Abstract
Introduction: In general, and more specifically in the Sub-Saharan Africa, HIV infection has become a significant health concern in recent years. Interestingly, HIV can seriously affect an older person’s brain health if not treated promptly, despite being a treatable condition.
This study’s primary goal is to determine how having HIV affects maintaining brain health as we age by examining the effects of illness conditions on ageing brain health, with a particular emphasis on HIV in Sub-Saharan Africa.
Methods: This systematic review will use charts, tables, and other resources to assemble data. It goes over the background and context of HIV-related brain health, the epidemiology of HIV and dementia, and the information and resources available on HIV and dementia in different geographical locations.
Results: HIV has been associated with an increased risk of age-related dementia and other brain problems, particularly in sub-Saharan Africa.
Conclusion: Because HIV significantly affects older adults’ mental health, it is a severe cause for concern in Sub-Saharan Africa. Additional specialist resources are required to address this issue. Some of these include expanded HIV and dementia education and awareness campaigns, increased housing assistance, and improved healthcare access.
Summary
HIV, a severe health problem in Sub-Saharan Africa, may significantly impact ageing people’s cognitive abilities. Therefore, the essay will examine how HIV affects the mental health of older adults in Sub-Saharan Africa, looking at dementia prevalence, care for HIV-positive people, and services for people with dementia. The essay will also review recent research on how HIV affects ageing brain health and the results’ implications. Additionally, the report will propose strategies for addressing the knowledge gap on this topic and discuss the impact of the COVID-19 pandemic on the overall health of ageing individuals living with HIV. The essay will also explore how this topic relates to the United Nations Sustainable Development Goals.
Introduction
In Sub-Saharan Africa, HIV is a severe health problem that can considerably impact older adults’ brain health. As people age, their brain health can be affected by various conditions, including HIV. It is crucial to comprehend how HIV affects brain health in aging people to raise the quality of life for those affected by HIV. Several changes occur in the body during the natural aging process, including modifications to brain function. (Vollmer et al., 2017). This essay will explore the impact of HIV on brain health in aging by examining current literature and the implications of the findings. Additionally, the report will propose strategies for addressing the knowledge gap on this topic and discuss the impact of the COVID-19 pandemic on the overall health of aging individuals living with HIV. The essay will also consider how this topic relates to the United Nations Sustainable Development Goals.
Topic/Question
Besides discussing the effects of HIV on aging adults’ brain health in Sub-Saharan Africa, along with the incidence of dementia, services for those with HIV, and care for those with dementia, the essay will also discuss strategies for addressing the knowledge gap on this topic and the impact of the COVID-19 pandemic on the overall health of aging individuals living with HIV. Finally, the essay will consider how this topic relates to the United Nations Sustainable Development Goals.
Background
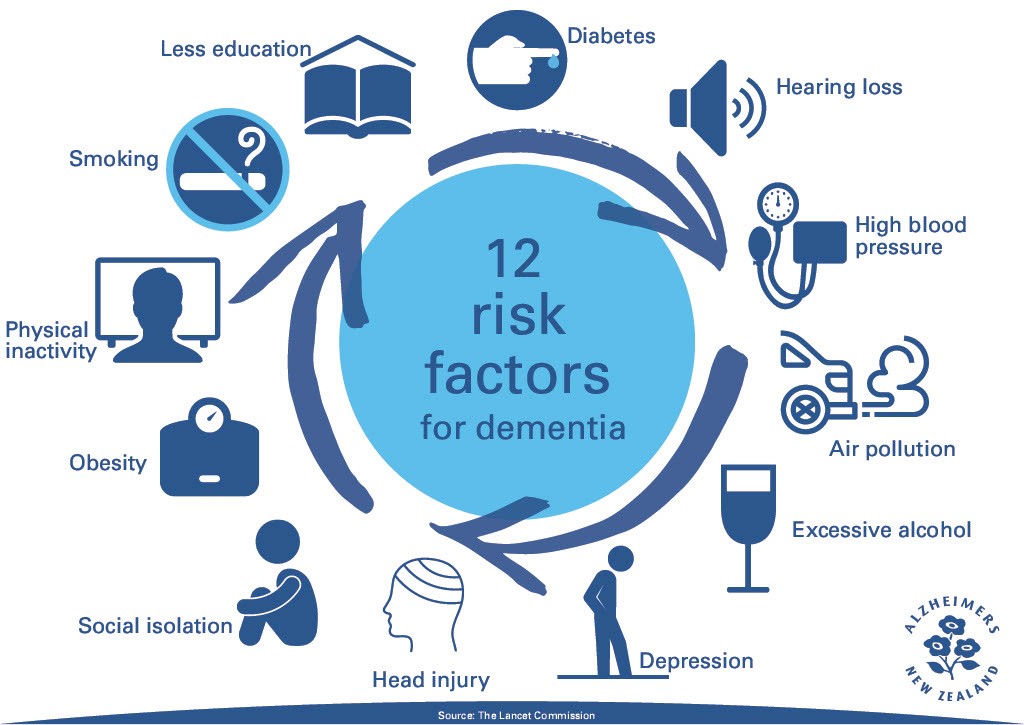
Elderly adults’ brain health can be significantly affected by HIV, a significant health concern in Sub-Saharan Africa. HIV frequently manifests as dementia, and this population has a higher prevalence of dementia than the general population (Akinny, 2016). In Sub-Saharan Africa, few services and available resources exist for people with dementia and HIV (Atef et al., 2023). HIV is most commonly spread through unprotected sex or sharing needles (Kharsany & Karim, 2016). In severe cases, the virus can impair immune function, increasing a person’s susceptibility to other diseases (Akinny, 2016). Dementia and other cognitive problems brought on by HIV can significantly lower the quality of life (Atef et al., 2023). Different studies have argued that people with HIV are more likely than people without HIV to develop dementia and that the risk increases with age (Bobrow et al., 2020). In some places, individuals with HIV and dementia might not receive the assistance and care they require because HIV and dementia are not widely recognized or understood (Kharsany & Karim, 2016). Cognitive and motor impairment, altered behaviour, and decreased functioning are all symptoms of HIV-associated dementia (HAD). A higher risk of stroke and other vascular diseases is also linked to HIV (Defrin et al., 2015).
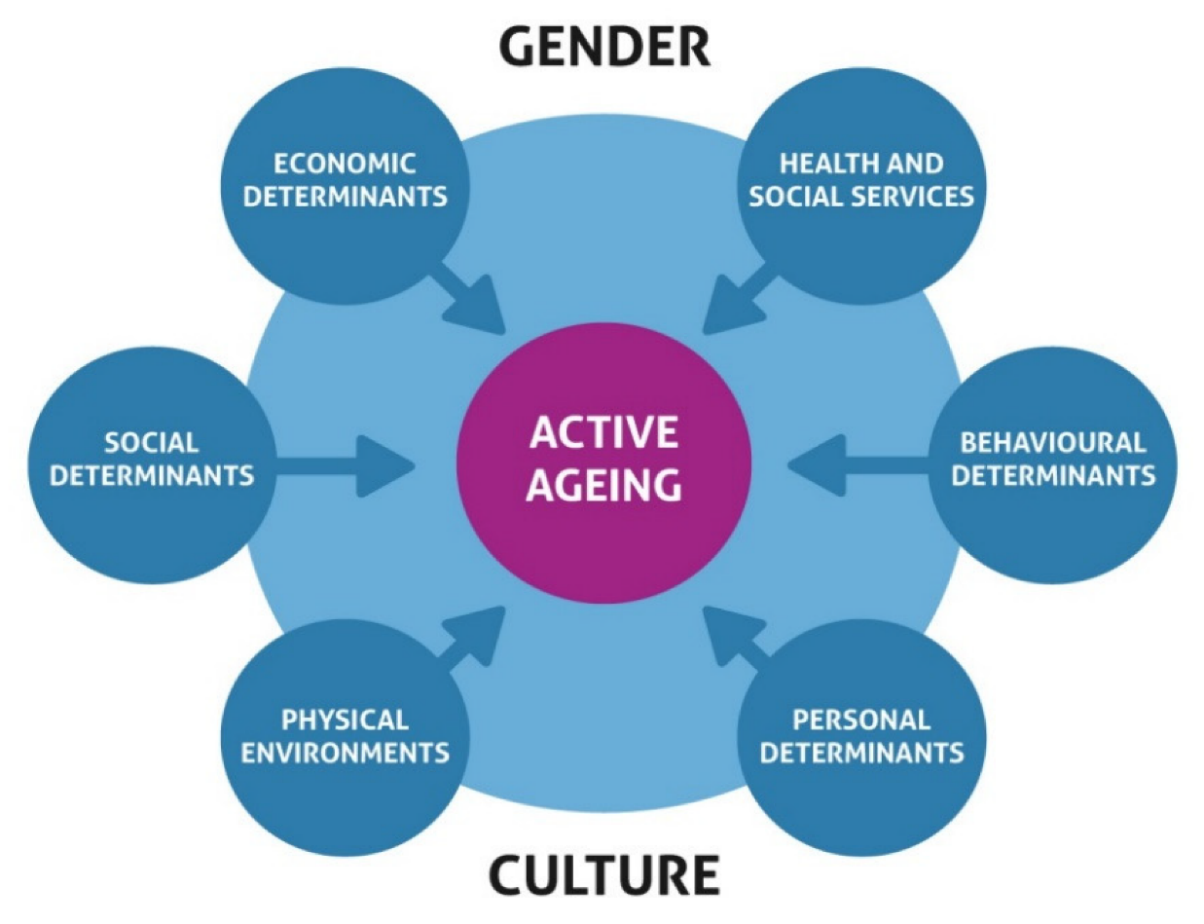
Determinants of Active and Healthy Ageing in Sub-Saharan Africa
Epidemiology of HIV and Dementia
Estimated Dementia Prevalence
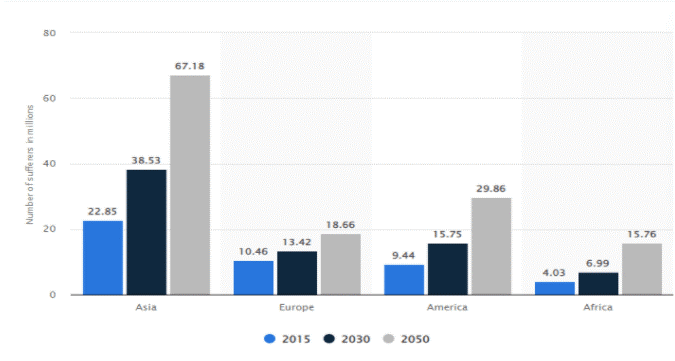
The growing number of people living with dementia highlights the importance of public health planning and policy to meet the requirements of this population. The country-level estimates can inform national planning and decision-making (George-Carey et al., 2012). Despite considerable increases in the expected number of individuals living with dementia, age-standardized both-sex prevalence remained steady between 2019 and 2050 (global percentage). To fulfil the needs of dementia patients, public health planning and policy should focus on increasing access to services, providing enough support and resources, and supporting their well-being. Better education, early diagnosis, and preventive measures should be promoted to lessen dementia’s burden (George-Carey et al., 2012).
To prevent dementia patients from being shunned, public health policy should also reduce stigma. Countries should also boost dementia treatment research and enhance access to existing therapies and strategies. Finally, public health policy should improve dementia patients’ quality of life by providing emotional and social support and suitable home and residential care. A safe and supportive environment for dementia patients can lower their risk of problems and increase their quality of life. To fulfil the needs of dementia patients, public health planning and policy should focus on improving access to services, providing enough support and resources, and supporting their well-being. Public health policy should also reduce dementia stigma, encourage dementia therapy research, and improve dementia patients’ quality of life.
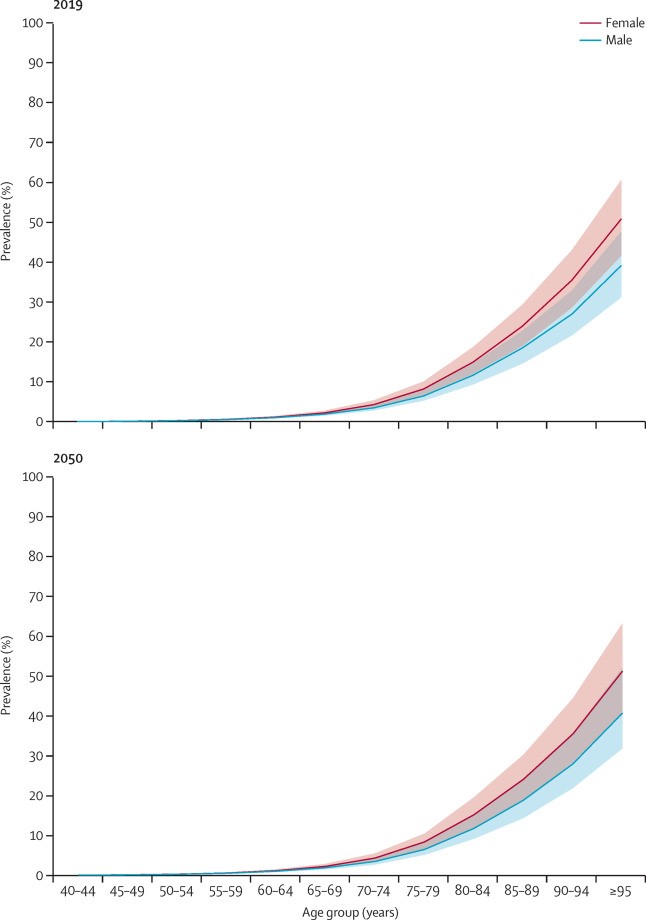
Based on different studies and research conducted by various institutions, it is expected that by 2030, 2.76 million people in Africa will have dementia, with a prevalence incidence of 2.4% among people aged 50 years and above. Females aged 80 and up had the highest prevalence (19.7%), with the minimal difference among areas (HOJILLA et al., 2021). Vascular dementia (26.9%) and Alzheimer’s disease (57.1%) were the two most frequent causes of dementia. The most significant risk variables were growing age, female sex, and cardiovascular disease.
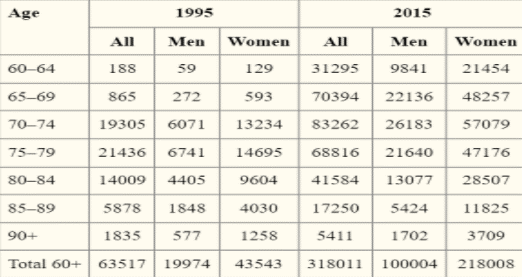
Dementia by sex
Estimated HIV Prevalence
Worldwide, [estimated range: 33.2-37.2] million persons were infected with HIV in 2020. While accounting for only 12% of the global population, Sub-Saharan Africa bears 70% of the world’s HIV load (Akinny, 2016). South Africa has been hit the hardest, with a 25% impact, followed by Nigeria (13%) and Mozambique (6%).
HIV prevalence in Sub-Saharan Africa is expected to be 5.4% in 2020, substantially higher than the global average of 0.8%. South Africa’s estimated HIV prevalence was 18.1%, Nigeria’s was 3.2%, Mozambique’s was 11.2%, and Malawi’s was 8.8%. As a result, South Africa appears to have the highest HIV prevalence, whereas Nigeria seems to have the lowest (Akinny, 2016). HIV prevalence in the United States is expected to be 0.3% in 2020. This is much lower than the global average and significantly lower than forecasts for Sub-Saharan Africa. However, the estimated HIV prevalence in the United States remained higher than in Canada (0.1%), Germany (0.1%), and the United Kingdom (0.2%). Sub-Saharan Africa will have the highest HIV prevalence in 2020, according to projections. South Africa has the highest estimated HIV prevalence rate, followed by Mozambique, Malawi, and Nigeria (Akinny, 2016). The estimated HIV prevalence in the United States was far lower than the global average and significantly lower than projections for Sub-Saharan Africa. However, it was still higher than estimates for several other countries.
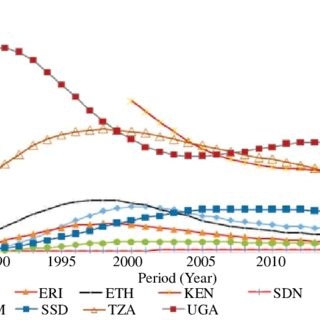
Dementia by Region
Addressing the gap/need and how to achieve it
Specifically, concerning how it affects a person’s cognitive and motor functioning, there is a lack of knowledge regarding how HIV affects brain health as people age. Therefore, we must investigate the current literature regarding the subject to build from it and fill the knowledge gap. HIV significantly impacts brain health in aging, particularly in the form of HIV-associated neurocognitive disorders (HAND). Several steps are necessary to improve the current situation, including increasing education and awareness of HAND among healthcare professionals and the general public, regularly screening people living with HIV for neurocognitive impairment, and conducting further research to understand the long-term impact of HIV on brain health in aging individuals.
- Perform longitudinal research to evaluate changes in cognitive function and brain health in people living with HIV over time.
- Determine the factors contributing to cognitive decline in HIV-positive patients and the interventions to prevent or delay cognitive decline.
- Create therapies that address particular mechanisms underlying cognitive deterioration in HIV patients, such as inflammation or oxidative stress.
- Increase healthcare access for those with HIV and dementia, including brain health assessments and therapies.
- Improve education and understanding of the impact of HIV on brain health in older people among healthcare providers and the general population.
- Advocating for legislation and funding to support research on the impact of HIV on brain health in aging, as well as the development of therapies to improve brain health in HIV-positive persons.
HIV in Sub-Saharan Africa; current status, challenges, and prospects
SDGs Addressed
This topic addresses several Sustainable Development Goals (SDGs); however, some of the most common SDGs managed by the case include; SDG 1: No Poverty – Disease conditions that impact brain health in ageing can lead to increased healthcare costs and reduced ability to work, contributing to poverty and economic hardship. SDG 2: Zero Hunger – A healthy diet is essential for maintaining brain health in aging and improving access to nutritious food can contribute to better health outcomes. SDG 4: Quality Education – Cognitive impairment and neurological disorders can impact learning and education outcomes. Addressing these conditions can improve educational opportunities for older adults. Others include SDG 17 (Partnerships for the Goals), SDG 3 (Good Health and Well-being), and SDG 10 (Reduced Inequalities). These SDGs are relevant to HIV and brain health in ageing individuals in this region as they aim to improve health and well-being, reduce inequalities, and promote partnerships to achieve the SDGs. For example, SDG 3 calls for increased access to healthcare and treatment for individuals with HIV and dementia. In addition, SDG 3 focuses on ensuring healthy lifestyles and promoting well-being for all ages.
Impact of the COVID-19 Pandemic
The COVID-19 pandemic has had a significant impact on the issue of HIV and dementia in Sub-Saharan Africa. The pandemic has worsened existing challenges, such as limited access to healthcare and support services (Carries et al., 2023). It has also created new ones, such as financial hardship and social isolation, among other issues. These issues can further complicate the management of HIV and dementia in the region.
In addition, the COVID-19 pandemic has disrupted healthcare systems worldwide, making it difficult to access quality healthcare and medical services; this is particularly true for older adults with HIV, who are more likely to experience cognitive decline and other neurological disorders (Carries et al., 2023). Additionally, the pandemic has increased stigma and prejudice against people living with HIV, making it more challenging to get the care they require (Carries et al., 2023). Additionally, the pandemic has caused stress and anxiety, which can exacerbate cognitive impairments in individuals living with HIV and dementia (Kharsany & Karim, 2016). Consequently, it is crucial to guarantee that people with HIV and dementia have access to the required healthcare and support services during any upcoming pandemic.
Analysis of HIV Concerning Public Health and Health Promotion
HIV impacts everyone and has a global impact. 14,000 Sub-Saharan Africans develop HIV daily, and 11,000 die from it or linked conditions (Akinny, 2016). Half Sub-Saharan Africans live on $1 daily (Kharsany & Karim, 2016). Poverty has been linked to HIV infection, but Sub-Saharan Africa’s high incidence has not been confirmed (Kharsany & Karim, 2016). Sub-Saharan Africa has 62% of HIV diagnoses. HIV is highest in Africa (Vollmer et al., 2016). Sub-Saharan Africa had five times more HIV than the Caribbean, seven times in Eastern Europe, 23 times in Central and Western Europe, 25 times in Asia, and nine times in North America in 2014. (Dwyer-Lindgren et al., 2014).
HIV harms communities economically and socially. HIV-related sickness can cause disability, premature death, missed wages, medical costs, and productivity (World Health Organization, 2017). HIV stigma can cause discrimination and exclusion, limiting education, employment, and health care (World Health Organization, 2017). HIV treatment and prevention cost governments and communities. HIV devastated Africa. HIV also lowers GDP and life expectancy (Kharsany & Karim, 2016). HIV also raises the risk of TB and weakens a country’s health system (Kharsany & Karim, 2016). HIV-related illnesses and deaths can lead to poorer productivity, higher medical costs, and a higher risk of poverty (Kharsany & Karim, 2016). There must be a global response against HIV. To design and implement HIV prevention, care, and stigma reduction strategies, governments, organizations, and individuals must work together. To decrease the effects of HIV on individuals, families, and communities, economic, social, and legal measures must be taken in addition to HIV prevention, treatment, care, and support.
Sub-Saharan Africa’s southern region is significantly affected. After the countries with the fastest-rising HIV cases worldwide, South Africa had the highest HIV prevalence in 2014. (Vollmer et al., 2016). Out of 52 million South Africans, 6.4 million had HIV in 2014, rising from 0.8% in 1990 and 24.5% in 2010. (Oramasionwu et al., 2011). One in six people globally had HIV, up from 4 million in 2002. (Oramasionwu et al., 2011). Ghana and Lesotho, with 230 000 and 320,000 HIV cases, respectively, are the least affected (Hanson, 2015).
Experts expect a 1.7:1.0 urban-rural HIV prevalence ratio in Sub-Saharan Africa (Hanson, 2015). Commercial sex and poverty increase urban HIV prevalence. Severe poverty in Zimbabwe and Uganda forces young women to prostitute. In Zimbabwe, families have split due to economic hardship, and extramarital affairs, especially among mine workers, are frequent (Oramasionwu et al., 2011). Rural HIV prevalence is rising due to healthcare disparities and migration (Oramasionwu et al., 2011). Rural residents’ healthcare access is limited. HIV decreases female fecundity, lowers life expectancy for HIV-positive children, and increases adult mortality in Sub-Saharan Africa. When the working-age workforce shrinks, more orphans and elderly must support their families, increasing social hardship. Since governments spend much money on subsidized HIV treatment and loss of human capacity in critical sectors like agriculture, HIV also hurts this region’s economy.
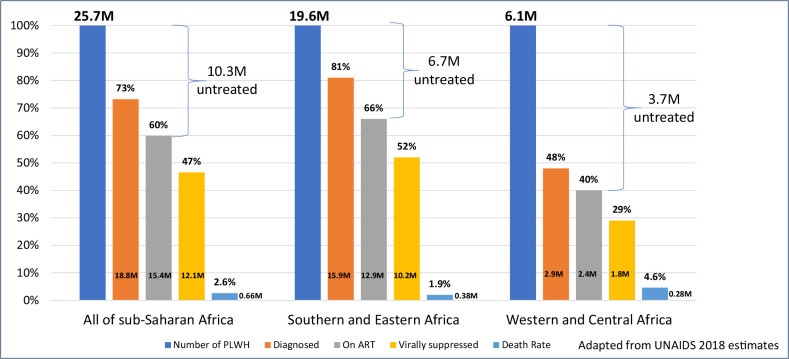
People living with HIV in Sub-Saharan Africa
Implications of HIV (Legal, Ethical, Clinical & Political)
The HIV/AIDS epidemic has dramatically impacted society in Sub-Saharan Africa. In terms of legal ramifications, HIV has aided individual states and the international community in developing non-discriminatory legislation while also fueling the epidemic’s exceptionally high prevalence. Some countries, for example, have legalized LGBT, which shields transgender persons from prejudice while also promoting HIV transmission. To combat the HIV epidemic, several preventative organizations want to decriminalize commercial sex and transgender relationships and minimize partner violence because these factors impair prevention efforts (Kharsany & Karim, 2016). Legalizing sexually transmitted illnesses, such as commercial sex work, negatively influences HIV prevalence (Vollmer et al., 2016). Because drug injection is a significant driver of HIV spread, the international community has established legislation worldwide to prohibit its usage (Vollmer et al., 2016).
People living with HIV in the Sub-Saharan region of Africa are more likely to be subjected to a stigmatising environment since HIV makes it easier for this environment to be established. Patients who test positive for HIV are subjected to psychological stigma from other community members, particularly in rural areas of Sub-Saharan Africa (Oramasionwu et al., 2011). The most vulnerable populations in the world are young women, children, gay men, and drug users. Other vulnerable groups include sex workers. Relationships between younger women and older men are linked to risky sexual activity, which increases the likelihood of HIV transmission, particularly in sub-Saharan African countries (Vollmer et al., 2016). Since 2009, the HIV infection rate among children has dropped by 43% due to increased efforts to stop the spread of the virus from mothers to their offspring. It is estimated that the prevalence of HIV infection among prostitutes in Africa will be 20%, compared to 3.9% worldwide (Vollmer et al., 2016). Although the chance of contracting HIV through injecting drugs is meager (0.02%), many people are at risk of infection.
Epidemiology of HIV AND Dementia
The epidemiology of HIV and dementia in sub-Saharan Africa is complex and, for the most part, unstudied. Infection with HIV is one of the most critical risk factors for developing dementia, particularly for people who live in isolated locations with restricted access to medical treatment (Hsu & Shrout, 2020). In addition, there is a correlation between having advanced age, having HIV for a more extended period, and having lower CD4 counts (HOJILLA et al., 2021). Cognitive decline may also be caused by comorbid disorders such as tuberculosis, hepatitis C, other diseases, starvation, drug addiction, and mental health challenges (Hsu & Shrout, 2020). Sub-Saharan Africa, which has the world’s highest HIV prevalence rates, presents a significant challenge for the public health system (George-Carey et al., 2012). Not much information is available about the correlation between dementia and HIV in sub-Saharan Africa (Hsu & Shrout, 2020). Research is necessary to understand better the causes, prevalence, and risk factors of dementia connected to HIV in Sub-Saharan Africa. This will benefit those who are afflicted with the condition and will ensure that they have improved access to care.
Discussion and Synthesis of Information
Elderly adults in Sub-Saharan Africa who have HIV are significantly affected in their brain health, a severe health issue. HIV frequently manifests as dementia, and this population has a higher prevalence of dementia than the general population. In Sub-Saharan Africa, few services and resources are available for people with dementia and HIV (Akinny, 2016). In comparison to other groups of the population, older HIV-positive individuals are more likely to acquire dementia and other brain illnesses, according to current studies. Dementia caused by HIV manifests as cognitive and motor impairment, changed behaviour, and diminished functioning (HAD). An increased risk of stroke and other vascular illnesses has been connected by research to HIV. In addition, the COVID-19 pandemic has increased stigma and prejudice against people living with HIV, making it more challenging for them to get the care they require.
Increasing public awareness of the condition and its risks is necessary to close the knowledge gap regarding the effect of HIV on brain health in aging. Consequently, to enhance the quality of life for persons impacted by HIV and dementia, more specialized tools and activities are needed. These may include improving access to healthcare, providing supportive housing, and implementing better education and awareness campaigns about HIV and dementia. The issue could also be addressed more effectively by developing better interventions and programs through collaboration and partnership between governments, organizations, and communities (Akinny, 2016). Moreover, teaching healthcare professionals how to identify and treat cognitive and motor impairments caused by HIV in older individuals is necessary. Finally, when creating interventions and programs, it is essential to consider how the COVID-19 pandemic has affected the problem of HIV and dementia in Sub-Saharan Africa.
Summary of Key Findings
The study examined how HIV affected older persons’ brain health in Sub-Saharan Africa. More specialized tools and programs are required, such as greater healthcare access, supportive housing, and more substantial HIV and dementia education and awareness campaigns (Kharsany & Karim, 2016). Governments, organizations, and communities may also collaborate to create better interventions and initiatives by establishing partnerships and cooperating to increase public knowledge of the issue. Besides, it is crucial to remember that the COVID-19 pandemic has substantially impacted the HIV and dementia issues in Sub-Saharan Africa while developing interventions and programs.
Conclusion
Conclusively, HIV can severely impact the mental health of aging individuals, a significant cause for concern in Sub-Saharan Africa. Therefore, it is evident that more specific resources and approaches are needed to address this issue, such as improved healthcare access, more housing help, and improved HIV and dementia education and awareness campaigns. Developing interventions and initiatives to solve the problem might entail cooperation and collaborations between governmental organizations, organizations, and society to comprehend better and address the situation. It is vital to consider the considerable influence that the COVID-19 pandemic has had on HIV and dementia issues, particularly in Sub-Saharan Africa, while creating interventions and initiatives.
References
Africa, S. S. The key questions. Palgrave Macmillan Studies in Family and Intimate Life, 4.
Akinny, W. D. (2016). Investigating the desirability and feasibility of the ‘Old People’s Home’as a viable business in Ghana (Doctoral dissertation).
Atef, R. Z., Michalowsky, B., Raedke, A., Platen, M., Mohr, W., Mühlichen, F., & Hoffmann, W. (2023). Impact of Hearing Aids on Progression of Cognitive Decline, Depression, and Quality of Life among People with Cognitive Impairment and Dementia. Journal of Alzheimer’s disease, (Preprint), 1-10.
Bobrow, K., Xia, F., Hoang, T., Valcour, V., & Yaffe, K. (2020). HIV and risk of dementia in older veterans. Aids, 34(11), 1673-1679.
Carries, S., Mkhwanazi, Z., Sigwadhi, L., Moshabela, M., Nyirenda, M., Goudge, J., & Govindasamy, D. (2023). An economic incentive package to support the well-being of caregivers of adolescents living with HIV during the COVID-19 pandemic in South Africa: a feasibility study protocol for a pilot randomized trial. Pilot and Feasibility Studies, 9(1), 3.
Defrin, R., Amanzio, M., De Tommaso, M., Dimova, V., Filipovic, S., Finn, D. P., & Kunz, M. (2015). Experimental pain processing in individuals with cognitive impairment: current state of the science. Pain, 156(8), 1396-1408.
Dwyer-Lindgren, L., Cork, M. A., Sligar, A., Steuben, K. M., Wilson, K. F., Provost, N. R., & Hay, S. I. (2019). Mapping HIV prevalence in sub-Saharan Africa between 2000 and 2017. Nature, 570(7760), 189–193.
George-Carey, R., Adeloye, D., Chan, K. Y., Paul, A., Kolčić, I., Campbell, H., & Rudan, I. (2012). An estimate of the prevalence of dementia in Africa: A systematic analysis. Journal of global health, 2(2).
Hanson, S. (2015). HIV/AIDS control in sub-Saharan Africa. Science, 294(5542), 521–523.
HOJILLA, J. C., ANDERSON, A. N., GILSANZ, P., ALEXEEFF, S. E., LEVINE-HALL, T., Nicole, H. O. O. D., … & SILVERBERG, M. J. (2021). Comparison of dementia risk after age 50 between individuals with and without HIV infection. AIDS (London, England), 35(5), 821.
Hsu, S. Y., & Shrout, P. E. (2020). HIV and dementia in sub-Saharan Africa: An emerging public health concern. Global Health, 16(1), 37.
Kharsany, A. B. M., & Karim, Q. A. (2016). HIV Infection and AIDS in Sub-Saharan Africa: Current Status, Challenges and Opportunities. The Open AIDS Journal, 10, 34–48.
Mutevedzi, P. C., & Newell, M. L. (2014). The changing face of the HIV epidemic in sub-Saharan Africa. Tropical Medicine & International Health, 19(9), 1015–1028.
Oramasionwu, C. U., Daniels, K. R., Labreche, M. J., & Frei, C. R. (2011). The environmental and social influences of HIV/AIDS in sub-Saharan Africa: a focus on rural communities. International journal of environmental research and public health, 8(7), 2967-2979.
Ortblad, K. F., Baeten, J. M., Cherutich, P., Wamicwe, J. N., & Wasserheit, J. N. (2019). The arc of HIV epidemics in sub-Saharan Africa: new challenges with concentrating epidemics in the era of 90-90-90. Current Opinion in HIV and AIDS, 14(5), 354.
Ramjee, G., & Daniels, B. (2013). Women and HIV in sub-Saharan Africa. AIDS research and therapy, 10(1), 1-9.
Vollmer, S., Harttgen, K., Alfven, T., Padayachy, J., Ghys, P., & Bärnighausen, T. (2017). The HIV epidemic in sub-Saharan Africa is ageing: evidence from the demographic and health surveys in sub-Saharan Africa. AIDS and Behavior, 21, 101-113.
 write
write