Introduction
Coronavirus ailment 2019 (COVID-19) is a new illness characterized by the coronavirus 2 that causes acute respiratory syndrome ( sars syndrome (SARS-CoV-2). The new therapeutic coronavirus was discovered in December 2019 in Wuhan, China, and quickly dispersed worldwide, resulting in a currently underway global epidemic. Coronavirus is directly impacting 223 countries / regions worldwide. Worldwide, upwards of 403 million incidents and 5.78 million mortalities had been confirmed by Feb 10, 2022. According to reports, 13% of the confined acolytes and 2–5% of the cumulative peer group died. The far more affected regions are the United States, South america, Russia, Western europe, Italy, France, and the United Kingdom.
COVID-19 virus can cause symptoms ranging from mild self-limiting communicable disease to liberal interpretation pneumonia with inter significant morbidity and mortality. According to research findings, upwards of 80% of cases managed to remain symptom free, and 15% of cases manifested as mild – to – moderate with prevalent symptoms such as flu, sore throat, tiredness, and impairment of taste and smell (Beigel et al., 2020). Latent infection onset may lead to mortality thanks to large alveolar impairment and gradual respiratory distress. The virus spreads via both coming into contact with an infected person directly or indirectly (Guan et al., 2019). Individual transmissions are most common during frequent proximity, with droplets secreted by coughing, nasal congestion, and conversing. Contact with infected areas or items and afterwards trying to touch the facial landmark results in indirect propagation. It is much more infectious during the first handful days once symptoms appear, however symptomless outbreaks can also transmit the infection.
The suggested intervention methods depend on combating the propagation, which includes repetitive hygienic practices, bodily distance, containment, trying to cover the nose and mouth throughout coughs, and preventing contamination of the face with unclean hands. Furthermore, the need for a mask is advised, notably for symptoms suggestive people and their care takers (Zhou et al., 2020). In healthy people, there seems to be insufficient evidence to determine the widespread usage of masks in the general public. Even so, the majority of such prevention methods are strongly advised but have not been thoroughly researched.
The following paper will be addressing the control measures of the Covid-19 virus adopted in Hong Kong, their implementation and their effectiveness. There will also be epidemiological data to support the inferences made. The paper will also provide recommendations for the control of the disease based on concepts from levels of disease management, a major topic of study in this course.
Covid-19 in Hong Kong
Regardless of the fact that there have been over 403 million COVID-19 reports and 578 million deaths worldwide, Hong Kong seems to have a total of approximately 15,811 cases somewhere at time of the report, which is among the least per million of population within and between advanced economies. The agonizing encounter of the SARS epidemic in 2003 prompted a massive amount of animal control monitoring, which revealed that 39 percent of Chinese elongated bats may be carrying bat SARS-related respiratory syncytial virus. Recognizing that coronaviruses are susceptible to spontaneous alterations and reassortment that result in new virus genus, as well as the existence of a storage reservoir of SARS-related viral pathogens within those elongated bats, Hong Kong has predicted and primed for the re-occurence of SARS as well as other newly developed infectious agents from animal life since 2007.
Border heat scanning and consensual reversed transcription polymerase chain reaction (RT-PCR) testing for inexplicable pneumonia were initiated depending on soft information that an outbreak caused by a probable SARS-related strike was impending in Wuhan on December 31, 2019. On Jan 4, 2020, the Centre for Health Protection triggered the severe reaction level. Chinese University of Hong Kong–Shenzhen institution functioned as a sentry for Hong Kong by recognizing the very initial COVID-19 kin group who reported with signs after arriving from Wuhan on 10 January 2020 (Boseley 2020). The kinship group enabled us to confirm our in-house SARS-CoV-2 assay prior commercialized testing kits became accessible. Additionally, the kinship group demonstrated that COVID-19 could be transmitted in the institution, spreads quickly in the family setting, afflicting six out of seven individuals, and can have moderate or symptomless signs. The table below shows the number of viral tests carried out in Hong Kong between 1st January and 14th April.
Table 1. Monthly numbers of COVID-19 viral tests performed: January 1 to April 14, 2020
| January | February | March | As of April 14th, 2020 |
| 3,610 | 26,983 | 65,441 | 35,752 |
Source: Centre for Health Protection, Government of Hong Kong SAR, 2020
Control measures, Implementation and effectiveness
COVID-19 transmission has a significant danger in Hong Kong. It is one of the world’s most heavily inhabited areas, estimated to have 200 000 individuals residing in partitioned apartments of 60 sq ft or fewer. In addition, Hong Kong has a significant senior demographic, with 1.27 million adults above the age of 65 vulnerable to acute COVID-19. Hong Kong seems to be at heightened hazard of transportation incident importation, as around 150 000 individuals traverse the Shenzhen–Hong Kong boundary each day, with a further 200 000 passing via Hong Kong International Airport. Subsequently, Hong Kong experiences a chilly, dry winter that may also favor viral propagation and excellent biocompatibility.
Due to the increased count of fairly benign or symptomless cases, healthcare professionals from various healthcare specialties recommended the Hong Kong general population to start practicing widespread covering up in addition to the basic hand washing on January 24, 2020, notwithstanding several local dissension and contrary advice from the World Health Organization and international health officials. Throughout morning rush period, Hong Kong’s public’s use of face masks increased to 97 percent. This lead to a significant decrease in the number of daily infections as compared to the days before (Cheng et al., 2020). Diagram 1.1 below shows the overall curve of daily infections for the city. Just 40% of Hong Kong’s COVID-19 cases appeared domestically transmitted, and the majority of coherent groups of transmissions were associated with mask-off behaviors.
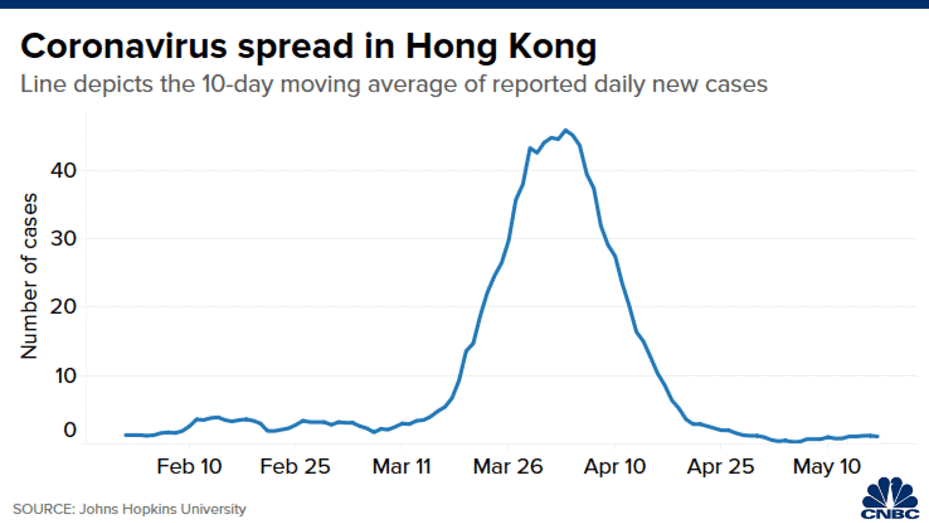
Diagram 1.1: A line graph showing 10-day moving average of reported daily new cases from the month of Feb to May 2020
Source: (Saiidi 2020). https://www.cnbc.com/2020/07/03/how-hong-kong-beat-coronavirus-and-avoided-lockdown.html
Thereby, in combination with standard customs checks, case discovering through rigorous testing, government mandated admittance for cases, quick investigations through contact tracing and containment, and social distancing approaches, global or community-wide covering up might well have provided Hong Kong an advantage in managing the regional propagation of COVID-19 (Yiu 2020). The professionalism level of Hong Kong healthcare practitioners, outstanding infection prevention and control education, and a sufficient amount of personalized protective gear culminated in zero COVID-19–related death and illness amongst Hong Kong’s hospital employees five months afterwards when the global epidemic began.
Epidemiological choices should be taken quickly enough for them to be successful, because transmission can occur 14 days even before infection is discovered. As a result, the very first infection from mainland China should have resulted in urgent border checks and isolation of travelers coming into the country. The very first abroad case should have resulted in airport screening and isolation of all abroad travelers. The growing number of small clusters of unidentified sources required more social separation. However, early case discovery is dependent on thorough testing using RT-PCR, particularly in individuals with minor dementia. Comprehensive RT-PCR testing will remain among the most significant markers used to guide epidemiological choices.
Home quarantine, partial border closure, social distancing and mass testing
Ever since announcement of a viral epidemic on Jan 25, 2020, the Hong Kong Government’s primary tactic was to limit the COVID-19 transmission by a provisional quarantine of the metropolis; all general populace sports and recreation facilities were shuttered (Hartley & Jarvis 2020). School was rescinded. Visitors from Wuhan and Hubei were barred from entering, and the bulk of crossings were closed to impede passenger movement between Hong Kong and the Chinese mainland. Throughout this incubation phase, “high-risk” persons who already had proximity encounters with the confirmed cases would be sent to a consolidated sequestered estate for screening and viral testing. In February, the precautions were broadened to include a ban on all nonresident passengers, a required 14-day domestic isolation for Hong Kong resident returns, and on-site viral screening at the airport.
Following a significant spike in infection numbers, a number of regulatory procedures were implemented. Fitness establishments, karaoke lounges, and mahjong parlors are examples of privatized spaces. A rule clause was triggered to restrict any types of assembling in public places with more than four persons (Ho et al., 2021). Eateries and catering companies were instructed to cut their initial seating by half, undertake body temp measurements on customers, and establish a minimum distance of 1.5 m amongst tables. Infringement of the new laws would result in a fine and incarceration, with law enforcement having the option of letting offenders go with a set punishment. The restriction became relaxed, but it was strengthened again in response to the second-wave breakout of illness in early July 2021. These methods appear to have been helpful in containing the regional breakout and resurgence, as well as identifying virus transmitters from high-risk areas.
Enforcement of implemented measures
Skilled medicals, emergency responders, citizen healthcare and hygiene representatives, enthusiast volunteers, and regulatory policeman were all tasked with enforcing these regulations (Sciortino & Saini 2020). Upwards of 2,000 individuals were assigned to guard the boundaries, perform virus screening, and impose quarantine measures to travelers from abroad. The consolidated quarantine facilities were manned by 1,000 volunteers, while the police, with their 30,000-able disciplinary force, were keen to check, detain, and transport scofflaws and exposed staff. The temporary lockdown of borders substantially curtailed inter and intra-city movement — incoming travelers dropped by 90%, and transportation and non-local passengers were no longer available.
According to the most recent data, the officials had conducted over 1,000 inspections of catering services, followed up on over 51,000 incidences of required quarantine, and administered over 2,000 authorized quarantine accommodations in four locations by mid-April 2020 (Ashby 2020). To improve the efficacy of enforcement agencies, the government established a helpline for the general populace to disclose cases. 144 incidents of alleged quarantine order violations were recorded, four of which were criminally charged and the culprits convicted. Upwards of 140,000 virus screenings for incoming tourists to Hong Kong were done by the Department Of health till mid-April. The ratio dominated most Asian regions, and it was likely one of the factors in the effective detention of symptomless individuals at the frontier gate and suspicious individuals in health facilities and privatized clinics.
When compared to the proportion of incoming passengers and returnees, the proportion of law enforcement officers deployed (police, Civil Aid Service [CAS], health inspectors, and volunteers) was not exceptionally large. The role of the police was mostly limited to assisting other government bodies, issuing penalty fines, court orders, or arresting people who violated the quarantine regulation (Staton 2020). The Hong Kong Police Department employs around 30,000 personnel, both plain clothed and civilian. Nevertheless, the whole force was not sent to deal with the epidemic. The number of inbound travelers as from end of March to mid-April 2020 are shown in Table 2 and 3 beneath.
Table 2. Number of inbound travelers from 19 March to 31 March
| HK residents | Mainland visitors | Other visitors | Total | |
| Airport | 52,681 | 305 | 4,784 | 57,770 |
| Hong Kong Zhuhai-Macao Bridge | 33,589 | 218 | 2,852 | 36,659 |
| Shenzhen Bay | 11,471 | 2,218 | 46 | 13,735 |
| Total | 97,741 | 2,741 | 7,682 | 108,164 |
Table 3. Number of inbound travelers from April 1 to April 14, 2020
| HK residents | Mainland visitors | Other visitors | Total | |
| Airport | 9,257 | 51 | 258 | 9,566 |
| Hong Kong Zhuhai-Macao Bridge | 775 | 82 | 36 | 893 |
| Shenzhen Bay | 7,678 | 1,253 | 19 | 8,950 |
| Total | 17,710 | 1,396 | 313 | 19,409 |
Source: Statistics on Passenger Traffic, Immigration Department, Government of Hong Kong SAR
On Feb 14, 2020, the Hong Kong Police Department launched a “Police Anticoronavirus Contingent” to assist in the enforcement of pandemic management measures. It was made up of seven operational policemen from Command Headquarters who mostly worked in the rear and 130 former cops who willingly joined (Wan et al., 2020). Their main responsibilities included assisting with the regulatory oversight of self-quarantine instructions, tracking the exact position of anyone who was answerable to the order, supervising volunteers in the executive leadership of the confinement facility, stationing at command posts to assist with the application of a digital wearable device to accurately track their adherence in remaining at their documented residential areas, and assisting at a contact centre in trying to make mobile phone calls to individuals under confinement to request them to communicate their real-time geolocation data.
Cooperation from the general public
The Hong Kong SAR Administration’s preparedness reactions appeared to be efficient, but residents’ attitudes and conduct should also be acknowledged for the “provisional success.” The vast proportion of responders stated that the low number of infections through June 2020 was due to citizen self-discipline versus legislative and regulatory competence (Wong 2020). Critiques of the government’s anti-tactics’ absurdity and flaws, as well as backlashes of unfairness as police implemented social distancing directives. The enforcement of social distance requirements was delegated to around 2,000 hygiene officials, 3,700 CAS volunteers, and temporary hired assistance. In theory, all duty and police officers, totaling around 25,000 personnel, was on the front lines enforcing social separation directives. Only seven cops and 130 retirees, nonetheless, were entrusted to these precise responsibilities. By mid-April, there were less than 10 investigated cases of isolation order disobedience presented to court. Inhabitants’ cooperation, rather than the exclusive ability of law enforcers, thereby influences the success of actions.
Conclusion and recommendations
Covid-19 pandemic continues to spread across borders since its inception in 2019. Despite numerous measure being put in place to curb its spread including administration of vaccines, the virus still keeps on mutating leading to resurgence. Hong Kong was one of the first cities to report cases of the virus. The city however implemented strict guidelines as discussed in this paper and through the collaboration of the government and the public, the city managed to prevent spread of the virus. As a recommendation measure, I would suggest mass education on the methods of preventing spread of the disease. This will act as a secondary prevention measure. I would also recommend use of monitors and video surveillance for infected patients so as to track their movements and those in contact with.
References
Ashby, M. P. (2020). Changes in police calls for service during the early months of the 2020 coronavirus pandemic. Policing: A Journal of Policy and Practice, 14(4), 1054-1072.
Beigel, J. H., Tomashek, K. M., & Dodd, L. E. (2020). Remdesivir for the treatment of Covid-19-preliminary report. Reply. The New England journal of medicine, 383(10), 994.
Boseley, S. (2020). Test and trace: lessons from Hong Kong on avoiding a coronavirus lockdown. The guardian, 17.
Cheng, V. C. C., Wong, S. C., Chuang, V. W. M., So, S. Y. C., Chen, J. H. K., Sridhar, S., … & Yuen, K. Y. (2020). The role of community-wide wearing of face mask for control of coronavirus disease 2019 (COVID-19) epidemic due to SARS-CoV-2. Journal of Infection, 81(1), 107-114.
Guan, W. J., Ni, Z. Y., Hu, Y., Liang, W. H., Ou, C. Q., He, J. X., … & Zhong, N. S. (2019). China medical treatment expert group for Covid-19. Clinical characteristics of coronavirus disease, 382(18), 1708-1720.
Hartley, K., & Jarvis, D. S. (2020). Policymaking in a low-trust state: legitimacy, state capacity, and responses to COVID-19 in Hong Kong. Policy and Society, 39(3), 403-423.
Ho, K. K. L., & Chan, Y. T. (2021). Hong Kong’s response to COVID-19: a glance to the control measures and their enforcement. Social Transformations in Chinese Societies.
Saiidi, U. (2020). How Hong Kong beat coronavirus and avoided lockdown.
Sciortino, R., & Saini, F. (2020). Towards a comprehensive narrative and response to COVID-19 in Southeast Asia. Social Sciences & Humanities Open, 2(1), 100058.
Staton, B. (2020). Lockdown measures infringe human rights, says UK justice secretary. Financial Times, 21.
Wan, K. M., Ka-ki, H. L., Wong, N. W. M., & Chiu, A. (2020). Government Capacity or Social Mobilization? The Outbreak of COVID-19 in Hong Kong. World Development, 10.
Wong, N. (2020). Coronavirus: Masks to spare? Here’s how to help those most in need in Hong Kong. South China Morning Post, 13.
Yiu, P. (2020). Hong Kongers set up face mask factory amid coronavirus panic buying. Retrieved May, 31, 2020.
Zhou, F., Yu, T., Du, R., Fan, G., Liu, Y., Liu, Z., … & Cao, B. (2020). Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. The lancet, 395(10229), 1054-1062.
 write
write