Introduction
Mental health has become a significant concern in public health over the past few decades affecting individuals across all populations. The public health systems have recognized this challenge, seeking intervention measures to improve mental health outcomes. Considering that most activities in mental healthcare still significantly rely on human participation, psychiatrists are still an essential aspect of the response to mental illness strategies. Therefore, future interventions targeting solving mental health issues at a population level need to seek options that integrate psychiatrists’ role in mental health with strategies that foster accessibility and awareness among patients. The interventions must seek to integrate the views of psychiatrists to ensure that the implemented strategies are alive to the realities of the challenges psychiatrist face as they interact with patients. This research uses qualitative and quantitative approaches to investigate the challenges that psychiatrists face in delivering mental healthcare and the challenges patients report regarding their access to mental healthcare. This research study finds that the lack of integration of mental healthcare services with the general healthcare systems poses the most significant challenge to mental health intervention as it leads to late detection and interventions, limit access for patients, and leads to psychiatrist dealing with advanced cases which in most cases are difficult to undo through conventional interventions.
Literature Review
Traditionally, mental health services have been provided separately from other healthcare services. Initially, segregation and the overall negative attitude toward mental illnesses was the primary motivation behind separating mental health and other healthcare services. However, even after the segregation of mental health patients was done away with, mental health hospitals have primarily remained separate from other healthcare facilities. On the other hand, the other healthcare services have experienced significant integration with pediatrics, adult and intensive care units being located under the same facility in most jurisdictions. Research on access to mental health services has identified that mental health services are among the least accessible in most jurisdictions. Fewer facilities primarily cause this inaccessibility compared to facilities dedicated to other health issues.
Kroenke and Unutzer (2017) investigated and reported on the sustainable approaches that could be implemented to integrate mental health services into primary care. In the article, the authors recognize that mental health disorders account for slightly above 25% of all health-related disabilities globally. The report also showed that most mental health patients receive mental health treatment from primary care facilities than from mental health institutions. There are significant deficits in mental healthcare training among primary healthcare providers, thus reducing the effectiveness of their intervention. Other issues affecting access to mental healthcare identified in the literature include inadequate reimbursement of resources into the mental healthcare system or the primary healthcare system, which limits the overall capacity to address mental health issues effectively.
Devkota, Basten and Subedi (2021) conducted a study a reported on the factors that affect the utilization of mental health services. In the study, the researcher found that mental healthcare suffers accessibility challenges experienced by primary healthcare systems. However, it also suffers other challenges that are uniquely more pronounced, such as stigma and the overall lack of awareness. This study mainly focuses on the lack of awareness and stigma, asserting that they are the leading global barriers to mental healthcare access. The researcher also found that the stigma and lack of awareness also affect policy formulations relating to mental health, including factors such as increasing the number of facilities or financing existing facilities.
Methodology
This study employed a hybrid approach involving both quantitative and qualitative approaches. The quantitative approach entailed a survey that incorporated college students who had reported having had mental health issues either presently or in the past. A group of 120 targeted participants were contacted via email and were asked to send confirmation of participation. Among those contacted, 77 (64% response rate) responded and provided consent to participate. The participants were between 19 and 27 years old. Two participants were excluded from participation after they failed to satisfy the exclusionary rule of reasonable mental stability. The remaining 75 participants were included in the survey and asked questions about their experience with mental healthcare, especially about access. The participants were gathered in a hall on campus and served with the survey questionnaires, which they were required to fill out individually without assistance. The survey required responses to be provided in numerical scores. For instance, one of the questions was: On a scale of 1 to 5, how would you rate the affordability of mental health?
The qualitative approach involved an interview with a practicing psychiatrist where questions were posed and responses recorded. Some of the questions asked include: What challenges do you face in your work? What do you think are the most common misconceptions about mental illness? The responses were recorded, and a thematic analysis was conducted. In the quantitative analysis, percentages and averages were conducted to determine patients’ perceptions of the accessibility of mental health services. This quantitative data was collected between the 17th and 22nd of April, while the qualitative interview was conducted virtually via Zoom on the 24th of April.
Findings (Quantitative)
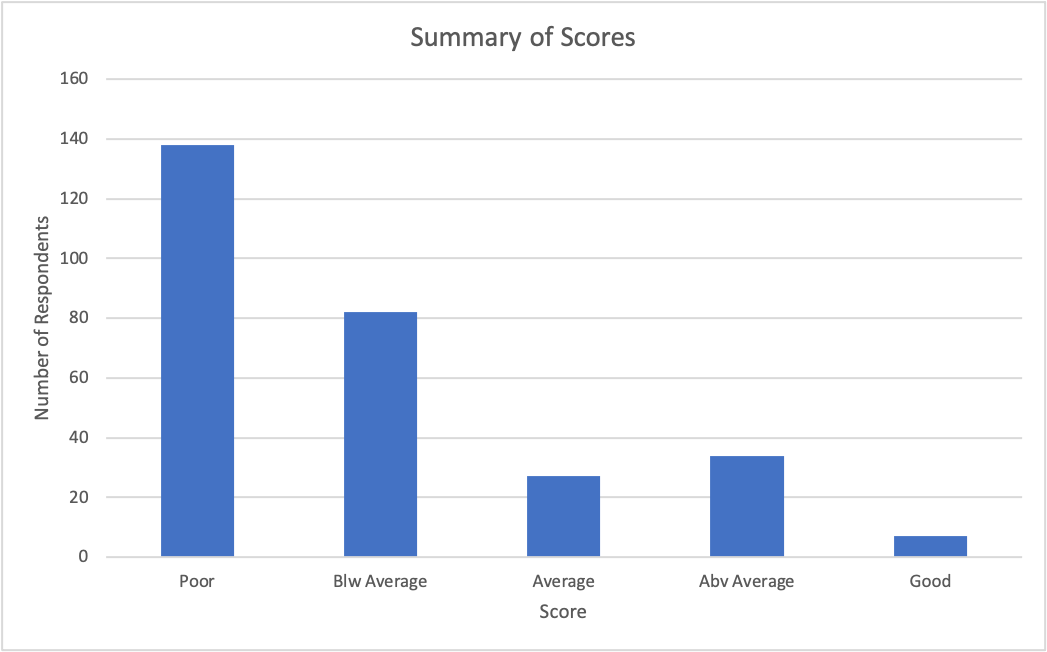
Graph 1: Summary of respondents’ scores in all the five questions asked in the survey.
The tables show the aggregated scores of the respondent’s responses to the five questions relating to their experience with mental health care services. The data shows that 138 (47.9%) answered all the questions. Responses with a score of 2 (low) were 82 (28.5%)—responses of above average and good recorded low scores of 12% and 2%, respectively.
Findings (Qualitative)
The qualitative findings revealed three main themes. The first theme was the importance of early detection and intervention. The psychiatrist emphasized detecting mental disorders as early as possible to ensure optimal outcomes. He also discussed the need for a comprehensive assessment to ensure an accurate diagnosis. He stated, “Additionally, it’s important to make sure that mental health services are integrated into primary care and that there is a greater emphasis on prevention and early intervention.”
The psychiatrist also highlighted the importance of establishing a solid therapeutic relationship with clients. “I think the most important factor in successful treatment is having the right support system in place. This includes having a good relationship with the psychiatrist or therapist, as well as having family and friends who are willing to provide support. It’s also important to have a good understanding of the illness and to be willing to work on it.”
Discussion
This study hypothesized that mental health generally experiences poor accessibility to mental health services. The quantitative findings in this project support this hypothesis as they indicate significant numbers of poor scores in all four questions asked in the survey. More than 50% of the responses in the study were below average, indicating that the respondents had a poor experience with mental health services in terms of accessibility.
The qualitative data from the interview also support the hypothesis of the study. The interviewee mentions essential details about the treatment services for people with mental health issues. One of the main themes in the discussion asserts the need for integrating mental health care with primary healthcare to make the services more accessible to mental health patients. The data from the interview also points to the need for adequate support for mental health patients both at the institutional level and remotely. The interview also shows that psychiatrists significantly suffer challenges that mainly emanate from the poor accessibility of mental healthcare.
Conclusion
Psychiatrists play a critical role in mental healthcare, considering the sector is still significantly dependent on human labour compared to other healthcare sectors. However, despite doing away with policies meant to segregate mental health patients from other patients, mental health institutions remain few and largely inaccessible to the more significant population affected by mental health disorders and illnesses. The rise in mental health diagnoses globally puts significant pressure on psychiatrists, who must use the few available resources to cater to the rising numbers of mental health patients. Research shows that mental health patients must travel long distances. To access mental health facilities, or must interact with healthcare providers with little training in mental health care. This study supports this hypothesis, indicating that both patients and psychiatrists agree that there is a significant need to develop mental health systems to cater to the general population’s needs.
References
Devkota, G., Basnet, P., Thapa, B., & Subedi, M. (2021). Factors affecting utilization of mental health services from Primary Health Care (PHC) facilities of the western hilly district of Nepal. PLOS ONE, 16(4), e0250694. https://doi.org/10.1371/journal.pone.0250694
Kroenke, K., & Unutzer, J. (2017). Closing the False Divide: Sustainable Approaches to Integrating Mental Health Services into Primary Care. Journal of General Internal Medicine, 32(4), 404–410. https://doi.org/10.1007/s11606-016-3967-9
 write
write