BACKGROUND
In this case study, we have a 38-year-old hospitalized man who has a case of severe hyponatremia. The cause, as outlined, is surreptitious water intoxication. This man has a reported but not confirmed history of Gitelman’s syndrome, hypertension, and diabetes that has been presented to Urgent Care(Claudel et al., 2022). The symptoms experienced include leg pain, dizziness, headache, and, upon testing, a serum sodium concentration [SNa] of 114 mmol/L, as per Claudel et al. (2022). This case of severe hyponatremia is a complicated one due to the unconfirmed diseases. The patient has shown a history of Gitelman’s syndrome, hypertension, and diabetes. Additionally, there were renal abnormalities seen in the laboratory that showed impaired renal concentrating ability that the suspected Gitelman syndrome could have brought.
Hyponatremia is a common electrolyte abnormality that occurs when sodium concentration in the blood is low(Gankam Kengne & Decaux, 2018). Sodium plays a vital role in regulating the amount of water within and outside body cells. Severe Hyponatremia, therefore, is serum sodium (Na) that is less than 135mmol/L, but this could vary from one laboratory to another(V et al., 2018). The balance between the total water body and total sodium concentration needs to maintain a certain equilibrium for the body to work effectively. Hyponatremia happens when the entire water body exceeds the total body sodium. This condition is common among the elderly, where age and medication are vital contributors to the condition. In the clinical field, its presentation ranges from asymptomatic to life-threatening neurological symptoms. This is dependent upon the time intervals of the reduced sodium level and the brain’s capacity to handle transcellular osmotic balances(Roumelioti et al., 2018). Its manifestations increase with an increased rate of change.
The total body water is made up of two compartments, namely, extracellular fluid (ECF) and intracellular fluid (ICF). The ECF exists outside cells and makes up about one-third of the total water body, while the ICF makes up the remaining two-thirds of the whole body of water(Neligan, 2024). The ICF’s major solute is potassium, while sodium is the major solute for the ECF. Diagnosing hyponatremia is done by measuring the serum osmolality as the first step to confirm hypotonicity, which is then followed by measuring urine and sodium to help differentiate between anti-diuretic hormone (ADH)-dependent and independent hyponatremia (Seay et al., 2020). Symptoms vary from one patient to another but are dependent on the severity and duration of hyponatremia. Severe hyponatremia symptoms include fatigue, anorexia, dizziness, and muscle cramps(Joiner, 2019). Other symptoms include headaches, nausea, vomiting, seizures, and even a coma. This medical condition is complex, and it can be quite challenging to disentangle the various causes, more so for hospitalized cases.
Gitelman’s syndrome, experienced by the patient, is a rare inherited disorder that affects the kidney’s ability to reabsorb some electrolytes, which results in low levels of potassium and magnesium in the blood. The syndrome contributes to the patient’s electrolyte imbalances, which affect response to hyponatremia correction strategies(Adrogué & Madias, 2012). The basic background of Gitelman’s syndrome requires customization of the treatment decisions. The case needs answers about the aetiology of hyponatremia, the role that Gitelman’s syndrome has played, and the management strategies that have been put in place to correct the situation.
CLINICAL FINDINGS
The first test showed a very low serum sodium concentration of 114 mmol/L. As a result, the patient had to be transferred to the emergency department for further evaluation and management. In the emergency department, the man’s blood pressure was measured, and it was 93/63 mmHg. More laboratory tests four hours later showed an increase in [SNa] to 121 mmol/L. The serum osmolality tests measured were at 248 mOsm/kg H2O, urine osmolality at 61 mOsm/kg H2O, and urine sodium < 20 mmol/L (Claudel et al., 2022). These results showed an irregular response to hyponatremia, raising a possible alarm about an underlying kidney dysfunction. To deal with the low blood pressure, the patient was given 1L of normal saline, which led to a quick increase in [SNa] to 127 mmol/L (Claudel et al., 2022). Other medical interventions included the administration of 2.5 litres of dextrose-containing water after he was admitted. The aim was to correct the sodium levels while dealing with the patient’s symptoms. This was then followed by continuous monitoring of glucose levels due to the dextrose infusion, ensuring the patient was safe during interventions. Nephrology was consulted for further management of this case. This emphasizes the need to have experts from different departments address the electrolyte imbalance and possible renal abnormalities (Gitelman’s syndrome in this case).

Blue: average serum sodium per hospital day, orange dots: Lowest serum sodium, grey dots: maximum serum sodium, Arrow-Day 17 when the restroom faucet was turned off.
PATHOPHYSIOLOGY
The pathophysiology of hyponatremia is abnormal changes in the regulation of water balance, which result in excess water when compared to sodium(Buffington & Abreo, 2015). Hyponatremia is caused by excessive water intake, which may lead to dilutional hyponatremia. It is also caused by loss of sodium and impaired renal water excretion due to conditions such as kidney dysfunction and hypovolemic states, which trigger the body to retain water, leading to a decrease in serum sodium concentration (National Kidney Foundation, 2024). Diuretics, too, can lead to an increase in sodium that can be excreted in urine, causing sodium loss. Another major cause is chronic drinking, which leads to more urination, hence the loss of more body fluid. Hyponatremia can happen to anyone, but it is more likely to happen to people with kidney problems, heart failure, lung, liver, and brain diseases, and people who have had surgery(Kheetan et al., 2021). The condition is also prevalent in people who have taken diuretics or antidepressants. This condition is the most common chemical abnormality experienced by hospitalized patients.
A patient with hyponatremia experiences neurologic symptoms that range from confusion to seizures to coma. When the sodium levels fall gradually, the symptoms are only mild, but when the symptoms get more serious, the sodium in the blood falls quickly. Other signs and symptoms of severe hyponatremia include muscle cramps or weakness, nausea and vomiting, headaches, and lethargy (Joiner, 2019). The disease also causes mental status changes as it has detrimental effects on the brain. To diagnose hyponatremia, the doctor will measure the sodium, potassium, and creatine concentrations in the urine. This will also include blood tests to ascertain total body water, sodium levels, and levels of hormones that regulate water uptake by the kidney(Cleveland Clinic Medical, 2024). The medical provider will also have to take note of the medical history of the patient, followed up by a physical examination, and this will help determine the sodium levels in the blood.
Since our case is complex due to underlying problems, there are a series of activities required to return the osmotic balance to equilibrium. To maintain serum sodium and osmolality, there is thirst stimulation, secretion of anti-diuretic hormone, and kidney processing of the filtered sodium. Normally, the plasma osmolality lies between 275 and 290 mOsm/kg. To maintain the required equilibrium of osmolality, water intake should be equivalent to water excretion. If not held at the appropriate equilibrium levels, hyponatremia will occur. To regulate the water intake, the thirst mechanism is employed, and as a result, the osmoreceptors present in the hypothalamus trigger thirst when the body osmolality attains 295 mOsm/kg(V et al., 2018). This also causes the posterior pituitary to secrete the anti-diuretic hormone vasopressin.
The ADH helps in the regulation of water secretion. ADH is produced in the hypothalamus and stored in the posterior pituitary gland. In some cases, baroreceptors present in the carotid sinus may trigger the secretion of ADH, but their effectiveness and sensitivity are lower than those of the osmoreceptors(Schrier, 2006). They trigger ADH secretion as a result of reduced effective circulation volume, stress, nausea from drugs, and pain. The anti-diuretic hormone works on the V2 receptors located on the basolateral aspect that collect duct cells, thereby boosting aquaporin expression on the luminal aspect of managing duct cells, inducing water absorption, and eliminating thirst.
Hyponatremia occurs in 3 major ways: hypervolemia, euvolemia, and hypovolemia.
- Hypervolemia: Hypervolemia occurs when more fluid is taken in than is excreted. Water take-in can be in terms of intravenous, transurethral, transrectal, transcervical or even through oral ingestion. When the water is taken in beyond the physiological requirements, it dilutes the sodium ions. The excess fluid can be excreted through urination, with the kidney excretion rates ranging from 778 to 1043 mL in an hour when arginine vasopressin (AVP) and ADH are suppressed(Weisz & Hew-Butler, 2016).
- Euvolemia: Euvolemia is the state of having normal body fluids in the body. Sometimes, water is abnormally retained by the body, which dilutes sodium levels. This condition accounts for 60% of the total cases of hyponatremia, making it the most common (Sivakumar et al., 2021). The inappropriate ADH and AVP secretion causes the body to retain water abnormally. In this case, the maximum kidney excretion rates are between 778 and 1043 mL per hour when the hormones are suppressed. People resistant to the activities of ADH at the kidney or psychogenic polydipsia can still have normal natremia status because the kidney is required to excrete between 15 and 20 litres of fluid a day. Some non-osmotic factors can trigger ADH and AVP through vomiting, endurance exercises, and plasma volume reductions that result in water preservation (Krishnaiah et al., 2023). Some of these factors include pain, heat, and drugs such as antidepressants and antipsychotics. These factors retain the fluid by activating the release of ADH and AVP from the posterior pituitary gland. These non-osmotic factors result in abnormal water retention, hence dilutional hyponatremia. The resulting type of hyponatremia is commonly referred to as the Syndrome of Anti-diuretic Hormone Secretion (SIADH).
- Hypovolemia: Hypovolemia occurs when the amount of sodium lost from the body is greater than the replacements. As a result, plasma volume decreases, which activates both the ADH and the AVP and the renin-angiotensin-aldosterone system (RAAS). The RAAS hormone stimulates thirst, while the ADH and the AVP retain all the fluids supplied(Boemi & Luconi, 2018). The water retained, and the volume driven may, in some cases, help in the formation of the volume depletion hyponatremia. It is worth noting that the sodium concentration of diarrhoea and sweat is lower than that of blood. With more gastrointestinal or sweat sodium ion losses, there is more loss of water than that of sodium, which triggers Hyponatremia as a result of lack of water replacement.
BIOCHEMICAL LABORATORY INVESTIGATIONS
For the body to work efficiently, electrolytes play a massive role. They are usually electrically charged minerals in the body. Sodium works to maintain the balance between fluid and pH in the body. To analyze the biochemical laboratory tests, this paper will focus on the Serum Sodium concentration and Serum osmolality.
Serum Sodium Concentration
Serum sodium concentration refers to the amount of sodium relative to the volume of water in the blood(Ackerman, 1990). The sodium concentration in the body should range between 137 and 142 mEq/L. The initial measurement was 114 mmol/L, and after the administration of 1L of normal saline infusion, there was a rapid increase to 127 mmol/L (Claudel et al., 2022). The initial SNa shows Hyponatremia sh, owing to an imbalance between sodium and water levels. The rapid increase after saline infusion showed the patient’s responsiveness to sodium correction.
Principle: It uses an Ion Specific Electrode (ISE) that develops an electrical potential electromotive force that measures ions in a solution by utilizing the specific features of certain membrane materials. The measuring system comprises the ISE, a reference electrode, and electronic circuits that are used to measure and process EMF to determine the concentration of the ions. The potentiometry uses the diluted ISE method to estimate the concentration of sodium in biological fluids. It measures the electrolyte processes in solution to calculate the concentration of sodium ions. When the sample comes into contact with the electrode, sodium ions exchange ions in the hydrated outermost layer of the glass electrode. When the ion exchange occurs, a voltage change occurs at the face of the electrode. The potential follows the Nernst equation and allows the calculation of the sodium ions.
Serum Osmolality
It is a test that measures the amount of water in the blood in relation to the different solutes. The serum osmolality should be between 275 to 295mOsm/kg. The initial measurement was 248 mOsm/kg H2O. This indicated an abnormal concentration of solutes in the blood. Urine osmolality, on the other hand, measures the amount of solutes in the water of the urine, and it should range between 50-1200 mOsm/kg. The initial measurement was 61mOsm/kg H2O, and a low urine osmolality of less than 20 mmol/L supports the diagnosis of inappropriate water retention due to impaired renal function due to the kidney’s inability to retain water (Claudel et al., 2022).
Principle: It makes use of the freezing point depression osmometry technique, which states that an increased concentration of solute in a solution can cause a lowering of the freezing point. To get accurate osmometry results, the osmometer should be well calibrated.
The initial measurement of the blood pressure stood at 93/63 mmHg, showing the need to administer normal saline. The low urine osmolality, low urine sodium concentration, and abnormal serum osmolality indicated inappropriate water retention, possibly due to impaired renal function.
DIAGNOSIS
After examination, the recorded body temperature was 99 °F, while the blood pressure was 100/58 mmHg. The pulse rate was at 97 bpm, and the oxygen saturation was at 94% in the surrounding air. Upon examination of the serum, the results showed that the patient’s sodium level was below the required range of 135–145 mmol/L before admission. A test at the urgent care unit showed a decrease from the normal range, indicating the presence of hyponatremia. The serum osmolality recorded was 248 mOsm/kg H20, which showed the presence of hypotonic hyponatremia (Claudel et al., 2022). A 24-hour urine test was done to show fluid restriction adherence as well as urinary electrolytes, and the urine osmolality was at 61 mOsm/kg and urine sodium< 20 mmol/L, which showed evidence of primary polydipsia. The creatine clearance of the patient was 19 mL/min, showing proof that there was a problem with kidney failure.
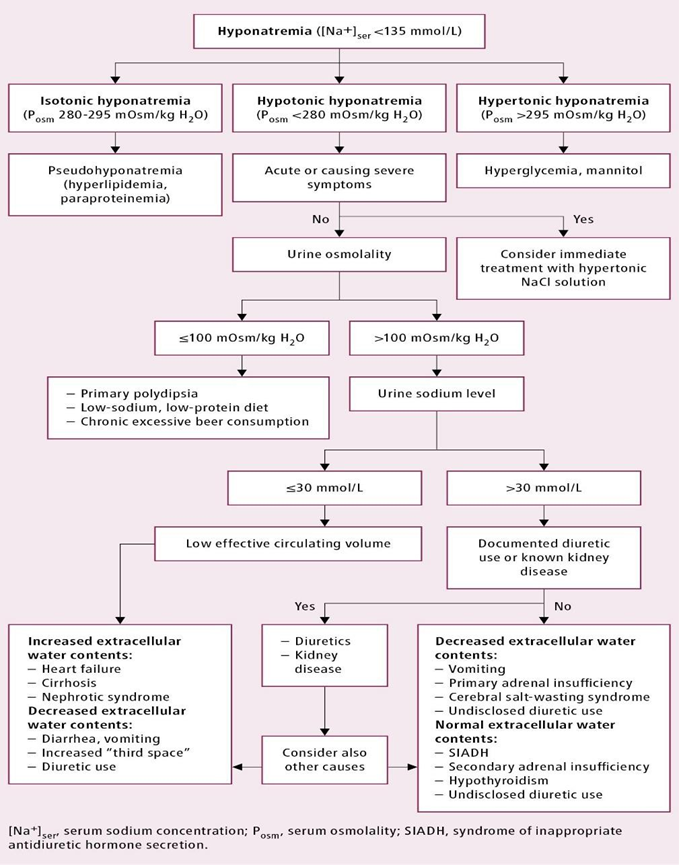
A Diagnostic Algorithm for Hyponatremia(McMaster University, 2022)
TREATMENT
The short-term treatment of Hyponatremia involves limiting the intake of water, treating the underlying diseases and stopping the intake of some medications. Long-term treatment methods include adding salt to the diet to increase the amount of sodium in the body. Our case is severe Hyponatremia and can not be solved by only one method (Cleveland Clinic Medical, 2024). Treating Hyponatremia for hospitalized patients requires interdepartmental interventions, more so if the patient has underlying diseases such as Diabetes, kidney disorders, hypertension and Gitelman’s Syndrome. It aims to prevent a further drop in sodium concentration, relieve the symptoms and lower intracranial pressure. Additionally, it can help in navigating the overcorrection of Hyponatremia in patients who have a high incidence of osmotic demyelination syndrome (ODS)(Anup & Vinod, 2013).
The first therapy aims to increase the concentration of serum sodium by 4 to 6 mEq/L within the first 24 hours. This should be achieved within the first six hours or less for patients showing symptoms, whether mild or severe. In the most severe cases, the highest correction rates should be 8 mEq/L within the first 24 hours (Adrogué & Madias, 2012). In our case, the patient was first taken into the emergency department and given 1L of normal saline as a measure to address low blood pressure and a possible case of hypovolemia. In response, there was an increase in SNa to 127 mmol/L, which indicated a need for a controlled mechanism to prevent overcorrection of hyponatremia. In addition, the patient was given 2.5 L of dextrose-containing water to reduce the imbalances in sodium. This solution is hypotonic and helps dilute the sodium in the blood and prevent a case of osmotic demyelination syndrome.
The patient had a case of Gitelman’s syndrome, and this was the major reason for using dextrose-containing water over other hypotonic solutions. The syndrome impairs the renal absorption of sodium, which can lead to hyponatremia. Most patients with hyponatremia are sensitive to small changes in sodium levels, making it necessary to use a hypotonic solution that will less likely lead to excessive sodium correction. In the treatment period, the treatment fluid was restricted to 1.2L per 24 hours, and amiloride was reinitiated; salt tablets (2g 3 times a day) were prescribed. Thyroid tests and cortisol levels were within normal ranges.
Monitoring
The serum sodium concentration was measured hourly with a keen eye on the symptoms to ascertain whether further therapy was needed. The frequency of monitoring can be reduced after the administration of 4 to 6 mEq/L of sodium serum (Ganguli & Veis, 2017). Examination of the urine output was observed with a focus on urine sodium, urine osmolality, and urine potassium. The correction rate may have to increase if there is a rise in urine output and a decrease in urine cation concentration. In such cases, it would be wise to measure serum sodium more frequently.
Fluid Restriction
In this case, the recommendation was to ensure the urine output was higher than the fluid intake. This achieves the goal of a negative water balance; the fluid levels should be 50–60% of the daily body requirements. For an increase in plasma osmolality to occur, there will be a controlled restriction of fluid. Sodium should not be restricted at this stage.
Amiloride reinitiation
Amiloride is a diuretic that helps the body avoid losing too much potassium. It works by reducing the amount of water in the body by triggering more urine flow, thereby reducing blood pressure. The drug also inhibits the reabsorption of sodium. Providing potassium can increase the serum sodium concentration and osmolality in patients with hyponatremia. Amiloride is preferred for cases of Gitelman’s syndrome as it has a potassium-sparing effect when compared to other water pills (Nuñez-Gonzalez et al., 2021). If used, loop diuretics can worsen hypokalemia, which is an issue in our case.
Oral Salt Tablets
Oral salt tablets are a good treatment prescription for patients with serum sodium levels above 120 mEq/L. They can be adopted together with fluid restriction in our case. In non-emergency cases, these tablets can be administered hourly instead of hypertonic saline. Consuming more sodium helps recover the lost electrolytes and maintain the required levels of serum sodium. Oral salt tablets are preferred and sustainable for chronic hyponatremia when compared to intravenous saline, which is preferable for mild cases (Calvo Latorre et al., 2022).
Prognosis
The severity and the underlying disease determine the possible cause of hyponatremia. In our case, the SNa ranged from 123 to 128 mmol/L for three days, even though the patient was on strict water and salt medication. The expectation is that if the current treatment plan of amiloride, fluid restriction, and salt tablets is adhered to, the patient’s sodium level is expected to stabilize within the normal ranges. Other underlying diseases, such as hypertension and diabetes, make the case complicated and must be managed alongside hyponatremia to improve the patient’s health.
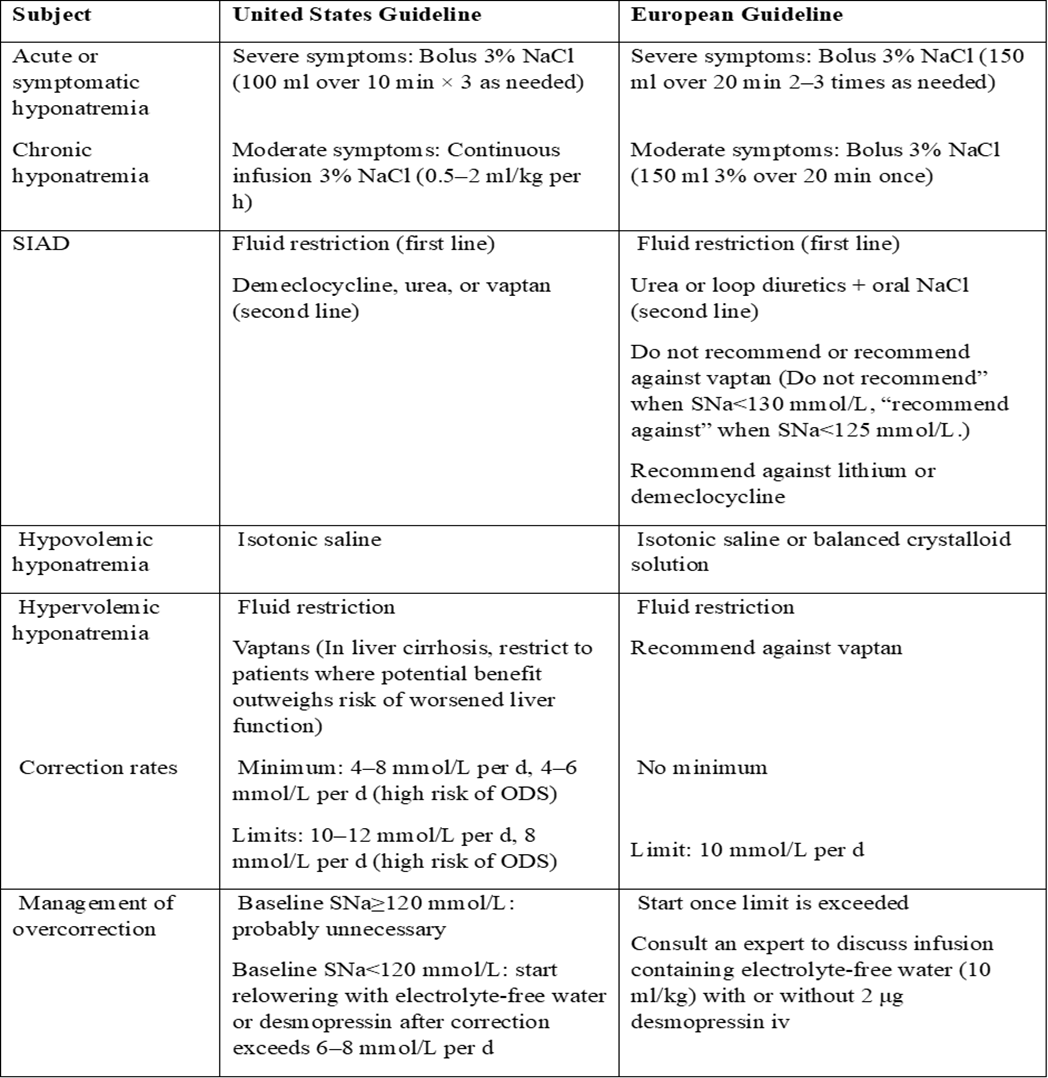
Recommended Treatment for United States and European Countries
DISCUSSION
Our case entails a 38-year-old man with a severe case of hyponatremia. Hyponatremia is a case of a serum sodium concentration that is below 135 mEq/L. This disorder is very common, as it is present in 30%–42% of hospitalized cases. Sodium plays a major role in the metabolic and biochemical processes of the body, as it helps in the transportation of water throughout the body. Sodium is a major component of the extracellular fluid (Strazzullo & Leclercq, 2014). Potassium, on the other hand, is a major solute for intracellular fluid, and it helps pump the byproducts of cellular activities out of the cell. This helps eliminate waste from the body. Sodium helps maintain the required amount of water, the osmotic equilibrium, the body pH balance, and the plasma volume. In addition, it helps regulate nerve impulses and the body’s muscle contractions.
Hyponatremia can be characterized based on the extracellular fluid levels. It can be identified as hypervolemic, euvolemic, or hypovolemic, depending on the volume of the fluid. In most cases, hyponatremia is caused by physiological signals that stimulate the production of vasopressin, which results in increased fluid production. The production of vasopressin results in physiological stimuli that include the loss of hypervolemic and hypovolemic hyponatremia. The release of vasopressin can be a result of adrenal insufficiency and hypothyroidism (Weisz & Hew-Butler, 2016). Women are generally more susceptible to hyponatremia as compared to men. Other risk factors include diabetes, cancer, heart failure, and liver failure.
True hyponatremia is characterized by low osmolality, meaning that the blood is more diluted than normal. To diagnose hyponatremia, the conditions that cause hypertonic hyponatremia are a result of active solutes such as glucose or mannitol, and isotonic hyponatremia is a result of an increase in plasma proteins, which should be distinguished. The first step to diagnosing hyponatremia is to check on the history of the patient and do an examination. This will then be followed by investigations whereby serum sodium is measured. The measurement can be done by ISE using direct potentiometry and serum osmolality, which is significant in distinguishing between true, pseudo, and translocational hyponatremia (Hamrahian, 2023). Another method is urine osmolality, which can help differentiate between impaired water secretion and hyponatremia, which has normal water excretion. Sodium in urine can be used to determine the source, whether it is renal or non-renal. Other methods to investigate include imaging of the chest and thyroid profile and the determination of the urine-to-serum ratio.
Limitation of Diagnosis
Measurement of errors: Inaccurate sodium measurements can happen in the laboratory due to poor calibration of the instruments, improper sample collection techniques and poor storage.
Pseudohyponatremia: This condition can hide true hyponatremia, which can lead to a false diagnosis. Some of these conditions include hyperlipidemia, hyperproteinemia, or multiple myeloma(Sosa, 2022). These conditions can increase osmolality falsely, thereby reducing calculated serum sodium.
Underlying aetiology: Some underlying diseases, such as heart failure and renal dysfunction, can increase the chances of hyponatremia. Only the serum sodium test is accurate, and beyond it, the other tests have to prove the precise aetiology of hyponatremia.
CONCLUSION
Hyponatremia is the most common chemicalabnormality, more so in hospitalized patients, which is a major challenge in diagnosis and management. In the complex case in this paper, a 38-year-old man has severe hyponatremia with a history of Gitelman’s syndrome, hypertension, and diabetes. Hyponatremia comes when there is a disruption of the water balance, resulting in more water as compared to sodium. The case needed a customized approach, as there was a case of Gitelman’s syndrome that inhibits the reabsorption of renal electrolytes. In this patient, interventions include a normal saline infusion and administering dextrose-containing water. To treat the condition, strategies such as fluid restriction, amiloride reinitiation, and oral salt tablets were employed. In conclusion, to effectively manage this condition, there must be a clear understanding of its pathophysiology and close monitoring coupled with individualized interventions to optimize the patient’s recovery.
Bibliography
Ackerman, G. (1990) ‘Clinical methods: The history, physical, and Laboratory Examinations’, Annals of Internal Medicine, 113(7), p. 563. doi:10.7326/0003-4819-113-7-563_2.
Adrogué, H.J. and Madias, N.E. (2012) ‘The challenge of Hyponatremia’, Journal of the American Society of Nephrology, 23(7), pp. 1140–1148. doi:10.1681/asn.2012020128.
Anup, P. and Vinod, M. (2013) . ‘neuromuscular blockade in the patient with neurologic disease’, Fundamentals of Neuroanesthesia, pp. 131–141. doi:10.1093/med/9780199755981.003.0010.
Boemi, M. and Luconi, M.P. (2018) ‘Water and sodium balance disorders in aging’, Trace Elements and Minerals in Health and Longevity, pp. 209–234. doi:10.1007/978-3-030-03742-0_8.
Buffington, M.A. and Abreo, K. (2015) ‘Hyponatremia’, Journal of Intensive Care Medicine, 31(4), pp. 223–236. doi:10.1177/0885066614566794.
Calvo Latorre, J., Senanayake, R. and Bashari, W.A. (2022) ‘Salt tablets safely increase serum sodium in hospitalized elderly patients with hyponatraemia secondary to refractory idiopathic syndrome of inappropriate anti-diuresis’, Cureus [Preprint]. doi:10.7759/cureus.24367.
Claudel, S.E., Waikar, S.S. and Verma, A. (2022) ‘Severe hyponatremia due to surreptitious water intoxication in a hospitalized patient’, CEN Case Reports, 12(2), pp. 135–138. doi:10.1007/s13730-022-00733-y.
Cleveland Clinic medical (2024) Hyponatremia: Causes, symptoms, diagnosis & treatment, Cleveland Clinic. Available at: https://my.clevelandclinic.org/health/diseases/17762-hyponatremia (Accessed: 22 February 2024).
Ganguli, A. and Veis, J. (2017) ‘Hyponatremia – a rare complication of Gitelman’s syndrome’, Indian Journal of Nephrology, 27(1), p. 74. doi:10.4103/0971-4065.177208.
Gankam Kengne, F. and Decaux, G. (2018) ‘Hyponatremia and the brain’, Kidney International Reports, 3(1), pp. 24–35. doi:10.1016/j.ekir.2017.08.015.
Hamrahian, S.M. (2023) Hyponatremia, Practice Essentials, Pathophysiology, Epidemiology. Available at: https://emedicine.medscape.com/article/242166-overview?form=fpf (Accessed: 22 February 2024).
Hyponatremia (low sodium level in the blood) (2024) National Kidney Foundation. Available at: https://www.kidney.org/atoz/content/hyponatremia# (Accessed: 21 February 2024).
Joiner, J.L. (2019) ‘Endocrine system’, AACN Core Curriculum for Pediatric High Acuity, Progressive, and Critical Care Nursing [Preprint]. doi:10.1891/9780826133038.0006.
Kheetan, M. et al. (2021) ‘Acute and chronic hyponatremia’, Frontiers in Medicine, 8. doi:10.3389/fmed.2021.693738.
Krishnaiah, M. et al. (2023) ‘A study on the disease pattern and outcome in Neonatal Intensive Care Unit, Tertiary Care Hospital of Andhra Pradesh’, Journal of Maternal and Child Health, 8(3), pp. 312–323. doi:10.26911/thejmch.2023.08.03.06.
McMaster University (2022) Figure 031_6302. Diagnostic algorithm for hyponatremia. Adapted from EUR J Endocrinol. 2014;170(3):G1-47 . McMaster textbook of internal medicine. Available at: https://empendium.com/mcmtextbook/image/B31.031_6302. (Accessed: 22 February 2024).
Neligan, P.J. (2024) ‘Fluid and electrolyte balance’, Anaesthesia & Intensive Care Medicine, 25(2), pp. 107–111. doi:10.1016/j.mpaic.2023.10.011.
Nuñez-Gonzalez, L., Carrera, N. and Garcia-Gonzalez, M.A. (2021) ‘Molecular basis, diagnostic challenges and therapeutic approaches of Bartter and Gitelman Syndromes: A Primer for clinicians’, International Journal of Molecular Sciences, 22(21), p. 11414. doi:10.3390/ijms222111414.
Roumelioti, M.-E. et al. (2018) ‘Fluid Balance Concepts in medicine: Principles and practice’, World Journal of Nephrology, 7(1), pp. 1–28. doi:10.5527/wjn.v7.i1.1.
Schrier, R.W. (2006) ‘Water and sodium retention in edematous disorders: Role of vasopressin and aldosterone’, The American Journal of Medicine, 119(7). doi:10.1016/j.amjmed.2006.05.007.
Seay, N.W., Lehrich, R.W. and Greenberg, A. (2020) ‘Diagnosis and management of disorders of body tonicity—hyponatremia and hypernatremia: Core curriculum 2020’, American Journal of Kidney Diseases, 75(2), pp. 272–286. doi:10.1053/j.ajkd.2019.07.014.
Sivakumar, S., Indrani and Divyapriya (2021) ‘Anemia profile in antenatal patients – A study at Tertiary Care Centre’, Indian Journal of Obstetrics and Gynecology, 9(1), pp. 27–29. doi:10.21088/ijog.2321.1636.9121.4.
Sosa, M. (2022) ‘Pseudohyponatremia in pregnancy’, Journal of Case Reports and Images in Obstetrics and Gynecology, 8, p. 1. doi:10.5348/100107z08ms2022cr.
Strazzullo, P. and Leclercq, C. (2014) ‘Sodium’, Advances in Nutrition, 5(2), pp. 188–190. doi:10.3945/an.113.005215.
V, Dr.A. et al. (2018) ‘Clinical profile of neonates admitted to a neonatal intensive care unit at a referral hospital in South India’, Pediatric Review: International Journal of Pediatric Research, 5(2), pp. 72–77. doi:10.17511/ijpr.2018.i02.06.
Weisz, K. and Hew-Butler, T. (2016) ‘Hyponatremia’, American Society for Clinical Laboratory Science, 29(3), pp. 168–175. doi:10.29074/ascls.29.3.168.
 write
write