Introduction
Providing a safe atmosphere is a basic requirement of healthcare. Effective infection control and prevention are integral parts of this. This has recently been demonstrated to be of utmost significance. Numerous nursing practices have historically been founded on ritual or custom; however, this is no longer acceptable, and all treatment must be supported by research. High infection rates significantly contribute to the rising cost of providing healthcare. Therefore, it is fundamental for healthcare workers, particularly nurses, to understand the principles of infection prevention and control as it plays an integral role in the provision of quality healthcare. Tuberculosis (TB) infection is a widespread respiratory infection that affects millions of individuals worldwide. The illness can harm anyone, regardless of age or race, according to the World Health Organization. WHO (2022) notes that TB infection can be treated and prevented. For the purpose of preventing outbreaks and reducing the risk of transmission, TB control and prevention are essential. This paper will cover eight significant sections revolving around principles of infection prevention and control in Hong Kong. The history of TB infection will be covered in the first section, and the transmission of tuberculosis will be covered in the second. The management of infection control and prevention will also be evaluated in this essay, and more discussion of infection control at different levels, including the hospital setting, the general public level, and the government level, will follow. The sixth section will address surveillance and audit before moving on to policy and public health. This paper’s final portion will describe the issues and suggestions for enhancing clinical practice in TB infection control.
Background of TB infection
The bacterium Mycobacterium tuberculosis is what causes the contagious bacterial illness tuberculosis (TB). It primarily targets a person’s lungs before causing problems with the spine, joints, heart, liver, and brain (tuberculosis meningitis). This sickness is contagious and transmits from individual to individual through the air (Damani, 2012). For instance, when an infected person talks, sneezes, or coughs, the TB bacteria may escape into the air and be breathed by an uninfected person, who would then get the illness (Andrews et al., 2013). Some of the typical TB symptoms include fever, weakness, weight loss, night sweats, coughing, chest pain, and hemoptysis. The incubation period may last anywhere from three weeks to many years because some TB cases go unnoticed. According to the CDC, TB cannot be spread by handshakes, exchanging foods, touching an infected person’s linen, sharing toothbrushes, or even engaging in intimate acts like kissing. An X-ray of the chest, a sputum test, or a tuberculin skin test can all be used to diagnose TB. The most precise diagnostic method is the tuberculin test, which is carried out by administering tuberculin intradermally into the anterior forearm of a person suspected to have tuberculosis.
It is important to note that TB spreads more quickly in crowded areas. Due to close contact, crowded conditions raise the possibility that vulnerable people will come into contact with infected people. As a result, overcrowding is included as one of the primary risk factors for TB infection since it is closely related to the route of transmission, susceptibility, prevalence, and antibiotic resistance (Winthrop et al., 2016). Correspondingly, overcrowding is closely associated with factors that increase TB transmissions, such as insufficient exposure to light, inadequate ventilation, and humidity.
Chain of transmission
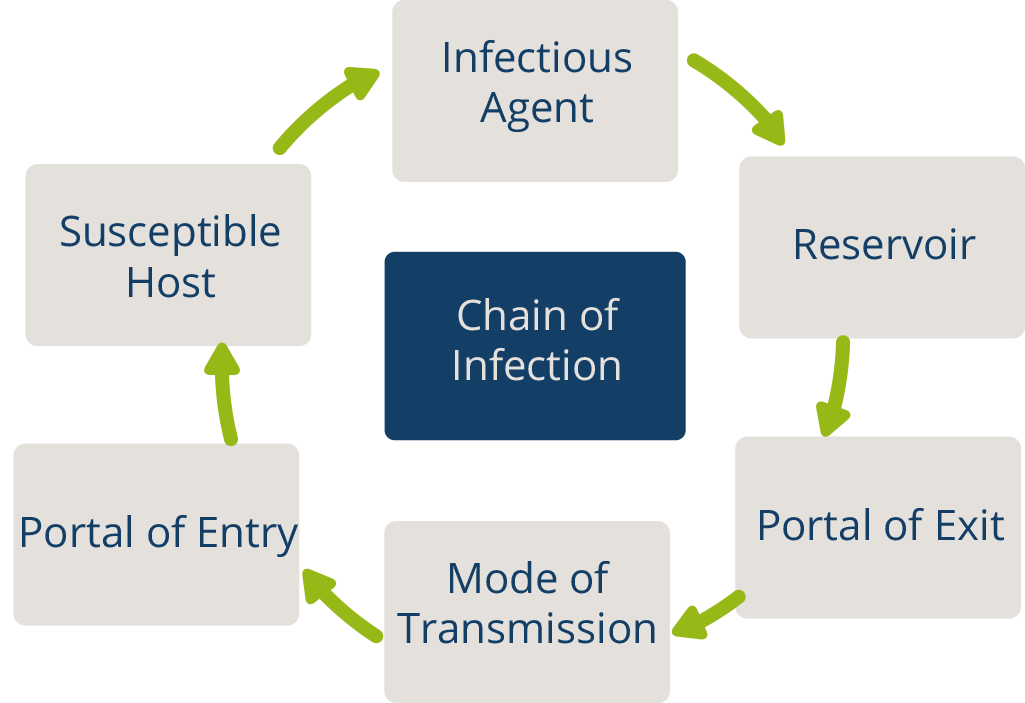
Figure 1. Diagram showing the chain of transmission. It indicates the three factors that are needed for an infection to happen: source, susceptible host, and transmission (OpenWHO, 2022).
Infectious agent
The infectious agent for tuberculosis is the bacterium, Mycobacterium tuberculosis. The bacterium is gram-positive and possesses a high potential to persist in host tissues for many years, even without leading to any infection (Damani, 2012). Mycobacterium tuberculosis is known for its great multiplication ability and capability to penetrate into the alveolar tissue with consequential damage to the lungs.
Reservoir
An animal, a person, or an object that can serve as an anchor and support for the growth of microbes can all serve as infection reservoirs. However, Mycobacterium tuberculosis primarily infects humans ((Damani, 2012). Occasionally, dead animals with the disease may still exist.
Portal of exit
The portal of exit designates the path by which an infectious organism exits the reservoir. The nose and mouth are the escape points for the microbes that cause Tb infection from the respiratory system. The TB pathogen escapes from the lungs when an infected individual coughs or sneezes (Damani, 2012). The escaped pathogen can then infect another susceptible individual and attach to his/her alveolar tissue.
Transmission mode
The point at which an infectious microbe enters a vulnerable host is known as the portal of entry. The pathogen’s nuclei travel from the inhaled respiratory droplets released by an infected person through the upper respiratory tract, the bronchi, the mouth, and the nose to the alveoli, where they land and cause illness (Tenna et al., 2013).
Susceptible host
A susceptible host is a final link in the chain of transmission of an infectious illness. The most vulnerable hosts for TB infection include immigrants from countries with high TB infection incidences, children under five years, homeless people, injectable drug users, people with HIV/AIDS, and people who are immunocompromised (Uden et al., 2017).
Infection prevention and control measures
Individual level
The warning signs and symptoms of tuberculosis should be understood, along with the ways to avoid getting infected. People should be made aware of the precautions to prevent TB infections. Anyone who thinks they might be experiencing TB symptoms should see a professional to be assessed and diagnosed. They must maintain a safe distance from other people to prevent contracting an illness before or while undergoing treatment. Additionally, it’s critical to adopt appropriate coughing techniques. When coughing or sneezing, an infected person should cover the portals of exit (mouth and nose) with a cloth or use their elbow to cover the nose and mouth. They should then wash their hands with soap and water. For the management and prevention of TB, hand cleanliness is essential (Tenna et al., 2012). To reduce the danger of transmission to healthy people, infected people are recommended to stay at home and stay away from busy public spaces. More significantly, those with TB infection are encouraged to keep their immediate surroundings clean, especially at home.
Hospital level
Healthcare organizations are currently paying greater attention to the prevention and control of infectious diseases (Wang et al., 2019). Healthcare leaders strive to ensure that their clinicians are protected from various infections such as TB by providing them with personal protective equipment as recommended by WHO. Additionally, affected individuals are isolated to protect non-infected admitted patients. Lastly, healthcare organizations engage in public education practices whereby patients and their relatives are educated about the modes, management, and control of TB infection.
Government level
The role of the government in TB infection prevention and management cannot be overlooked. Public education is the most effective strategy for lowering the transmission of TB infection. Education enables people to be in control over their health as they undertake measures to protect themselves and their loved ones. By promoting the importance of immunizations, many people may ensure that their kids receive the BCG vaccine, shielding them from contracting this serious illness. Nowadays, most newborns receive their BCG vaccination shortly after birth. The Hong Kong government has also started a campaign to inform the public of the symptoms and warning signs of TB. It cautions readers to look out for these signs and seek assistance if needed.
Regrettably, the government pays less attention to residential areas. It is alarming that a tuberculosis outbreak has spread to Hong Kong’s residential areas. The Hong Kong government should employ individuals to check the aeration in the residences there on an annual basis. Infected individuals are urged not to travel by public transit or congregate in social settings. They are advised to sleep alone in well-ventilated rooms and to regularly expose themselves to sunlight.
To prevent the spread of contagious diseases, the Hospital Authority, fortunately, maintains multiple public district hospitals. There are therapeutic standards in every hospital. The guideline includes the suggested medicine dosage and method. It makes following instructions simpler for medical staff and recent grads. The right medical attention can hasten recovery while lowering the rate of transmission. To contain a TB epidemic, the general public is encouraged to visit one of Hong Kong’s numerous district hospitals. Each district hospital has its own list of treatment guidelines that medical staff must adhere to. These recommendations, which also include dosages and administration methods, can be followed by medical workers with even a small level of training. The Hong Kong government also put in place a containment regime to reduce the movement of infected individuals.
Standard and special precautions for managing TB infection
An essential component of the prevention and management of infectious diseases like tuberculosis is the practice of good hand hygiene. Medical practitioners should practice good hand hygiene, but everyone in the community should as well. According to a study by Han (2018), hand-washing habits are associated with lower rates of tuberculosis and mortality in the local population. Hand washing is thus included in community-based health promotion efforts. Particularly, the WHO specifies a hand-washing process with seven crucial steps that must be followed, particularly by healthcare professionals dealing with infected patients.
More importantly, the Centers for Disease Prevention and Control (2022) outlines a hand-washing technique that should be followed for adequate hand hygiene. To begin, one should use running water to ensure that their hands are moist. Thereafter, lather should be made with water and soap. Then, use the phases of proper hand hygiene to rub your hands for at least 20 seconds away from flowing water. Ensure that you have rubbed the back of your hands, in-between fingers, under the nails, and around the wrist. Afterward, hands should then be dried with a dry clean towel to ensure that clean hands won’t come into touch with the tap again to prevent infection.
Moreover, when managing infected patients, healthcare professionals are encouraged to put on protective equipment such as gloves, masks, and eyeglasses. A healthcare professional must choose the most suitable PPE, given that there are various types of PPE. To prevent and manage TB, you must wear an eye shield, a mask, a face shield, and protective clothing such as disposable gowns. By using such PPE, the practitioner’s interaction with the patient’s generated droplets will be avoided or reduced (Von Delft et al., 2015). After attending to TB patients, the practitioner is required to remove the PPEs, dispose of them, and use the previously mentioned hand-washing procedure (Sharma et al., 2012). Adhering to these guidelines will help in the effective prevention and management of TB infections. MacIntyre & Chughtai (2015) note that wearing face masks in hospital and community settings decreases the risk of TB transmission.
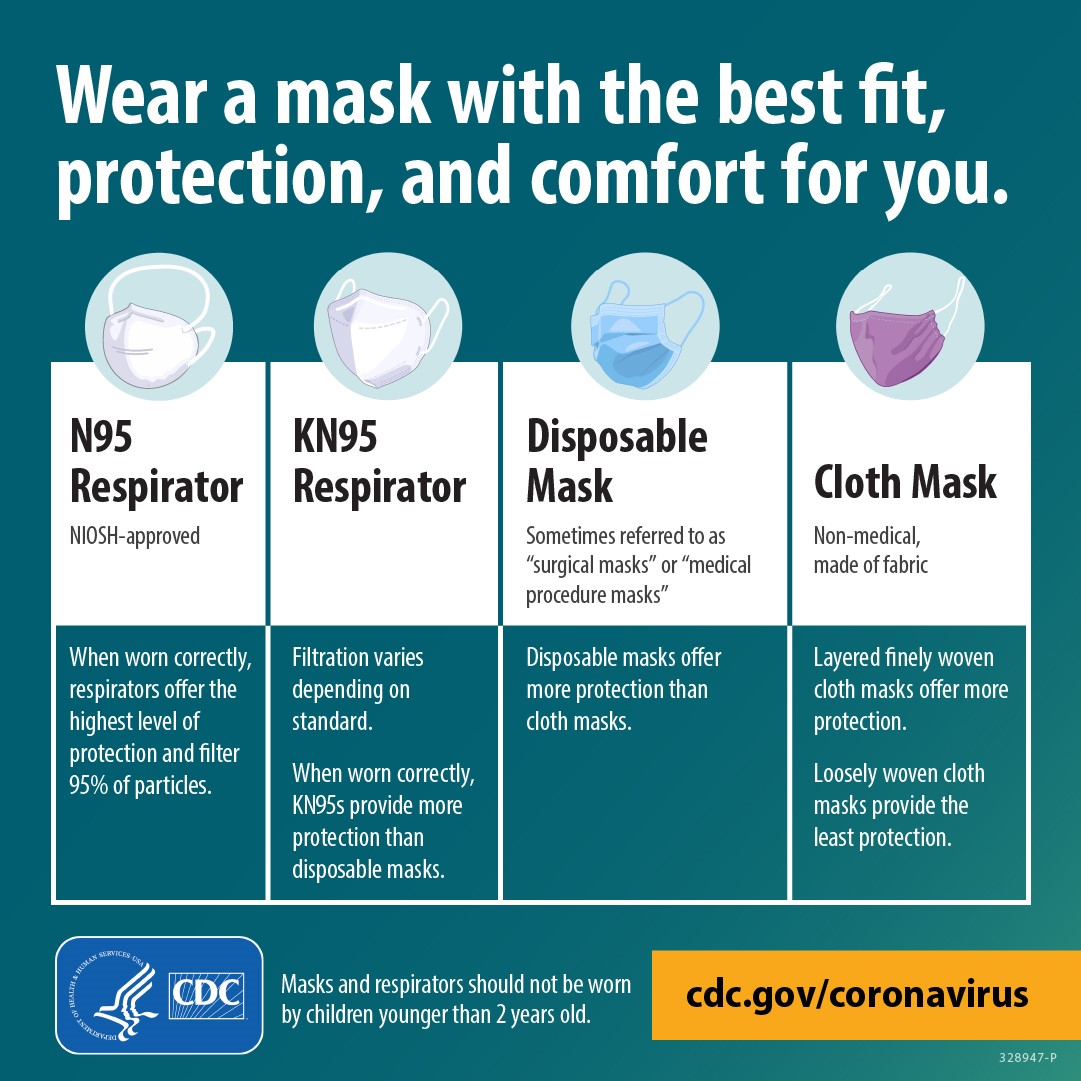
Figure 2. Guidelines for wearing a mask show various types of masks and how to appropriately wear them; N95 Respirator, KN95 Respirator, Disposable mask, and Cloth mask (CDC, 2022).
WHO recommends the isolation of infected patients to prevent transmission to non-infected patients. A sick person has to be isolated in a space where they can’t interact with other patients. For the isolation chamber, 6–12 air changes per 60 minutes of negative pressure are appropriate (World Health Organization. 2019). To prevent air from seeping into the halls, it is crucial to maintain the isolation room door closed at all times. Once the patient has been released, it is recommended to leave the room unoccupied, depending on the state of the ventilation. Then, a different TB sufferer may utilize the space.
Furthermore, because clinical waste contains blood, bodily fluids, secretions, and excretions, it must be handled carefully to limit the spread of infections. It should be against hospital policies to look inside clinical waste or handle it with bare hands. It is crucial to adhere to regional regulations when processing medical waste (World Health Organization. 2019). Similarly to this, reusable medical equipment must be thoroughly cleaned and sterilized before being used on another client.
Lastly, to avoid spreading the infection when coughing or sneezing, infected individuals must take important airborne measures (Wang et al., 2015). For airborne measures, the use of PPE is essential. A particle respirator, such as an N95 that has received the 6-NIOSH certification, is necessary while entering the room of an infected patient or doing procedures that release aerosols. Any time N95 is used, the treatment should be finished before conducting a seal inspection.
Prevention of TB infection
Local level
One of the nations with a serious TB problem in Hong Kong. The Hong Kong Hospital Authority keeps track of more than 4500 TB cases annually (Department of Health- Tuberculosis and Chest Service 2022). In order to limit and manage TB infections, federal and municipal regulations are put into practice. Locally, the TB and chest service has 17 chest clinics throughout the city that mostly provide outpatient care for TB patients. One should visit a primary care clinic or one of the chest clinics for medical attention if they exhibit TB-specific symptoms. Additionally, it is in charge of the city’s TB monitoring and surveillance. It collects TB information using notification forms, death certificates, and other surveillance programs. A summary of the surveillance data is then published online, in annual reports, or in medical newsletters. Likewise, the organization participated in TB control public health projects like defaulter recognition, regular contact with TB patients, and health promotion (Center for Health Protection 2019). Remarkably, the service is significant since it studies respiratory disorders like TB. In the end, the business operates two X-ray centers and a pneumoconiosis clinic that treats patients with the condition.
Government level
Regulations have been implemented by the Hong Kong government to stop the spread of TB. Since TB is an infectious illness that spreads through the air, effective infection prevention and control measures must be implemented (Gao & Yu, 2020). The Hospital Authority oversees the management of public health services in Hong Kong (HA). A principle that restricts visitors during the first two weeks was developed by the HA. TB sufferers are allowed to work from home but not at their places of work. They are also not permitted to participate in enclosed public events or activities.
Audit, Surveillance and Risk Management
Audits are particularly important for controlling and preventing infections. Clinicians conduct audits using a step-by-step process and criteria for improvement. An infection prevention and control audit, according to the Department of Health (DH), can help ensure that outpatient facilities continue to follow the recommended infection control practices while also helping to improve compliance with infection control regulations (World Health Organization. 2019).
Through surveillance, information about tuberculosis infection can be tracked and assessed. The statistics from the Global Tuberculosis Report (2020) demonstrate that there were approximately 10 million TB cases globally in 2019, and the proportion is progressively decreasing. In the surveillance, men’s infection rates are significantly higher than those of women and youngsters. 56% of males and 32% of women, respectively, have TB. Only 12% of children have the disease. This serves as further evidence of the importance of TB protection, not just for the people of Hong Kong but also for the entire world. TB cases sometimes tend to congregate in educational settings. According to a DH spokeswoman, the common clustering is brought about by delayed diagnosis or manifestation due to the long latent periods, which make it difficult to identify the common features early.
Notably, identifying which tasks and procedures put patients, guests, and clinicians at risk is the first step in risk mitigation. If eliminating risks is not achievable, then every attempt must be made to lessen them. Eliminating risks is the optimal way to manage hazards. Following hazard identification comes risk assessment, and then comes risk management. Following identification, aspects of TB that affect patients and medical staff are recorded. After determining the risk levels, options for lowering risk or injury are presented (World Health Organization. 2019). Because risk management improves patient safety and ensures effective clinical practice, the rate of TB transmission from patients to healthcare staff has decreased.
Public health and policy
The Prevention and Control of Disease Ordinance is a piece of legislation or policy that outlines risks to the public’s health as well as related laws and public health advice. The law states that there is a legitimate possibility that someone could suffer harm. By definition, “contact” refers to coming into contact with someone who might expose you to infectious diseases. Recessive indications in an individual can be discovered by routine medical evaluation and surveillance.
Problems and Recommendations
The principal challenge associated with the prevention and control of TB in Hong Kong is the existence of multi-drug resistance tuberculosis (MDR-TB). MDR-TB is not destroyed by the principal anti-TB medicines such as rifampicin and isoniazid (Zhang et al., 2012). Because MDR-TB is so challenging to treat, patients who have it have a terrible prognosis. The best way to overcome this resistance is to enhance public awareness of the importance of early diagnosis, successful anti-TB medication use, and regular medical visits for surveillance (Fox et al., 2017). Comprehensive and efficient TB testing, including the use of molecular assays, can aid in the detection of MDR-TB and afterward help start the patient on the proper anti-TB medications. Taking the recommended dosages at the scheduled intervals is another requirement for MDR-TB mitigation.
Secondly, high immigration rates from countries with high TB prevalence, such as India, Vietnam, and China, increase the rates of cross-border transmission of TB infection (Babu, & Laxminarayan, 2012). Overcrowding, a significant risk factor for TB transmission, can be caused by immigration. Frequently, immigrants are not adequately educated on TB prevention and control (Tam et al., 2018). In order to reduce the spread of the infection owing to immigration, it is advised that public education about TB infection prevention and control be improved. The government should instruct the populace using a variety of channels, including social media, and by hiring teachers to train individuals in rural places.
Conclusion
Tuberculosis constitutes one of the most widespread infectious diseases that afflict people worldwide. Overpopulation is a significant risk factor for TB, resulting in populous nations like China and India struggling with TB care and prevention. The best method for containing a TB outbreak is infection prevention and control measures. In Hong Kong, the disease is being stopped and managed by municipal and governmental initiatives. The government upholds laws to ensure public safety, and TB & CS encourages local infection control.
References
Andrews, J. R., Morrow, C., & Wood, R. (2013). Modeling the role of public transportation in sustaining tuberculosis transmission in South Africa. American journal of epidemiology, 177(6), 556-561.
Babu, G. R., & Laxminarayan, R. (2012). The unsurprising story of MDR-TB resistance in India. Tuberculosis, 92(4), 301-306.
CDC (2022, August 11). Coronavirus disease 2019. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/communication/masks.html
CDC. (2022, March 14). When and how to wash your hands. https://www.cdc.gov/handwashing/when-how-handwashing.html
Center for Health Protection. (2019). Tuberculosis. Centre for Health Protection. https://www.chp.gov.hk/en/healthtopics/content/24/44.html
Damani, N. (2012). Manual of infection prevention and control.
Department of Health- Tuberculosis and Chest Service. (2022). Tuberculosis & chest service. https://www.info.gov.hk/tb_chest/en/contents/c611.htm
Fox, G. J., Schaaf, H. S., Mandalakas, A., Chiappini, E., Zumla, A., & Marais, B. J. (2017). Preventing the spread of multidrug-resistant tuberculosis and protecting contacts of infectious cases. Clinical Microbiology and Infection, 23(3), 147-153.
Gao, X., & Yu, J. (2020). Public governance mechanism in the prevention and control of the COVID-19: information, decision-making and execution. Journal of Chinese Governance, 5(2), 178-197.
Global tuberculosis report (2020). Retrieved October 22, 2022, from https://www.who.int/publications-detail-redirect/9789240013131
Han, M. A. (2018). Hand hygiene and tuberculosis risk in Korea: An ecological association. Asia Pacific Journal of Public Health, 30(1), 67-74.
Hanson, M. A., & Gluckman, P. D. (2015). Developmental origins of health and disease–global public health implications. Best practice & research Clinical obstetrics & gynaecology, 29(1), 24-31.
MacIntyre, C. R., & Chughtai, A. A. (2015). Facemasks for the prevention of infection in healthcare and community settings. BMJ, 350.
OpenWHO. (2022, August 10). Introduction to infection prevention and control (IPC). https://openwho.org/courses/IPC-INTRO-EN
Sharma, S. K., Mohanan, S., & Sharma, A. (2012). Relevance of latent TB infection in areas of high TB prevalence. Chest, 142(3), 761-773.
Tenna, A., Stenehjem, E. A., Margoles, L., Kacha, E., Blumberg, H. M., & Kempker, R. R. (2013). Infection control knowledge, attitudes, and practices among healthcare workers in Addis Ababa, Ethiopia. Infection Control & Hospital Epidemiology, 34(12), 1289-1296.
Uden, L., Barber, E., Ford, N., & Cooke, G. S. (2017). Risk of tuberculosis infection and disease for health care workers: an updated meta-analysis. In Open forum infectious diseases (Vol. 4, No. 3, p. ofx137). US: Oxford University Press.
Von Delft, A., Dramowski, A., Khosa, C., Kotze, K., Lederer, P., Mosidi, T., … & Zumla, A. (2015). Why healthcare workers are sick of TB. International Journal of Infectious Diseases, 32, 147-151.
Wang, L., Wang, Z., Ma, Q., Fang, G., & Yang, J. (2019). The development and reform of public health in China from 1949 to 2019. Globalization and health, 15(1), 1-21.
WHO, (2022, October 27). Tuberculosis. World Health Organization. https://www.who.int/news-room/fact-sheets/detail/tuberculosis#:~:text=Key%20facts,with%20tuberculosis(TB)%20worldwide.
Winthrop, K. L., Park, S. H., Gul, A., Cardiel, M. H., Gomez-Reino, J. J., Tanaka, Y., … & Valdez, H. (2016). Tuberculosis and other opportunistic infections in tofacitinib-treated patients with rheumatoid arthritis. Annals of the rheumatic diseases, 75(6), 1133-1138.
World Health Organization. (2019). WHO guidelines on tuberculosis infection prevention and control: 2019 update (No. WHO/CDS/TB/2019.1). World Health Organization.
Zhang, Y., Chiu Chang, K., Leung, C. C., Wai Yew, W., Gicquel, B., Fallows, D., … & Zhang, W. (2012). ‘ZS-MDR-TB’versus ‘ZR-MDR-TB’: improving treatment of MDR-TB by identifying pyrazinamide susceptibility. Emerging microbes & infections, 1(1), 1-4.
 write
write