Abstract
Dementia is a primary world health concern, and early onset types impose an enormous burden on Health institutions and carers. This systematic review, however, focuses on assessing the role of pharmacists in the detection and treatment of early-onset dementia, underlining their significant position that enables medication management as well as enhances efficiency towards earlier detection. Using a PRISMA-guided comprehensive search across databases like PubMed and MEDLINE, eleven studies representing the pharmacist’s ability to manage medication in deprescribing to minimize dementia risks were identified. Nevertheless, the results show significant inconsistencies in pharmacists’ training and education concerning dementia coupled with difficulties related to early-onset dementia diagnosis along with polypharmacy management. Notwithstanding these obstacles, pharmacists can substantially improve patient outcomes by optimizing medication management and patient education. For this potential to be fully realized, specific training programs for pharmacists are needed; there must also be clear guidelines of what roles they play in dementia care and more research required on the subject. The present study calls for structured training of pharmacists, policy revisions to include the formal participation of pharmacists in dementia management teams, and additional research on competent practices that should be employed when providing care services to people with dementia.
Introduction
Dementia, a syndrome with multiple cognitive impairments that include memory loss, reasoning difficulties, and behavioral changes, represents a significant global health challenge. Dementia involves different subtypes, such as Alzheimer’s disease, vascular dementia, Lewy body dementia, and frontotemporal dementia. It reduces the value of life for those diagnosed and places tremendous demands on caregivers and worldwide healthcare systems (Arvanitakis et al., 2019). The primary caregiver is required to provide constant supervision on basic activities of daily living, such as bathing, dressing, and eating, while also understanding the needs and preferences of dementia patients. Moreover, Yates et al. (2021) note that the increasing prevalence of dementia strains healthcare systems as they need to allocate resources to address the growing demand for specialized dementia care, including medical professionals, facilities, and support services. This creates frustration for both the caregiver and the person with dementia.
Approximately 50 million people worldwide have dementia, and projections are showing a steady increase to close to half this number by the year 2050 (Tran, 2022) as the prevalence is also bound to increase considerably, with more and more people living their lives while demented in coming decades. NHS statistics show that 90 % of people who have dementia are older than sixty-five years and take multiple drugs (NHS,2018). Consequently, they are at higher risk of developing dementia, which could reduce the effectiveness of some particular therapies or have a negative outcome.
Pharmacology issues in dementia care are a vital element in ensuring effective treatment for patients diagnosed with cognitive impairment. A key issue, however, concerns the use of inappropriate medications that increase dementia risks, including those with high anticholinergic burden (Grossi et al., 2019). When anticholinergic obstruction of brain acetylcholine receptors occurs, cognitive impairment and long-term memory deficit can follow suit; these drugs are among the risks because individuals who have dementia tend to take such medications. Besides the anticholinergic burden relief, a holistic approach to dementia care includes non-pharmacological interventions and personalized treatment strategies. Physical exercise, cognition training, behavioral therapies, and occupation therapy are some of the interventions that may be undertaken (Thijssen et al., 2021). Thus, integrated dementia care should incorporate person-centered support and treatment networks.
Various entities advocate for the earlier presentation of dementia. The Dementia Friends is a social movement that receives backing from the Alzheimer’s Society in the U.K. and its counterparts internationally (Shannon et al., 2019). Through knowledge and education sharing, Dementia Friends aims to reduce the social stigma linked with a demented person and demystify public consciousness of that illness by promoting greater acceptance for those afflicted as it works towards creating a supportive society.
Dealing with dementia patients requires the pharmacists (Shoji et al., 2023). By recognizing symptoms and extending their role as prescribers, they assist in the early detection of dementia by either prescribing proper medications or deprescribing, which is a process that means stopping taking irrelevant medications. Nevertheless, the early stages of treatment administration and beginning care in patients with dementia are hardly issues for pharmacists. As per Nwadiugwu (2021), early-onset dementia presents a distinct set of challenges for its diagnosis and treatment in the United Kingdom. Early onset dementia remains one of the most troubling problems since, in many cases, such patients are misdiagnosed due to a mistaken belief that cognitive loss is characteristic only for senile individuals. Also, the symptoms of early-onset dementia can be atypical and easily mistaken for other diseases, thereby leading to a delay in diagnosis. It, therefore, holds that early detection and the efficacy of management contribute significantly to improved outcomes and an enhanced quality of life for people with dementia.
In the recent literature, several studies have focused on pharmacists as an opportunity to seek signs and manage early-onset dementia. This has been demonstrated in several different studies that have made suggestions concerning the approach to challenge resolution for incorporating these roles into mainstream pharmacy practice.
Although previous works recognize the role of pharmacists in dementia treatment, they call for a systematic review to aggregate all studies presented. The present literature needs to provide insight into such patterns in awareness levels, as some pharmacists are more proactive with early detection than others. Moreover, the reviews do not demonstrate how much pharmacists actively identify early-onset dementia. This systemic review aims to provide an overview of what extent patient-centered care can be delivered by pharmacists in dementia treatment, as well as explore more responsibilities they can take on.
Aims and Objectives
This study aims to conduct a comprehensive literature review on pharmacists’ involvement in identifying early-onset dementia. It aims to assess pharmacists’ level of awareness and readiness about early-onset dementia, research potential positive aspects and difficulties in developing prescribers through pharmacy professionals concerning dementia care, and conduct critical analysis, including a focus on training inside forms for education projects such as the MPharm program.
To attain the stated necessity, a widespread search operation will be carried out across databases from various sources covering pharmacological interventions instituted by psychiatrists in treating dementia. Eligible studies will be selected, including randomized controlled trials, case reports, and systematic reviews. The main endpoint parameters will be cognitive function, behavioral changes, and overall quality of life.
Methodology
The literature review methodology performed by “Preferred Reporting Items for Systematic Reviews, PRISMA” has been selected for this paper. Snyder (2019) defines literature review as a crucial stage of conducting studies, particularly as it allows the analysis of in-depth relevant research that provides knowledge on present opportunities or areas needing improvement associated with the specific issue. Thus, the chosen approach controls for aspects of strength and applicability since it systematically rates methods by success in establishing links between exposure factors and outcomes (Rahman et al., 2021). Therefore, the methodology is compatible with comprehensively assessing existing evidence based on early-onset dementia under potential evolving pharmacists’ roles. Furthermore, the study seeks to determine advanced mandates that pharmacists can accept in such an environment. Eligibility criteria are the PICO framework. Suitable studies comprise randomized controlled trials, observational doctrines, systematic reviews, and experimental and quasi-experimental plan analyses on the concerned subject (Suwa et al., 2021). The hunt will include works published between 2015 and the end times as of now, utilizing English language writing courtesies that are direly abundant in nature come after research done within the United Kingdom:
Sources of information for this review were also from databases provided by PubMed, MEDLINE ScienceDirect, and the pharmaceutical journal. Oswald (2017) notes that this eclectic choice includes medical, psychological, and multi-disciplinary sources, thus analyzing the collection of evidence available regarding pharmacists’ identification and management participation in early-onset dementia. For the search to be conducted using specific keywords, key terms on dementia care, health outcomes targeted at pharmacist specialists, and a general description of such people formed part of the keywords used. Items considered under inclusion criteria were papers and books published within the previous decade on the pharmacist’s role in dementia.
The study will have a stringent selection process since it will strictly rely on the preset PICOS elements. First, the identified articles will be screened for relevance by their titles and abstracts. Within the selected articles by Candy et al. (2015), there will be a full-text review of the study design, methodology, and outcomes to determine whether papers should or should not be included in the review process.
Data will be collected discreetly based on the requirements of piloted forms that should represent important variables and details under predetermined specifications. McGuinness et al. (2019) observe that these forms should comprise variables such as PICOS elements, relevant outcomes, and publication details to enhance uniformity in data extraction to print the tenability of the information captured easily. The data items to be extracted are made of various aspects covering the patient characteristics, intervention details, mock comparators or groups, and aggregated outcome measures with specific design components attached.
In this methodology, individual studies’ risk of bias was determined. It elaborated on the steps followed during this evaluation and their adaptation in building up subsequent data analysis. It also included the risk of bias across studies, such as publication biases or selective reporting within a study.
Key indicators suggested for the principal summary measures in a systematic review will be risk ratios and differences from means. Risk ratios are specified in the case of binary outcomes allowing to interpret how high is relative risk for certain events between intervention and control groups (Wang and Brooke, 2020). For continuous outcomes, differences in means will be used for quantifying the average change or effect size between groups.
A qualitative analysis will assess trends, gaps, and challenges in the current literature regarding pharmacists’ incorporation into identifying and managing early onset dementia within healthcare settings. Further, a review matrix will be used to visualize the central concepts within the articles identified and aid in the structured and efficient analysis.
Finally, the methodology was described by merging data and combining individual study findings and prespecified and other supplemental analyses such as sensitivity analysis subgroups or meta-regression. A thorough review was accurate and enlightening on the current knowledge of promoting dementia awareness in healthcare.
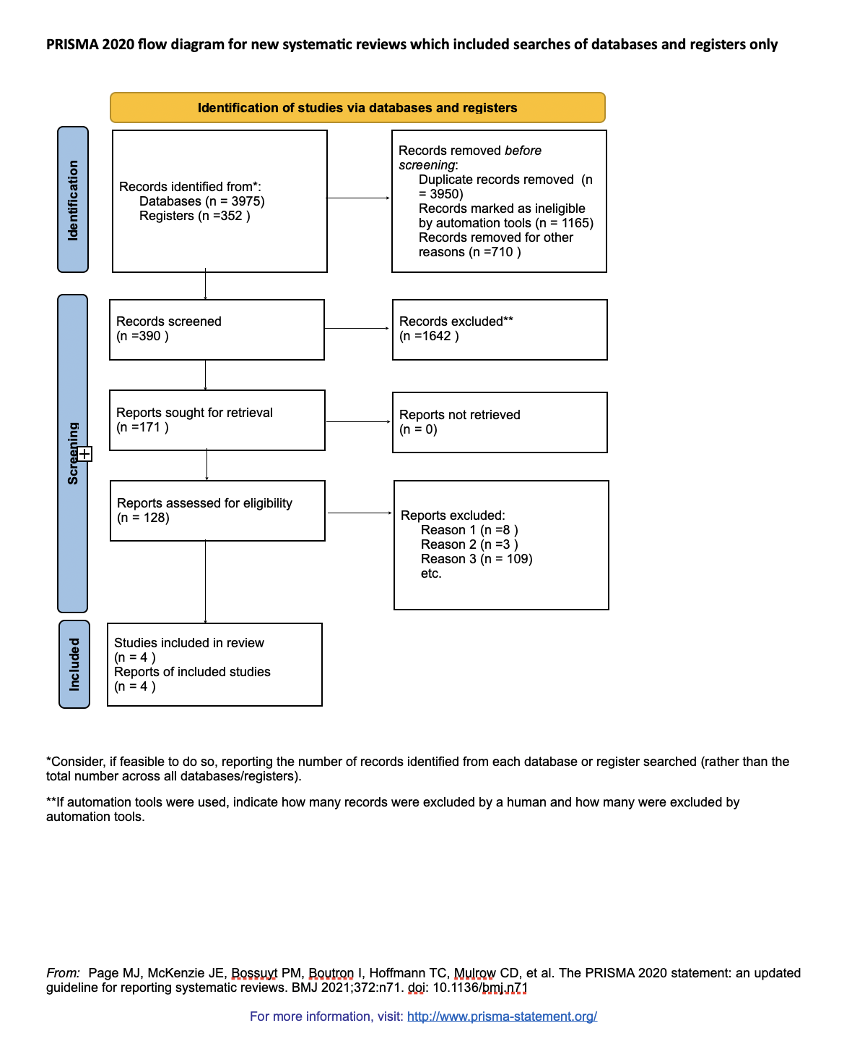
(PRISMA TRANSPARENT REPORTING of SYSTEMATIC REVIEWS and META-ANALYSE, 2021)
How Has Research Been Conducted So Far?
The use of diverse sources allowed for an elaborate examination of existing literature on dementia awareness within healthcare and the role of pharmacists in this sense. Key studies like those of Levine and colleagues (2021) and Suwa and researchers (2021) helped to understand how the pharmacy contributes to helping dementia care.
This study revealed that additional educational sessions need to be conducted to boost capacity building by providing adequate health care information to their patients. It was also found that pharmacists’ involvement is imperative since they play a vital role in patients’ clinical management. Besides, there are difficulties in dealing with a vast body of literature and interpreting conflicting results. This article presents an up-to-date overview of pharmacy’s role in dementia care, highlighting gaps where additional research and efforts are needed.
Results
Search Results and Included Studies Characteristics
The search was broad across the PubMed, MEDLINE databases, ScienceDirect, and the Pharmaceutical Journal register. During the identification phase of the systematic review, 4327 records were located from database searches, including registers with 3975 documents coming out from various databases. Before the screening process, 3,950 duplicates were identified by automation tools, and 710 were eliminated. The screening phase included checking 390 records, resulting in the elimination of 1642 records. In carrying out the eligibility assessment of these reports, 128 were read in detail, and another 37 were excluded for specific reasons. After this strict screening selection, only 11 studies were finally incorporated into the systematic review.
Overview of Findings
Dementia in general, but early-onset dementia especially, is increasingly being seen as a significant global health problem. It is a multidomain dementia that manifests as multiple cognitive deficits such as loss of memory, thinking ability complications, and emotional regulation problems. These deficits severely lower the quality of life for those diagnosed while significantly straining caregivers. In addition, rising cases of dementia continuously push health systems to the limit as they have no choice but to spend on both medical care personnel and facilities for specialized dementia treatment.
One of the pharmacists’ responsibilities is detecting and managing early-onset dementia. They uniquely support early identification of the symptoms and prescribing or stopping medication. This position is of particular importance as dementia often represents several subtypes and hampers the efficacy of one or another treatment, resulting in adverse outcomes. Therefore, pharmacists’ involvement is critical in providing optimal therapy to individuals suffering from cognitive loss because they help mitigate significant limitations that underline targeted treatment.
Although there are great benefits attached to the early detection of dementia, it has been a major challenge in the health system. Such a situation most typically results in misinterpretation of the condition, for instance, assuming that cognitive impairment is not limited to only specific individuals. Moreover, the symptoms of early-onset dementia are atypical and often can be mistaken for other diseases; these complications further disturb diagnosis-making. It necessitates a holistic approach that includes early detection, effective response, and support provided to victims.
The current literature recognizes the importance of pharmacists. However, more research is needed. There are recommendations for those two roles to be intertwined in everyday pharmacy practice, but more research is required on the role of Pharmacists in dementia care. This involves looking into extended roles that pharmacists can take on under this particular setting if such a form would result in benefits or challenges.
One more vital issue in improving dementia care is education. More educational sessions should be conducted to strengthen capacity building, and adequate healthcare information awareness should be given to the patient. These sessions could improve awareness and readiness among pharmacists on early-onset dementia while equipping them with the right skills, knowledge, and tools necessary to tackle this challenging condition.
Synthesis of Findings
Effectiveness of Pharmacist Interventions
Many studies, such as those conducted by Grossi et al. (2019) and Levine et al., 2021 have also shown how using pharmacist-led intervention can result in considerable improvements in medication management and adherence amounts that, combined with a reduction in dementia progression improvement might also be related there to the level of patient’s quality life Research by Grossi et al. (2019) was a U.K. cohort study aimed at determining the relationship between anticholinergic and benzodiazepine medication use, on dementia incidence risk in case of their usage within 5–8 years after that (Grossi et al., 2019) They saw that the use of anticholinergics with high activity in an inverse relationship tended to increase the risk of dementia, especially for anti-depressants drugs; and above all anti-Parkinsonian’s drug as well as urological.1 Additionally, ‘it would lead to an increase in dementia development no matter the duration from which using benzodiazepines (Grossi et al., 2019). They recommended consuming these medications with care and attention, especially for elderly patients, all subject to alternatives.
Among older adults followed by a home-based care team, Levine et al. (2021) examined the consequences of pharmacist identification and management of scarce drug treatment to medication therapy problems involving cognition. In searching for MTDs, pharmacists identified as many as 153 medication therapy problems among older people yet involving cognition; overall reported of such utilization, this figure was estimated at approximately one-fourth (42%), disregarding all types either confirmed or not. They also discovered that the home-based care team resolved 74 % of the medication therapy problems, improving medication adherence, lowering Medication burdens, and patient satisfaction. They argued that pharmacists are crucial to medication management optimization and how they help mitigate some cognitive problems within the community among older. Other benefits of pharmacist interventions are psychological, quality of life and positive affect outcomes for demented patients and their caregivers. A systematic review conducted by Lussier et al. (2020) showed that the involvement of community pharmacists in care transitions for people with dementia can lead to reduced readmission rates, emergency department visits, and medication-related errors (Lussier et al., 2020).
In their qualitative study, Barry et al. (2020) explored the perceptions and experiences of primary healthcare employees regarding medicines management among people with dementia and the theory-informed intervention needed for a better approach based on how they feel about this allocation. They have created an empiric model by developing several modifications depending on input from experts heard during. The intervention consisted of a pharmacist-led medication review and consultation service for patients with dementia and those who care for them. It was made available online as an example video directing attention to essential behaviors using corrective feedback. This intervention, according to Maidment et al. (2017), can allow more awareness and understanding of dementia as well as pharmacotherapy by both healthcare personnel and carers; it also facilitates a patient-centered team approach in medicine management (Maidment et al., 2017). These researches prove that pharmacist-led interventions bring positive effects on early dementia identification and dealing with medication concerns associated with it. They also underline the importance of multi-disciplinary cooperation and patient-centred treatment in dementia prevention and management.
Impact of Deprescribing Anticholinergic Medication
The research by Gannon et al. (2021) and Gray et al. (2015) points out the critical role of deprescribing anticholinergic medications in preventing dementia and improving patient outcomes. They underline the significant contribution pharmacists can have in detecting and treating patient medication schedules to lessen exposure to anticholinergics with their cumulative impact on cognition. This method enforces the need for a proactive strategy in healthcare to minimize the risk of dementia through proper medication management. (Gannon et al., 2021; Gray et al., 2015)
Pharmacists’ Role and Awareness:
As was shown in the findings presented by Shoji et al. (2023) and Bentley Garth Oswald, their work backs up the critical role pharmacists play during the early detection of dementia but, at the same time, lack awareness together with special training concerning dementia care particulars. Shoji et al. (2023) surveyed 1,00 people – community pharmacists in Japan to examine their dementia knowledge practices and attitudes toward providing care for individuals with this condition [1]. The knowledge level of pharmacists on D.M. appeared to be moderate, and they had a positive attitude toward dementia; however, their confidence and satisfaction regarding caring for dementia seemed low (Shoji et al., 2021). They also identified that pharmacists participating in the program whose training was specific to dementia or who were more experienced with patients with this condition showed more excellent knowledge and satisfaction scores (Shoji et al., 2021). They recommended that pharmacists require better education and support in order to develop their dementia care abilities further.
Oswald (2017) reviewed the impact of community pharmacy and optimization practice for individuals with dementia using medicines as medicine Optimiser in the U.K. He presented the issues and opportunities for pharmacists to deliver patient-centered care to dementia patients, involving medication reviews, identifying and resolving medication-related problems, and supplying information on improving adherence concordance (Oswald, 2017). He also emphasized teamwork, effectively communicating with other healthcare and social workers to come into close contact with patients or carers, and establishing continuous training opportunities for pharmacists and their assistants. Tarhan and Arslan (2023) reveal that pharmacists play a critical role in the early diagnosis and monitoring of dementia. However, there are a few associated barriers and gaps in knowledge (Tarhan and Arslan, 2023). They further highlight the role of pharmacists in multi-disciplinary holistic care among people with dementia and their family members. The effects and economic value of pharmacist-focused interventions in dementia care programs must be further explored so that the best approaches for implementing and sustaining them can also be considered.
Educational and Training Needs
While pointing out a gap in pharmacy education about dementia care, Blagburn (2017) calls for more inclusive training programs to prepare future standards to be recognized as identifiers and managers of new cases. In their case, Dillon et al. (2017) outlined dementia characteristics that interfere with medication management and decision-making ability, as well as behavioral modifications required from the pharmaceutist to offer patient-centered care will be discussed at length by addressing behavior change in health professionals working alongside adjustments needed language employability of healthcare workers aimed at establishing clinically viably In addition; he provided data on the related risks of anticholinergic drugs especially antipsychotics among dementia patients. In this case, he proposed a guide for medication review – a challenging clinical situation (Dillon et al., 2017).
The Pharmaceutical Care of People with Dementia is an online educational package developed by NHS Education for Scotland to address the education and training needs of pharmacists and home-care supervising role from Phase 1: assessment involving progression goals such as telephone skills dialogue between staff and patient or carer noted communication assessments. The bundle includes subtype dementia, risk factors and early signs, assessment process screening diagnosis, pharmacological resistance, non-pharmaceutical intervention, ethical and legal issues, and end-of-life care.
Dementia Friendly Pharmacy is a web-based course by Dementia Training Australia designed to ensure that community pharmacists and their assistants gain knowledge in delivering quality products, services, or information for people who are living with dementia as well as caring for residents (DTA, 2019). Among the topics dealt with in this course are community pharmacy contribution to supporting family carers of people living with dementia, guidelines for a supportive and dignified environment by adopting practices that make them friendly as well as becoming friendly facilities, prescribing roles, properly using medications commonly used when supporting patients diagnosed dementia. (DTA 2019).
The module of continuing education Module, Role of the Pharmacist in the Care of Persons Living with Dementia, was developed by the Department of Health and Human Services U.S. to provide an overview of dementia, its causes, symptoms, diagnosis, and treatment as well as how this role works for pharmacists caring for a person who has deminat5. It outlines pharmacological and non-pharmacological management of dementia, medication therapy monitoring, communication strategies, ethical concerns, and legal issues. The evidence that these sources provide is the increase in acknowledgment for pharmacy education and training about dementia care alongside active resources as well as programs available on improving knowledge and practice. Nevertheless, further research is required for the assessment of the efficacy and influence of such educational interventions on care quality and results in dementia patients as well as their carers.
Challenges in Dementia Care
Barriers to effective pharmacist involvement in dementia care included diagnostic challenges, particularly in early-onset cases, as discussed by Nwadiugwu (2021), and the complexity of managing polypharmacy in dementia patients, as noted by Reeve et al. (2015). EOD presents a set of diagnostic, interventionist, and supportive care challenges in that many patients work full-time or have young children; moreover, their forms of dementia deviate from typical old age ones. Pharmacists, as representatives of a multi-disciplinary healthcare team, can contribute to detecting and treating EOD through screening, referral for in-depth evaluation if necessary, and education regarding medications consumed by elderly subjects, among others. Nevertheless, several bottlenecks restrict the pharmacist’s participation in EOD management, including lack of awareness and recognition regarding symptoms for early onset dementia as well intervention difficulties, including medication regimens that have complexity or variability; communication is also an issue with other healthcare providers and clients a deficient training program along with resources targeted to solutions concerning pharmacy services incredibly pert.
The timely and accurate diagnosis of dementia is always one of the core challenges faced during any care service provision efforts done with such a mindset. One of the key issues discussed by Nwadiugwu (2020) regarding early-onset dementia is its low recognition and awareness, denial, and stigma associated with this condition, lack of access to specialist services as well as work and family customs after all that challenges such situation brings along. Davies et al. (2023) further proposed a person-centered care model that includes the individual, family members, and all health social workers -parents in an elaborate symbiotic relationship (Davies et al., 2023).
Polypharmacy, the simultaneous use of several medications in dementia patients with multiple comorbidities and cognitive impairments, is also a challenge to manage (Cox et al., 2016). However, polypharmacy increases the likelihood of adverse drug reactions and interactions, medication errors as well and non-adherence while at the same time negatively influencing quality of life. A network analysis of a systematic review done by Reeve et al. (2015) shows that deprescribing is the process of reducing or stopping inappropriate and unnecessary medications, which can also be shown below: Research reported that deprescription includes a holistic assessment of an individual’s use of medications, identification of suboptimal medicinals listed in the Beers criteria and compromise decisions with the person or their caregiver (Reeve et al., 2015). They also identified the necessity of further studies and advice for using deprescribing in practice, even more so with dementia patients.
Summary of Key Findings
The significance of multi-disciplinary healthcare approaches lies in the fact that pharmacists could be a significant part of early-onset dementia identification and management. As they are available and interact with the community regularly, pharmacists could be introduced to crucial players in the early detection of cognitive impairment. They can use quick, validated screening tools that can spot people who may be predisposed to dementia and, with early treatment hence, direct them to specialist care. This method not only increases the probability of early detection but also reduces access inequality in healthcare, such that more people can get their needed care as quickly as possible.
Medication management involving pharmacists is critical in that they, among many other reasons, address polypharmacy issues affecting the elderly, who are easily subjected to such problems. They can measure, improve, and control cumbersome drug regimens to remedy undesirable effects as well as the pathway of unwelcome medication interaction; that is one vital aspect in treating what could be the most common senile ailment. Pharmacists’ contribution in administering appropriate drugs also delays the progression of these types, if not to specific diseases, leading to at least better or even less frightening outcomes related to patient treatment. Their roles go far beyond just monitoring drug consumption and introducing patients and family members to appropriate strategies for disease management or treatment conduct. Through such practices, they help alleviate the dementia nursing care burden on people with dementia and their relatives.
Moreover, Pharmacists provide supportive and informative roles; one can ask patients or their families about dementia counseling. This includes provisions of counseling which entail guiding modification in lifestyles that can retard the progression of this disease and teaching implications of different medications. Their position makes them intermediaries; they connect patients straining for help to more health resources. This integrative patient care model enables us to deliver much more than a carer can provide since dementia patients need so much emotional support.
Maintaining a constant watch and monitoring of the subjects who presented first-onset dementia is required of pharmacists. Such repeated engagements allow pharmacists to assess changes that come with a patient’s cognitive function and medication adherence; continuous surveillance is also possible alongside the adjustment for treatment plan modification aside from other healthcare professionals who would manage patients concerning their illness. Apart from this, including pharmacists in research and interprofessional collaboration reforms generalized knowledge about dementia treatment, resulting in more efficient measures.
Employing pharmacists for dementia management is beneficial but also not easy. Additional pharmacist education is needed in dementia care pathways, such as screening tools and knowledge of the atypical approach to dementia (Blagburn, 2017). The regulatory and scope of practice barriers may become a poor implementation barrier. Policy changes may also follow the application of pharmacist knowledge. Nevertheless, overcoming these barriers is essential for the successful partnership between healthcare providers and to provide the proper care that patients deserve, personalized, coordinated, and fully integrated.
Including pharmacists in formulation care teams for people with early-onset dementia will likely result in significant quality enhancement and accessibility development. In early detection, medication management, patient education, and follow-ups, pharmacists should be placed in an active role to maximize the available potential within the community. With proper training and application of dementia care policies, this revolutionary approach to managing the condition can be put on firmer ground, which will not negatively impact family caress caregivers.
Conclusion and Recommendations
Conclusion
This systematic review has allowed for a critical evaluation of the potential to include pharmacists in detecting and managing early-onset dementia, thereby bringing to light an opportunity that is promising but underused within healthcare systems. Our evidence highlights the crucial role of pharmacists in early detection and medication management, providing a singular platform to intervene at this stage. However, despite all the potential evidence from various studies that formed our review subjects, pharmacists needed more training and awareness of the discrepancies between different healthcare settings. The evidence implies that pharmacists establish quite a lot in the care of dementia patients by enhancing their medication regimen, deprescribing potentially inappropriate medicinal products, and educating patients about medications. It results not only in improving patient outcomes but also in decreasing the burden on family member-caregivers or other ‘unpaid’ standards for staff. Nevertheless, realizing this potential is made less effective by a deficit in dementia-specific training and unclear guidelines on pharmacists` role in dementia diagnosis and management. In addition, the studies that make up this review have a series of limitations characteristic of observational and qualitative research; for instance, they need careful interpretation of their results.
Recommendations
From the analysis of synthesis evidence in this review, several recommendations for strengthening the scope and impact role pharmacists play in dementia care are proposed. Primarily under review, the issue to be addressed is that there is a pressing demand for implementing profound training programs concerning dementia care that are directed at pharmacists. Such programs should cover early diagnosis, medication management, and effective patient and caregiver communication strategies. Second, healthcare policies need to be updated so that pharmacists are formally included in multi-disciplinary dementia care teams, hence recognizing their contribution to patient management. The integration implies the establishment of transparent patient guidelines and protocols that clearly define pharmacist roles in dementia care. Third, more research is suggested to solve these gaps in the literature, especially well-sized epidemiological studies, which serve more robust segments of evidence about pharmacists’ Work on Dementia Care. Such research should strive to determine the net benefits of pharmacist interventions on patient outcomes, medication safety, and healthcare utilization.
Study Limitations
The main limitation is related to the heterogeneity of the studies included in this metanalysis, as they differ in research designs and populations, rendering it challenging to derive synthesized findings with synthesizing generalizability. Furthermore, the process for risk of bias comparison focused on some issues regarding methodological quality, especially in the case of observational studies or qualitative research, which may affect reliability from the evidence base. The second limitation is the use of English language publications, which could have resulted in missing documents published in non-English languages. In addition, most of these were conducted in high-income countries, questioning their values in low, middle-income settings. Finally, the review did not systematically evaluate the economic effects associated with pharmacist engagement in dementia management, an aspect that deserves future study.
Future Directions
Based on the limitations and findings of this review, future studies should address gaps in evidence by doing well-organized multicenter research, which will help us determine efficacy interventions by pharmacists across varied healthcare settings among different populations. Studies assessing the economic burden of including pharmacists in dementia care teams, especially cost-effectiveness analyses, are also needed. Furthermore, it would be interesting to determine what obstacles and even facilitators novel changes in pharmacy education and healthcare policy implementation involve since a total contribution of the profession to early-onset dementia patients’ care depends on translation from theory into practice.
Reference list
Arvanitakis, Z., Shah, R.C. and Bennett, D.A. (2019). Diagnosis and Management of Dementia: Review. JAMA, [online] 322(16), pp.1589–1599. Doi:https://doi.org/10.1001/jama.2019.4782.
Barry, H.E., Bedford, L.E., McGrattan, M., Ryan, C., Passmore, A.P., Robinson, A.L., Molloy, G.J., Darcy, C.M., Buchanan, H. and Hughes, C.M. (2020). Improving medicines management for people with dementia in primary care: a qualitative study of healthcare professionals to develop a theory-informed intervention. BMC Health Services Research, 20(1). doi:https://doi.org/10.1186/s12913-020-4971-7.
Blackburn, J. (2017). How pharmacy can provide patient-centered care for dementia patients. [online] The Pharmaceutical Journal. Available at: https://pharmaceutical-journal.com/article/ld/how-pharmacy-can-provide-patient-centred-care-for-dementia-patients.
Candy, B., Elliott, M., Moore, K., Vickerstaff, V., Sampson, E. and Jones, L. (2015). UK quality statements on end of life care in dementia: a systematic review of research evidence. BMC Palliative Care, 14(1). doi:https://doi.org/10.1186/s12904-015-0047-6.
Cox, M., Cuff, P., Brandt, B., Reeves, S. and Zierler, B. (2016). Measuring the impact of interprofessional education on collaborative practice and patient outcomes. Journal of Interprofessional Care, 30(1), pp.1–3. doi https://doi.org/10.3109/13561820.2015.1111052.
Davies, N., Kolodin, V., Woodward, A., Bhanu, C., Jani, Y., Manthorpe, J., Orlu, M., Samsi, K., Burnand, A., Vickerstaff, V., West, E., Wilcock, J. and Rait, G. (2023). Models of care and the role of clinical pharmacists in UK primary care for older adults: A scoping review protocol. PloS One, [online] 18(7), p.e0276471. Doi:https://doi.org/10.1371/journal.pone.0276471.
Dementia Training Australia (2019). Dementia Friendly Pharmacy, Online dementia courses, DTA. [online] DTA. Available at: https://dta.com.au/online-courses/dementia-friendly-pharmacy/.
Dillon, A.R., Blagburn, B.L., Tillson, M., Brawner, W., Welles, B., Johnson, C., Cattley, R., Rynders, P. and Barney, S. (2017). Heartworm-associated respiratory disease (HARD) induced by immature adult Dirofilaria immitis in cats. Parasites & Vectors, 10(S2). doi:https://doi.org/10.1186/s13071-017-2452-6.
Gannon, J.M., Lupu, A., Brar, J., Brandt, M., Zawacki, S., John, S., Carl, K. and Chengappa, K.N.Roy. (2021). Deprescribing anticholinergic medication in the community mental health setting: A quality improvement initiative. Research in Social and Administrative Pharmacy, 17(10), pp.1841–1846. doi:https://doi.org/10.1016/j.sapharm.2020.12.010.
Gray, S.L., Anderson, M.L., Dublin, S., Hanlon, J.T., Hubbard, R., Walker, R., Yu, O., Crane, P.K. and Larson, E.B. (2015). Cumulative Use of Strong Anticholinergics and Incident Dementia: A Prospective Cohort Study. JAMA Internal Medicine, 175(3), pp.401–7. doi:https://doi.org/10.1001/jamainternmed.2014.7663.
Grossi, C.M., Richardson, K., Fox, C., Maidment, I., Steel, N., Loke, Y.K., Arthur, A., Myint, P.K., Campbell, N., Boustani, M., Robinson, L., Brayne, C., Matthews, F.E. and Savva, G.M. (2019). Anticholinergic and benzodiazepine medication use and risk of incident dementia: a UK cohort study. BMC Geriatrics, 19(1). doi:https://doi.org/10.1186/s12877-019-1280-2.
Levine, A., Emonds, E.E., Smith, M.L., Rickles, N.M., Kuchel, G.A., Steffens, D.C., Alis Ohlheiser and Fortinsky, R.H. (2021). Pharmacist Identification of Medication Therapy Problems Involving Cognition Among Older Adults Followed by a Home-Based Care Team. 38(2), pp.157–168. doi:https://doi.org/10.1007/s40266-020-00821-7.
Lussier, M.E., Evans, H.J., Wright, E.A. and Gionfriddo, M.R. (2020). The impact of community pharmacist involvement on care transitions: A systematic review and meta-analysis. Journal of the American Pharmacists Association, 60(1), pp.153-162.e5. Doi:https://doi.org/10.1016/j.japh.2019.07.002.
Maidment, I.D., Aston, L., Moutela, T., Fox, C.G. and Hilton, A. (2017). A qualitative study exploring medication management in people with dementia living in the community and the potential role of the community pharmacist. Health Expectations, 20(5), pp.929–942. doi:https://doi.org/10.1111/hex.12534.
McGuinness, L.A., Warren‐Gash, C., Moorhouse, L.R. and Thomas, S.L. (2019). The validity of dementia diagnoses in routinely collected electronic health records in the United Kingdom: A systematic review. Pharmacoepidemiology and Drug Safety, 28(2), pp.244–255. doi:https://doi.org/10.1002/pds.4669.
NHS (2018). Palliative Care Guidelines In Dementia 2nd Edition North West Coast Strategic Clinical Network. [online] Available at: https://www.england.nhs.uk/north/wp-content/uploads/sites/5/2018/06/palliative-care-guidelines-in-dementia.pdf.
Nwadiugwu, M. (2020). Early-onset dementia: key issues using a relationship-centred care approach. Postgraduate Medical Journal, 97(1151), p.postgradmedj-2020-138517. Doi:https://doi.org/10.1136/postgradmedj-2020-138517.
O’Dwyer, M., Maidment, I.D., Bennett, K., Peklar, J., Mulryan, N., McCallion, P., McCarron, M. and Henman, M.C. (2016). Association of anticholinergic burden with adverse effects in
Older people with intellectual disabilities: an observational
cross-sectional study. British Journal of Psychiatry, 209(6), pp.504–510. doi https://doi.org/10.1192/bjp.bp.115.173971.
Oswald, K. (2017). Medicines optimization in dementia: the role of the community pharmacy. [online] The Pharmaceutical Journal. Available at: https://pharmaceutical-journal.com/article/feature/medicines-optimisation-in-dementia-the-role-of-the-community-pharmacy.
PRISMA (2020). PRISMA. [online] prisma-statement.org. Available at: http://prisma-statement.org/PRISMAStatement/FlowDiagram.
Rahman, Md.M., Kamal, M.A., Mim, S.A., Islam, Md.R., Parvez, A., Islam, F., Uddin, M.B., Rahaman, Md.S., Shuvo, P.A., Ahmed, M. and Greig, N.H. (2022). Exploring the Recent Trends in Management of Dementia and Frailty:
Focus on Diagnosis and Treatment. Current Medicinal Chemistry, 29(32), pp.5289–5314. doi https://doi.org/10.2174/0929867329666220408102051.
Reeve, E., Gnjidic, D., Long, J., and Hilmer, S. (2015). A systematic review of the emerging definition of ‘deprescribing’ with network analysis: implications for future research and clinical practice. British Journal of Clinical Pharmacology, [online] 80(6), pp.1254–68. doi:https://doi.org/10.1111/bcp.12732.
Shannon, K., Bail, K. and Neville, S. (2019). Dementia‐friendly community initiatives: An integrative review. Journal of Clinical Nursing, 28(11-12), pp.2035–2045. doi:https://doi.org/10.1111/jocn.14746.
Shoji, M., Cato, S., Iida, T., Ishida, K., Ito, A. and McElwain, K.M. (2021). Variations in Early-Stage Responses to Pandemics: Survey Evidence from the COVID-19 Pandemic in Japan. Economics of Disasters and Climate Change. Doi:https://doi.org/10.1007/s41885-021-00103-5.
Snyder, H. (2019). Literature Review as a Research methodology: an Overview and Guidelines. Journal of Business Research, 104(1), pp.333–339. doi:https://doi.org/10.1016/j.jbusres.2019.07.039.
Suwa, S., Tsujimura, M., Yumoto, A., Iwata, N. and Shimamura, A. (2021). Multidisciplinary pharmacotherapy collaboration for home‐based older adults with dementia: a study focusing on physicians, pharmacists, and nursing professionals. Psychogeriatrics, 21(5), pp.749–762. doi:https://doi.org/10.1111/psyg.12735.
Tarhan, N. and Arslan, M. (2023). Psychometric assessment of pharmacists’ counseling in dementia. Patient Education and Counseling, [online] 115, p.107903. doi:https://doi.org/10.1016/j.pec.2023.107903.
Thijssen, M., Daniels, R., Lexis, M., Jansen, R., Peeters, J., Chadborn, N., Nijhuis‐van der Sanden, M.W.G., Kuijer‐Siebelink, W. and Graff, M. (2021). How do community-based dementia-friendly initiatives work for people with dementia and their caregivers, and why? A rapid realist review. International Journal of Geriatric Psychiatry, 37(2). doi:https://doi.org/10.1002/gps.5662.
Tran, Q. (2022). Worldwide dementia cases will triple by 2050 to over 150 million people. [online] Alzheimer’s Research UK. Available at: https://www.alzheimersresearchuk.org/worldwide-dementia-cases-to-triple-by-2050-to-over-150-million/.
Wang, N. and Brooke, J. (2020). The experience of children with parents diagnosed with young onset dementia: a systematic literature review. British Journal of Neuroscience Nursing, 16(4), pp.165–173. doi https://doi.org/10.12968/bjnn.2020.16.4.165.
Yates, J., Stanyon, M., Samra, R., and Clare, L. (2021). Challenges in disclosing and receiving a diagnosis of dementia: a systematic review of practice from the perspectives of people with dementia, carers, and healthcare professionals. International Psychogeriatrics, pp.1–32. doi:https://doi.org/10.1017/s1041610221000119.
 write
write