adopted by the people of Cambridgeshire to reduce childhood obesity and improve the Human Mass Index in relation to other regions in England and at the international level also, which are:
- Breastfeeding at an early age,
- Proper diet and nutrition
- Proper food structure
- Increase in physical activities
- Parental interference in children health.
- Emotional development.
- Improving the mental health of children above five years in age
These measures have been extracted from a study based on the child population development in the Cambridgeshire locality in England and are designed to increase the health index of children to the row of the national and international index concerning childhood obesity. These measures will ensure sound health behaviours in children and reduce obesity in them.
Apart from this, developing eat-healthy standard programmes like Family Food First Programme and Healthy Smiles Programme for promoting children health when they have become five. Moreover, adhering to children centres and training institutes for various children related health developments like exercising, healthy eating and standard of living is also encouraged for maintaining the development framework in children who start growing above five years of age.
3.0 Discussion of the determinants, Inequalities and Barriers to health
Health as a condition or state of wellbeing is influenced by several environmental, social and societal determinants. These determinants to health affect the people in the context of their health as they are basically the accessed and available economic and social services, environmental situations and resources provided to the people. Respectively, Cambridgeshire as a county present in the east of England also homes such determinants which are avoidable, and unfair differences occur due to the conditions under which population grow, reside, function and age such as schooling, housing, health infrastructure, sanitation and other leisure facilities as shown in figure 1 (The King’s fund, 2020).
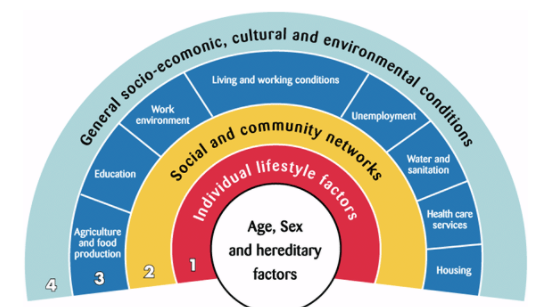
Figure 5: Determinants to Health inequalities.
Source: (Health Knowledge, 2017).
In the same context, according to the annual public health report of the year 2016, besides the known determinants to health inequalities, poverty is also a major factor as out of 12, at least 1 pupil whose age is 8 years didn’t have access to breakfast and involved in the consumption of alcohol and drinking before his/her studies, same goes for the 1 in 8 pupils whose age is 10 years lacked the necessities and involved in the same as shown in figure 2 (Cambridge Insight, 2016).
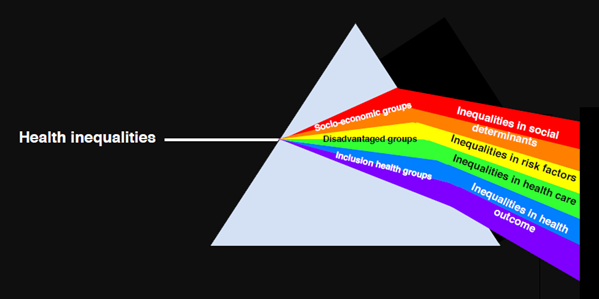
Figure 6: Health inequalities
Source: (NHS Cambridgeshire and Peterborough clinical commissioning group, 2021)
Data presented in the annual public health report 2016 indicated that in an average group of 30 children, 4 children fall in the category of overweight and 5 are obese due to low physical activity and food consumption (Cambridge Insight, 2016). As it has been observed that deprivation and obesity are correlated and are seen mostly in relation to gender and colour differences, people belonging to a black background have a high percentage to be obese and overweight at around 73%, people who belong to Chinese background are 35.3% and Asian background’s approximately 56.2%. This reflects that the people from the black community or other minority groups struggle in getting adequate support and guidance from the healthcare institutions so as to reduce the risk of developing obesity (NHS Cambridgeshire and Peterborough clinical commissioning group, 2020).
Agriculture and food production is also a key determinant that has a direct impact on the health of the people, as it affects the individual nutritional value intake because of the exorbitant prices and disparity based on race that also leads to obesity and other diet-related diseases. In Cambridgeshire, Wisbech is one of the most underprivileged wards, being low-skilled, inconsistent and insecure in addition to employing high amounts of migrant labour, ultimately leading to a low life expectancy of 6.8 years to the local men and low life expectancy of 5.0 years for women (Burgess, 2017).
Having belonged to a more prosperous area and having a degree when it comes to a successful and healthy future life are prominent issues to those people who lack such leisures. For example, some people have a double suicidal risk rate than the population in general as they don’t have an educational background which even leads to a high mortality rate (Ogilvie et al., 2016). Cambridgeshire county, as a whole, due to health inequalities, faces high losses when it comes to national productivity between £31 to £33 billion per year with insertion of NHS additional health care cost. Those insertions are majorly associated with extra spending on tackling the diseases such as obesity because of having low employment growth rates apart from the rest of the United Kingdom (Fletcher-Etherington et al., 2021). In Cambridgeshire, the employment growth rate is very less as compared to other counties present in the United Kingdom, as shown in figure 3, because of having no degrees and belonging to an uneducated background ultimately leading premature mortality with a great influence on nutrition, smoking habits and others (Plümper, Laroze and Neumayer, 2018).
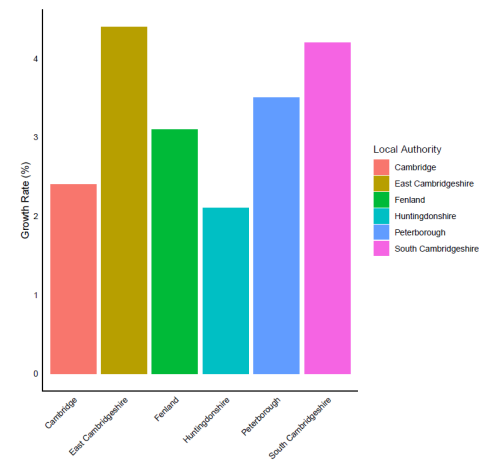
Figure 7: Growth rate in Cambridgeshire County
Source: (Fletcher-Etherington et al., 2021)
4.0 Reviewing the Services and Healthcare that are Available for the Public Health
a) Local, National Policy, Services, Charities available for Public Health Concern
Obesity in children is a severe public health issue with long-term health and developmental repercussions. The NHS and the government are devoted to empowering services to shape fitness and social health care to prevent obesity in children (Croker et al., 2012). Comprehensive family-based initiatives by the National Health Service (NHS) produced the highest results in addressing childhood obesity by identifying and managing support to obese children by monitoring and taking appropriate action at every contact. To prevent obesity in children, the NHS has made sure that the spaces for the children to run, cycle, and play are built and maintained (Hurley, Cross and Hughes, 2011).
To plan healthcare services for Cambridgeshire, the Health and Wellbeing Board and Network brings together people who buy and run services in the NHS, health care, social services, and child healthcare services. The board also provides healthcare facilities to the district facilities, elected officials, and representatives from Health Watch promote physical activity to maintain a healthy weight. The Board decides on Joint Strategic Needs Assessment (JSNA) in a collaborative effort to guide the community’s Health and Wellbeing Strategy by encouraging a healthy and nutritional lifestyle. The regular audits are conducted with compliance to food standards by the NHS to ensure nutrition intake in food. Ensuring free drinking water, capping the maximum calories per serve, nutritional labelling, reducing sugar intake and making healthy catering a good practice are the steps taken by NHS, UK (Mockford et al., 2012).
The National Institute of Health and Clinical Excellence (NICE) commissioned the study to see how well UK’s local planning authorities in Cambridgeshire, England, include health into their land use plans and development choices. In 2006, the National Institute for Health and Clinical Excellence (NICE) published advice on preventing, detecting, assessing, and managing overweight and obesity in adults and children (Swain and Sacher, 2009). NICE clinical guidelines are NHS recommendations for caring for people with specific clinical conditions. These guidelines include child obesity and circumstances ranging from self-care to prevention via primary and secondary care and more specialised services in Cambridgeshire, UK (Robertson, Murphy and Johnson, 2016).
Concerning the issues of child obesity, Clinical Commissioning Groups (CCGs) took over the planning and commissioning of health services for child obesity treatment across the UK from Primary Trust Care Trusts (PCTs) in April 2013. Clinical Commissioning Groups, led by GPs and physicians, collaborate with health care providers, patients and local communities and administrations to prevent and reduce the issue of overweight children by promoting and supporting healthy weight (Carmichael et al., 2013).
b) Looking the Role of the Nurse in Health Promotion and Screening in Cambridgeshire
Child obesity is a big problem in the United Kingdom and even in Cambridgeshire, and nurses play an essential role in identifying people at risk of gaining weight. Nurses play a significant role in providing advice and assistance to those who want to lose weight and live a healthier lifestyle (Ruxton, 2004). It is also crucial that nursing personnel maintain a healthy weight. Nurses can assist children and parents by offering dietary advice reducing calorie consumption, and boosting physical activity through weight control programmes. Nurses are given preference to adopt the whole-family approach since it is difficult for obese children to change their eating or activity habits if their families are not supportive. Nurses’ collaboration with health professionals and multidisciplinary teams promotes plans and strategies to control child obesity (Lazarou and Kouta, 2010).
Nurses are well-positioned to assess and manage child obese patients in primary care settings (National Institute for Clinical Excellence, NICE). However, the nursing profession must rise to the occasion and train nurses to have a specialised role in managing obesity. Child obesity is becoming more of a problem in Cambridgeshire as ‘Tackling Obesities’, foresight research from 2007, predicted that half of the UK population would be obese by 2050. Therefore, the nurses advise dietary and behavioural changes and a physical activity regimen to treat obese children (Penn and Kerr, 2014).
Nurses’ promotion of healthy lifestyle patterns can help reduce the risks of being obese and overweight. Breast-feeding, meals at regular intervals, physical activities, and nutrition are areas where the nurses can spread the word to decrease the risk of obesity. Many professional nurses are enthusiastic about providing dietary assistance (Banning, 2005). However, if nurses are pressed for time, eating patterns and obesity may be overlooked. They looked at the patterns of clinical practice, beliefs, and attitudes of primary care nurses concerning obesity management. They found that only practise nurses reported significant clinical engagement in this area. Other nurses and health visitors reported significantly less activity, despite believing that childhood obesity was a serious health concern and managing it was an essential aspect of their job. Weight maintenance and nutrition education are among the strategic roles that nurses and national nursing organisations can play in supporting a healthy lifestyle, according to a policy statement on obesity (Nolan et al., 2012).
5.0 Conclusion and Recommendations
Based on the statements and facts given above, a combination of two facts has been identified, which prevails in concerning the obesity level in the children to a certain degree. According to the figures, the heavy consumption of fast foods and social media usage has impacted children’s development of obesity when they grow beyond five years. Apart from this, some policies and procedures conducive to child health care have been highlighted and enumerated in the statement, which prescribes complete adherence of the nurses in exercising them to promote well being of the children. The role of parents has also been shown with complete concern for maintaining the children health. Major contributions have been mainly focused on including dietary styles, breastfeeding, taking meals at regular intervals, self-care, healthy nutrition, and regular physical activities through weight control programmes. It has also focused on strategic management of children and adult education by referring to the training of children and adults at the training and educational centres. The institute dealings are also supported by providing awareness to the children and adults of nutritional concentration to be adopted to reduce obesity during later years.
Henceforth, there is a need for employment and the adoption of new behaviours for improving the standard of living in the population of Cambridgeshire and flushing out the regional economic disparity and as against with the nation and international economic spectrum. Furthermore, to have a systematic developmental attitude, the clinical sphere, including the participation of nurses and local urban and rural bodies of a kind of authority, should conscientiously evolve their part in work to improve child health care. In addition to this, due interference of parents in child maintenance for reducing their addiction to social media is also important to reduce the child obesity threats.
References
Asirvatham, J., Thomsen, M.R., Nayga Jr, R.M. and Goudie, A. 2019. Do fast-food restaurants surrounding schools affect childhood obesity? Economics & Human Biology 33, pp. 124-133.
Banning, M. 2005. The management of obesity: the role of the specialist nurse. British journal of nursing 14(3), pp. 139-144.
Burgess, G. 2017. What is the potential for community currencies to deliver positive public health outcomes? Case study of time credits in Wisbech, Cambridgeshire, UK. International journal of community currency research 21(2), pp. 19.
Cambridge Insight. 2016. Annual Public Health Report 2015–2016. [Online]. Available at: https://cambridgeshireinsight.org.uk/search/?q=health+ineuqalities+in+cambridgeshire/ [Accessed on: 31 January 2022].
Carmichael, L., Barton, H., Gray, S. and Lease, H. 2013. Health-integrated planning at the local level in England: Impediments and opportunities, Land Use Policy 31, pp. 259-266.
Croker, H., Viner, R. M., Nicholls, D., Haroun, D., Chadwick, P., Edwards, C., Wells, J. C. and Wardle, J. 2012. Family-based behavioural treatment of childhood obesity in a UK National Health Service setting: randomized controlled trial. International Journal of Obesity 36(1), pp. 16-26.
Fletcher-Etherington, A., Mackinlay, K., Leggat, J., Baird, T., Simpson-Kent, I.L. and Rendina, C. 2021. The effect of Council decision making on the ability of Cambridgeshire communities to develop initiatives that lessen the need for formal health and social care services. Cambridge University Science and Policy Exchange (CUSPE) in collaboration with Cambridgeshire County Council, pp. 1-106.
Health Knowledge. 2017. Inequalities in health (e.g. by region, ethnicity, soci-economic position or gender) and in access to health care, including their causes. [Online]. Available at: https://www.healthknowledge.org.uk/public-health-textbook/medical-sociology-policy-economics/4c-equality-equity-policy/inequalities-distribution/ [Accessed on: 31 January 2022].
Hurley, K. M., Cross, M. B. and Hughes, S. O. 2011. A Systematic Review of Responsive Feeding and Child Obesity in High-Income Countries, The Journal of Nutrition 141(3), pp. 495–501.
Ibrahim, R.I., Bonham, A.C., Garfitt, K.J., Viner, R.M., Sewell, K., Gahagan, A., Taylor, R. and Ball, M. 2020. Learning from local authorities with downward trends in childhood obesity. Public Health England, pp. 1-34.
Lazarou, C. and Kouta, C. 2010. The role of nurses in the prevention and management of obesity. British Journal of Nursing 19(10), pp. 641-647.
Mockford, C., Staniszewska, S., Griffiths, F. and Herron-Marx, S. 2012. The impact of patient and public involvement on UK NHS health care: a systematic review. International journal for quality in health care 24(1), pp. 28-38.
NHS Cambridgeshire and Peterborough clinical commissioning group. 2021. [Online]. Available at: https://www.cambridgeshireandpeterboroughccg.nhs.uk/about-us/health-inequalities/ [Accessed on: 31 January 2022].
NHS Cambridgeshire and Peterborough clinical commissioning group. 2020. Inequalities in obesity in Cambridgeshire & Peterborough (June 2020). [Online]. Available at: https://www.cambridgeshireandpeterboroughccg.nhs.uk/easysiteweb/getresource.axd?assetid=21650&type=0&servicetype=1#:~:text=As%20outlined%20in%20the%20Foresight,individual%20psychology%20and%20social%20psychology/ [Accessed on: 31 January 2022].
Nolan, C., Deehan, A., Wylie, A. and Jones, R. 2012. Practice nurses and obesity: professional and practice-based factors affecting role adequacy and role legitimacy. Primary health care research & development 13(4), pp. 353-363.
Ogilvie, D., Panter, J., Guell, C., Jones, A., Mackett, R. and Griffin, S. 2016. Health impacts of the Cambridgeshire Guided Busway: a natural experimental study. Public Health Research 4(1), pp. 1-10.
Penn, S. and Kerr, J. 2014. Childhood obesity: the challenges for nurses. Nursing children and young people 26(2), pp. 16-21.
Plümper, T., Laroze, D. and Neumayer, E. 2018. Regional inequalities in premature mortality in Great Britain. PloS one 13(2), pp. 1-16.
Ribner, A.D. and McHarg, G. 2021. Screens across the pond: Findings from longitudinal screen time research in the US and UK. Infant Behavior and Development 63, p. 101551.
Robertson, W., Murphy, M. and Johnson, R. 2016. Evidence base for the prevention and management of child obesity. Paediatrics and Child Health 26(5), pp. 212-218.
Ruxton, C. 2004. Obesity in children. Nursing Standard 18(20), pp. 47-55.
Snowdon, C. 2018. Fast Food Outlets and Obesity: What is the Evidence? Institute of Economic Affairs Current Controversies (59), pp. 5-6.
Swain, C. and Sacher, P. 2009. Child obesity: a manageable condition. Nurse Prescribing 7(1), pp. 14-18.
The King’s fund. 2020. What are health inequalities? [Online]. Available at: https://www.kingsfund.org.uk/publications/what-are-health-inequalities/ [Accessed on: 31 January 2022].
Vignola, E.F., Nazmi, A. and Freudenberg, N. 2021. What Makes Ultra-Processed Food Appealing? A critical scan and conceptual model. World Nutrition 12(4), pp. 136-175.
 write
write