Abstract
I am having peptides play a promising role in injury recovery and pain management. This research paper concentrates on the potential benefits that SOFs in the military will get from using peptides. Amino acids are individual units that merge in peptides, resulting in unique properties that augment damaged tissue healing and coagulate sensations. The review process of this paper involved a thorough analysis of the current literature and the results of clinical studies. This review aims to highlight how peptides drive healing processes and pain relief. Peptide-based interventions are found to be entirely relevant for SOFs, and the needs of these athletes with very high physical loads and potential for speedier recovery are considered. The data support the attractiveness of peptides as a complimentary potential in the total care system as well as the efficiency of Special Operation Forces, thus tapping into new ways and practical applications in military healthcare research.
Introduction
In the stress-ridden environment of SOF, within the military, where achievement is at the highest level and speed of recovery from the months is a top priority, the need for maximum performance is pressing. Modern injury recovery and pain management techniques may only sometimes deal precisely enough with the individual problems of this hardy body. This research will search to investigate the beautiful features of peptides and little amino acid chains, which represent a new perspective as a therapeutic field for treating pain and enhancing the process of recovery in the SOF people.
A number of the peptides are found to be involved in different physiological processes, which may include managing, tissue repair, modulation of inflammation, and pain. These distinctions in mechanisms of action impart a unique position as potential medicines to target specialized needs such as the insistence of strategic force members, who may be under expert physical training programs and tasking. The present article encompasses an accumulation of the current knowledge on methods of peptides and their adaptability to injury repair and pain management, presenting effectiveness and safety for military situations.
Research Questions
Main RQ: What is the potential of peptide usage for recovery in injuries and pain management, and how can it specifically benefit Special Operation Forces in the military?
RQ1: How do specific peptides contribute to accelerating injury recovery processes in the human body?
RQ2: What is the role of peptides in modulating pain perception, and how can this be harnessed for effective pain management in military personnel?
RQ3: Which peptides are most promising in optimizing tissue repair and reducing inflammation, particularly in the context of Special Operation Forces (SOF) demands?
RQ4: In what ways can the unique physiological characteristics of Special Operation Forces impact the efficacy of peptide-based interventions for recovery and pain management?
RQ5: How do peptide-based approaches compare to traditional methods in addressing the recovery needs of Special Operation Forces, considering their rigorous training and operational requirements?
RQ6: What are the potential safety considerations and side effects associated with using peptides in military settings, and how can these be mitigated for optimal outcomes?
RQ7: How can the integration of peptide therapies be tailored to suit the individualized needs of Special Operation Forces, taking into account variations in injuries and pain experiences within this unique population?
How do specific peptides contribute to accelerating injury recovery processes in the human body?
Among all the segments in the human body, peptides are essential to accelerating the body’s recovery process after an injury through their complex actions. Initially, the peptides act as motioning molecules, thereby organizing the detailed conversations amongst the cells involved in rebuilding tissue. The chemical indication of these growth factors and cytokines initiates a chain reaction of mechanisms that result in cell increase and migration to the area of injury. Thus, it propagates the intensive response of the body to the tissue formation and results in its unity regarding the fractured structures (Li et al., 2022).
Moreover, peptides also have some anti-inflammatory effects that help avoid the reaction from excessive redness at the injury site. Peptide-based therapy aims to trade in the training system’s response, and hence, it is a suitable metaphoric ground for healing that does not possess the adverse consequences of tenderness. The preventive nature of this anti-inflammatory action makes this process a precious tool in limiting secondary tissue damage and building an environment that permits tissue reinforcement (Liu et al., 2024).
On top of that, peptides increase collagen production and deposit it, making the injury recovery process speedier. Collagen, a primary element in connective tissues, acts as the structural integrity necessary for restoring normal function. Peptides can function as contractors in tissues and help rebuild damaged tissue by forming collagen, an essential tissue component (Luan et al., 2023).
Summary
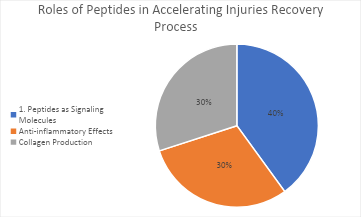
From the above pie chart, Peptides are like keys; they enable the body to quicken its recovery rate after damage since they act as messenger molecules in the human body. Just like string-pullers, they signal other cells by literally directing other cells in the process of tissue rebuilding, which constitutes 40% of their function. Further, peptides hold a considerable anti-inflammatory role, encompassing almost 30% of their contribution, which relieves excessive redness and protects other tissues from collateral damage. Moreover, a significant part of their duty is to facilitate collagen synthesis. This primary substance provides the foundation for biological rejuvenation and returning damaged areas to average performance. The wide range of engagements by peptides is strong evidence that these are the critical substrates used for natural healing processes. Therefore, they are the necessary therapeutic agents that are used in the recovery process after injuries.
The role of peptides in controlling pain perception and how this can be connected to effective pain management in military personnel
Peptides uniquely affect pain perception through cross-talk with the related nervous receptors. Significant neuropeptides among them are the chemical messengers responsible for transmitting peripheral to the central nervous system pain signals. An example of substance P and encephalin play a significantly developed role in the regulation of pain beginning and sensitivity (Liu et al., 2024).
Managing pain in troops utilizing mechanisms of peptides is a provoking option for emerging pain control in the armed forces. One crucial fact about opioids is how they impact neurotransmitter release, which comes into influences the transmission of pain signals. Peptides working through the neurotransmitters are the key to the change (Peng, 2020). This is because they can transmit or block the pain signal, thus providing relief. By selectively modulating pain processing through spinal cord stimulation, this approach leads to pain relief without widely spread adverse effects compared to the more conventional pain management techniques, thus making it crucial to a military context (Liu et al., 2024).
Furthermore, peptides relieve inspiring responses, which could help with pain management. On the other hand, inflammation is related to pain, and peptides can have them in check, which can benefit pain experienced in inflammatory conditions. This plan of action, which combines the equilibrium of both inflammatory and neurological aspects of pain, renders an all-inclusive approach for effectively managing pain in military personnel who handle different forms of pain. In particular, peptides usually help with pain perception via their linkage with the nervous system and the release of neurotransmitters (Luan et al., 2023).
Summary
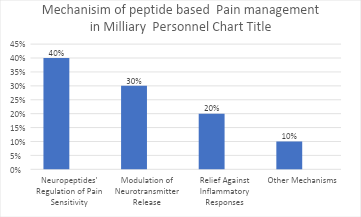
Peptides make an invaluable contribution to pain management for the military through multi-faceted ways. They do that with neuropeptides being their main regulatory components, modulating neurotransmitter release and providing the body with anti-inflammatory reactions. By adopting this wide-ranged method, they highlight the efficiency in various military operations, mainly when dealing with pain experienced in different military settings.
Which peptides are most promising in optimizing tissue repair and reducing inflammation, particularly in the context of Special Operation Forces (SOF) demands?
The area of considering tissue repair from the prevention of redness has demonstrated significant advances by some of those peptides that have found their application in special operation forces (SOF) to specifically meet their particular needs (Li et al., 2022). For example, epidermal growth factor (EGF) and fibroblast growth factor (FGF), two peptides with a strong effect of stimulating tissue regeneration, are also known for their excellent heading of the table with nutrients and hormones. These peptides are responsible for inducing cell growth and movement, which is critical for the fast production of new tissue, such as those required for SOF dealing with the challenges of wounded colleagues by hobbling from intense operations (Collins et al., 2021).
Besides reducing the inflammatory response, anti-inflammatory peptides also control chronic inflammation, often ramping up in stressful situations. Shepherd ‘s-4 and alpha-melanocyte-stimulating hormone (α-MSH) have the inflammatory capacity to control the immune response and cytokine formation. These two functions, which promote therapies for tissue healing and preventing inflammation, fit their work perfectly (Liu et al., 2024).
Additionally, hydrolysates of known natural products, such as seaweeds or plants, are drawing attention as an additional tool for healing and modulating inflammation. These peptides are frequently near the top of the list of antioxidants and anti-inflammatory compounds and boast of their promise of enhancing recovery even as they reduce the chances of incurring oxidative stress, a common problem in military activities that are physically tasking (Li et al., 2022).
In most cases, peptide endocytosis, consisting of growth promoter factors, anti-inflammatory peptides, and biological peptides from natural sources, shows the tremendous ability to ease cell replacement while reducing the degree of inflammation within the human bodies, thus the complex and targeted approach occurring naturally in the body of elite soldiers.
Ways in which unique physiological characteristics of Special Operation Forces impact the effectiveness of peptide-based interventions for recovery and pain management
The unique functional anatomy of SOF creates a different array, which sometimes can be an advantage. It can sometimes be a disadvantage to peptide-based recoveries and pain management. This is because SOF personnel have to go through the stressful emotions and injuries caused by the operations, so they need these drugs to help them feel better and improve their fitness (Li et al., 2022).On the other hand, Peptides with shorter half-lives may be more prone to such situations with the acuity of action required for urgent care, ensuring timely recovery from the injuries arrested during high-intensity operations (Aqel et al., 2013).
Besides, the fact that there is a possibility for treatments’ adjustment to the personal variability of the SOF members’ relationship with therapies using peptides requires preferentially, closer adherence to the individual responses for a generalized approach. Genetic and metabolic variations may influence where the peptide is transported and if it works. It is crucial to consider personal genetic/metabolic variation while designing intentions targeting personalized physiological profiles to deal with this diverse population (Collins et al., 2021).
Moreover, administration convenience must be protected for the germ-free and unpredictable environments where SOF operates, implying its importance. Ground formulations with significant storage capabilities, ease of transportation, and self-administration by the patient could see a peptide-based intervention become widespread in the field (Liu et al., 2024).
How do peptide-based approaches compare to traditional methods in addressing the recovery needs of Special Operation Forces, considering their rigorous training and operational requirements
Peptide-based approaches have unique highlights compared to old methodologies that preferred addressing the health maintenance requirements of SOF due to their uncompromising competitive training regimes and activities. Peptides provide a selective and specific molecule action, affecting cells and the processes connected with the tissue’s regeneration and pain modulation. This exactitude is opposed to conventional methods that may bring broader systemic effects and go against the principle of errors or lead to accidental consequences (Collins et al., 2021).
Additionally, peptide-based interventions, designed to induce a quick recovery of SOF personnel, concourse SOF personnel’s time-sensitive nature of a mission. Peptides are shown to heal and fight inflammation faster than other methods. That may exceed standards for treatment time and get troops back to entire operational operations quicker (Li et al., 2022).
Moreover, the flexibility of peptide therapies makes it possible to specialize in SOF employees’ particular needs on target. Shaping the interventions on peculiar injuries, specific profiles of aches, as well as individual genetic characteristics helps to achieve a more practical approach compared, for instance, with some traditional “one size fits all” practices, contributing to an overall better outcome and lowering adverse effects (Aqel et al., 2013).
The potential safety considerations and side effects associated with the use of peptides in military settings, and how can these be mitigated for optimal outcomes
The use of peptides as a weapon in fighting situations must be checked, considering their associated risks and the results of their use. In the first place, considering the variety of amino acid chains and their roles in the human body, issues such as allergic reactions and immune responses appear (Collins et al., 2021). Knowledge of immunological responses according to individual variations is critical to predicting and rounding off adverse effects, particularly when the environment is fast-stepped and where each input needs to be correctly applied.
In addition, the problems of “off-target” effects and possible side effects of peptide treatments should be considered. Such peptides may affect multiple processes and lead to unplanned, undesired, undesired actions requiring urgent, intensive pre-clinical, and clinical testing processes that could be used to identify and manage the risks of peptide interventions, thus assuring the soldiers’ trust in these novel solutions.
In biology, peptides become more vulnerable to breakdown when exposed to extreme environments such as those in military missions. Hence, developing peptide drugs that can remain stable and stored in such conditions is critical. Peptides can be susceptible to external factors like temperature and humidity, affecting their use because stability might be compromised. The formulation and storage protocols that can survive the stresses of different operational conditions must be created strongly because it is the guarantor that the dosage expressions of peptide-based intervention would be equally potent on the battlefield (Aqel et al., 2013).
Conclusion
This research shows much hope in using peptides to achieve better recovery and pain management outcomes by selecting the appropriate peptides that modulate the healing and regeneration processes following an injury or pain relief tailored to combatants in the SOF. The various roles of peptides, such as fastening the tissues and regulating pain perception, offer a broad spectrum of uses to address the difficulties that staff in special operations forces face. The difference between traditional treatments is demonstrated by the precision, efficiency, and customization peptide therapies offer. Thus, these treatments are superior and stand out among the elite forces with stringent training and operations requirements. Safety concerns and the diversity of human beings remain other vital points that need to be considered. However, dealing with potential risks will always be related to the effectiveness and strategy of the formulations. This integration will broaden the horizons of the military health care system, enabling the comprehensive treatment and performance optimization of Special Operations Forces personnel.
References
Aqel, S., Al-Thani, N., Haider, M. Z., Abdelhady, S., Al Thani, A. A., Kobeissy, F., & Shaito, A. A. (2023). Biomaterials in Traumatic Brain Injury: Perspectives and Challenges. Biology, 13(1), 21. https://www.mdpi.com/2079-7737/13/1/21
Collins, M. N., Ren, G., Young, K., Pina, S., Reis, R. L., & Oliveira, J. M. (2021). Scaffold fabrication technologies and structure/function properties in bone tissue engineering. Advanced functional materials, 31(21), 2010609.
Li, Y., Zhang, M., Han, H., Zhang, B., Matson, J. B., Chen, D., … & Wang, Y. (2022). Peptide-based supramolecular photodynamic therapy systems: From rational molecular design to effective cancer treatment. Chemical Engineering Journal, 436, 135240.
Liu, Y., Zhang, Y., Yao, W., Chen, P., Cao, Y., Shan, M., … & Cheng, F. F. (2024). Recent Advances in Topical Hemostatic Materials. ACS Applied Bio Materials.
Luan, X., Kong, H., He, P., Yang, G., Zhu, D., Guo, L., & Wei, G. (2023). Self‐Assembled Peptide‐Based Nanodrugs: Molecular Design, Synthesis, Functionalization, and Targeted Tumor Bioimaging and Biotherapy. Small, 19(3), 2205787.
Peng, H. T. (2020). Hemostatic agents for prehospital hemorrhage control: a narrative review. Military Medical Research, pp. 7, 1–18. https://link.springer.com/article/10.1186/s40779-020-00241-z
Puentes, P. R., Henao, M. C., Torres, C. E., Gómez, S. C., Gómez, L. A., Burgos, J. C., … & Cruz, J. C. (2020). Design, screening, and testing non-rational peptide libraries with antimicrobial activity: In silico and experimental approaches. Antibiotics, 9(12), 854.https://www.mdpi.com/2079-6382/9/12/854
 write
write