1.0 Hypertension in Adults
Hypertension is a persistent health condition characterized by blood vessel pressure that goes beyond 140/90 mmHg (WHO, 2023). According to a study by Yildiz et al. (2020), hypertension can result in various adverse effects, such as cardiovascular complications, chest pains, and increased mortality rates if left untreated. Globally, an estimated 1.28 billion people aged between 30-79 years are affected by hypertension. Alarmingly, approximately 46% of people with hypertension are not aware. Furthermore, less than half (42%) of adults who have been diagnosed with hypertension are under treatment. Only around 21% of adults with hypertension have successfully achieved control over their blood pressure. Hypertension is a primary contributor to premature mortality globally, responsible for approximately 17.9 million fatalities, which represents 32% of global deaths (WHO, 2021).
Modifiable and non-modifiable are two types of risk factors associated with hypertension. Modifiable risk factors can be influenced and changed through lifestyle modifications. These include unhealthy eating habits such as consuming excessive amounts of salt, excessive tobacco and alcohol consumption, physical inactivity, having a diet rich in saturated fats, and obesity (Yusuf et al., 2020). On the other hand, non-modifiable risk factors refer to factors that are beyond one’s control or ability to change. These encompass factors such as having a familial predisposition to hypertension, being above the age of 65, and having pre-existing conditions like diabetes or kidney disease. In the US, hypertension is a significant concern, with the Centers for Disease Control and Prevention (CDC) reporting that one out of every four deaths is associated with this condition, resulting in a death every 36 seconds (CDC, 2018). The Global Burden of Disease Study reveals that in 2019, hypertension played a significant role in causing the loss of approximately 34.4 million years of life and disability-adjusted life years. This estimate has a confidence interval of 95%, ranging from 24.9 million to 43.6 million (Roth et al., 2020). Furthermore, the economic burden of hypertension is substantial. The US government spends approximately USD 363 billion annually on hypertension-related costs, including medications, healthcare services, and lost productivity due to morbidity and mortality. According to research conducted by Tsao et al. (2022), it is projected that these costs will escalate to USD 1 trillion by 2035. These alarming statistics underscore the significant public health impact of hypertension.
Yusuf et al. carried out a prospective cohort study in the year 2020 involving 155,722 individuals, the evaluation of 14 risk factors that could potentially be changed showed that behaviors like unhealthy eating habits and consuming excessive amounts of salt were responsible for approximately 26.3% of deaths. Furthermore, a meta-analysis by Schwingshackl et al. in 2017, analyzing 28 selected reports, demonstrated a direct risk of hypertension associated with certain foods; the study found that consuming 100g of red meat daily was associated with (RR) of 1.14 and (a CI) of 95% ranging from 1.02 to 1.28. Similarly, consuming 250ml of sugar-sweetened beverages per day was associated with (an RR) of 1.07 and (a CI) of 95% ranging from 1.04 to 1.10. Conversely, a negative relationship or decreased risk of hypertension was associated with consuming 30g of whole grains daily, with (RR) of 0.92 and 95% (CI) ranging from 0.87 to 0.98. Similarly, consuming 100g of fruits per day was linked to (RR) of 0.97, with a 95% (CI) ranging from 0.96 to 0.99. The findings of Schwingshackl et al. (2017) and Yusuf et al. (2020) highlight the positive correlation between certain foods and the predisposition to hypertension, as well as the potential for other foods to reduce the risk. This emphasizes the significance of nutrition in the prevention, management, and reduction of the effects linked to hypertension, as highlighted by the World Health Organization (WHO) in 2021. In this review of existing literature, we will thoroughly analyze the influence of nutrition in preventing hypertension, with a particular focus on the DASH diet as a nutritional intervention to combat hypertension and the concerns surrounding salt consumption and its impact on hypertension.
2.0 Literature Review
2.1 Salt Intake as a Nutritional Intervention Towards Hypertension
According to the British Dietetic Association (BDA) (2022), the suggested amount of salt to consume is between 0 and 0.3 grams per 100 grams of food, which is equivalent to 0.1 grams of sodium, with a maximum limit of 1.5g of salt (0.6g of sodium) per 100g of food. The National Health Service (2021) provides a simplified guideline of not exceeding 6g of salt per day (2.4g of sodium) for adults, with further reductions for children based on their age. These guidelines were established based on earlier studies indicating a direct link between increased salt consumption and the development or worsening of hypertension (Gradual, 2018). However, recent studies have shown that this association is weak, prompting a reevaluation of these recommendations. According to Gradual (2018), the limited link between lowering salt consumption to below 6 grams per day, as advised, is particularly evident among individuals who are not obese and those with normal blood pressure. The researchers also noted a noteworthy discovery that the current guideline for reducing salt below 6 grams per day triggers the renin-angiotensin-aldosterone (RAS) system, resulting in elevated plasma lipids and higher rates of mortality. These findings suggest that the harm outweighs the benefits of strict salt reduction.
While a systematic review conducted by McLean et al. (2019) indicated a positive link between reducing salt intake and a decrease in hypertension, it also brought attention to a higher mortality rate among older individuals in Italy who switched from a high-salt diet to a low salt intake. Further research is necessary to comprehend this inverse relationship between low salt intake and high mortality. Gradual et al. (2020) did a similar review which included 195 studies with a total of 12,296 participants; the side effects of sodium reduction were found to be weakly associated with the intended goal of reducing hypertension. The recorded adverse effects encompassed elevated levels of hormones such as renin (55%), aldosterone (127%), noradrenaline (27%), and adrenaline (14%), as well as increased levels of lipids such as cholesterol (2.9%), triglycerides (6.3%), and low-density lipoprotein (Gradual et al., 2020). This inverse relationship raises concerns as these hormone and lipid increases are associated with stress and negative health impacts, including higher mortality rates (Gradual et al., 2020). The evidence presented supports the call made by Gradual and Jürgens (2018) to review the recent guidelines for day-to-day salt intake. This position is also supported by Filippou et al. (2020) in their meta-analysis, which suggests that the DASH diet alone, without sodium reduction, can effectively lower blood pressure, especially in individuals with normal to high sodium intake and younger age.
2.2 Dietary Approach (DASH Diet) as a Nutritional Intervention to Curb Hypertension
Siervo et al. (2015) defined DASH diet as an eating plan aimed at reducing or managing hypertension by emphasizing the consumption of essential nutrients such as potassium, calcium, magnesium, fiber, and vegetable proteins. According to Challa et al. (2021), the DASH diet typically consists of around 5 servings of vegetables daily, 5 servings of fruits daily, 7 servings of carbohydrates daily, 2 servings of low-fat dairy products daily, and 2 to 3 servings of nuts and seeds on a weekly basis. This framework acts as a foundation that can be adapted based on the context, location, available food options, and the target population for implementation.
Siervo et al. (2015) conducted a comprehensive analysis of 20 articles involving 1917 participants over intervention periods ranging from 2 to 24 weeks. The findings of the study revealed that DASH diet is an effective nutritional intervention in reducing hypertension. The findings demonstrated a significant reduction in systolic blood pressure (SBP) (-5.2mmHg, 95%CI, P<0.001), diastolic blood pressure (DBP) (-2.6mmHg, 95%CI, P<0.001), as well as total cholesterol and LDL cholesterol levels, which are risk factors associated with cardiovascular disease. These results suggested a 13% reduction in the 10-year incidence of cardiovascular disease based on the Framingham risk score (Siervo et al., 2015). Similarly, Filippou et al. (2020) conducted a study involving 30 randomized control trials with 5545 participants, the impacts of the DASH diet on individuals with and without hypertension were examined. The results demonstrated a consistent link between the DASH diet and a lower risk of hypertension, regardless of whether individuals had existing hypertension or were taking antihypertensive medication (Filippou et al., 2020). These results support the current guidelines recommending early adoption of the DASH diet to prevent hypertension and enhance the effectiveness of antihypertensive treatment.
Although the DASH diet is known for its effectiveness in managing hypertension, it is important to exercise caution when introducing it to people who have particular chronic conditions like chronic kidney disease, heart failure, and diabetes or those who are taking RAS inhibitors or potassium-sparing diuretics. This is because of the relationship between the DASH diet with certain essential nutrients and the potential for metabolic complications (Tyson et al., 2012). Hence, it is crucial for healthcare professionals to conduct a comprehensive evaluation of individuals and provide close monitoring when implementing the DASH diet. This consideration is made because the benefits of achieving proper blood pressure control outweigh the potential risk of metabolic complications associated with the diet. The consistent inverse association between the DASH diet and hypertension, along with statistically significant results favoring the null hypothesis, clearly indicate that the DASH diet is the most effective approach for minimizing hypertension (Filippou et al., 2020). Finally, Challa et al. (2021) posit that the adaptability and feasibility of replicating the DASH diet in various settings and populations contribute to its strength as an intervention for hypertension management.
3.0 Conclusion and Recommendations
Hypertension poses a significant global public health challenge, and its impact continues to grow. Effectively addressing this problem requires a strong focus on modifiable risk factors, particularly nutrition. Based on extensive evidence and literature reviewed above, DASH diet proved to be the best nutritional intervention to combat hypertension. While reducing salt intake has been recommended to reduce hypertension (less than 2.4g of sodium per day), a reevaluation is warranted due to the potential side effects that outweigh the benefits, including the recent association with mortality. Therefore, it is recommended to prioritize strict adherence to the DASH diet while maintaining normal salt intake as a sufficient strategy to prevent, reduce, or manage hypertension effectively. Early adoption of this approach in life is encouraged to maximize its benefits.
4.0 Health Promotional Material – DASH Diet Poster
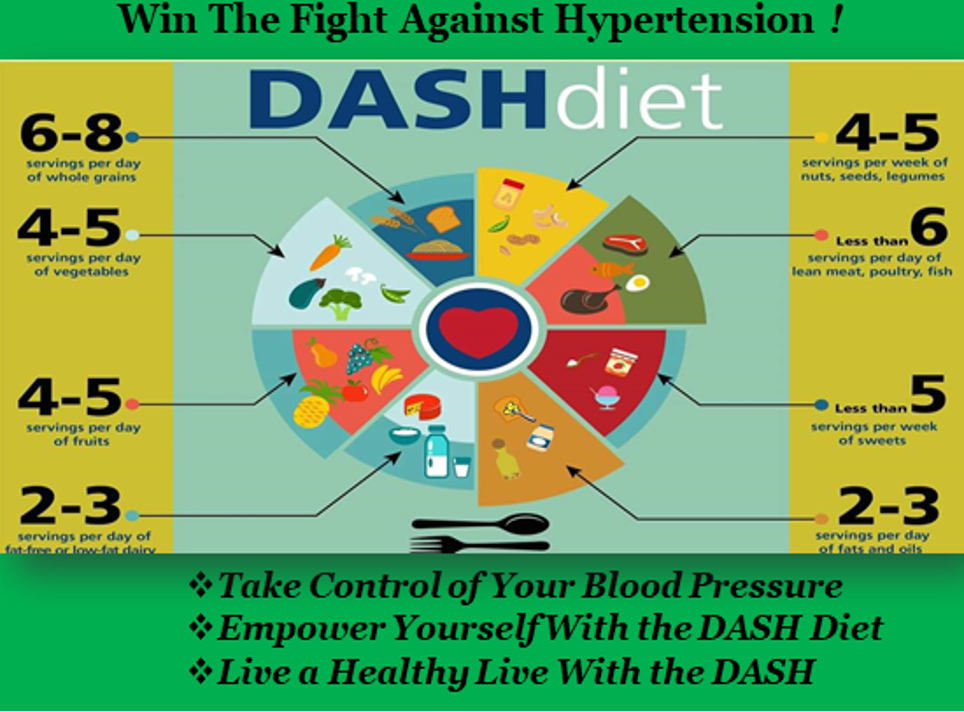
Figure 1: DASH Diet Poster
5.0 Evaluation of the DASH Diet Poster
According to Clarke (1999), evaluation is a methodical examination of a program, encompassing its execution and outcomes, with the aim of acquiring knowledge and making informed decisions. This is consistent with Rossi et al.’s (2018) definition and evaluation approach, which highlights the significance of assessing a program at its initiation, midpoint, and conclusion. Such evaluations are crucial for identifying errors and making necessary adjustments to ensure the effectiveness of the initiative or program. The purpose of this evaluation is to gauge the impact of the poster featured in Figure 1 on reducing hypertension among individuals attending the hypertensive and diabetes (HPT/DM) clinic at a community hospital in Swansea.
The poster provides a concise overview of the consequences of hypertension and offers guidance on prevention and control through the implementation of the DASH diet and maintaining a normal salt intake, as substantiated by the earlier literature review. Moreover, the poster incorporates visual depictions of everyday food choices and emphasizes the essential elements of the DASH diet using food groups, thereby making it relatable and applicable to individuals based on their local or familiar dietary preferences. This approach is adopted due to the diverse population residing in Swansea and seeking healthcare services at the community hospital. The posters will be printed and placed in strategic locations along the community hospital where individuals can easily read them as they pass. Additionally, flyers will be produced and circulated among all HPT/DM patients, with minor adjustments made to the DASH diet guidelines for particular groups, such as individuals with chronic kidney disease or heart failure, taking into account the metabolic complications highlighted in the literature review. The evaluation procedure will involve four primary components, as outlined by Gibson (2005): anthropometric measurements (such as weight), biochemical parameters (such as cholesterol level), clinical evaluation (such as physical examinations), and dietary history. All four components will be utilized in this evaluation of the nutritional program.
At the program’s commencement, the patients’ body mass index (BMI) will be assessed using anthropometric measurements, and their blood pressure levels will be recorded through clinical evaluation, specifically physical examinations. These assessments will be conducted every three months during the patients’ regular visits to the HPT/DM clinic. Patients will be urged to strictly follow the DASH guidelines outlined in the flyer based on their dietary history. Additionally, a food frequency questionnaire will be administered on a monthly basis, and feedback will be provided quarterly during the patients’ visits to the HPT/DM clinic. Although the food frequency questionnaire has limitations, such as low dietary recall and reliance on memory, it was selected due to its cost-effectiveness and ability to accommodate foods consumed in significant quantities, as highlighted by Walton et al. (2020). This approach aims to create a sense of urgency and motivate patients to closely adhere to the guidelines, as their progress will be continuously monitored.
To evaluate the influence of the DASH diet on serum cholesterol levels, a fasting lipid profile test will be performed at the program’s onset and repeated every six months using biochemical assessment techniques. A decrease in BMI, blood pressure, and cholesterol levels will serve as indicators of the intervention’s effectiveness. In summary, the program will be assessed at the beginning, followed by monthly dietary evaluations, quarterly anthropometry and clinical examinations, and biochemical evaluations every six months. As the target population comprises chronic disease patients, the intervention focuses on managing their long-term condition, and therefore, no final assessment or evaluation will be conducted.
6.0 References
British Dietetic Association (BDA). (2022). Hypertension and Diet: Food fact sheet. https://www.bda.uk.com/resource/hypertension-diet.html
Center for Disease Control and Prevention. (2018). Underlying Cause of Death, 1999–2018; CDC WONDER Online Database; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2018. In.
Challa, H. J., Ameer, M. A., & Uppaluri, K. R. (2021). DASH Diet To Stop Hypertension. https://www.ncbi.nlm.nih.gov/books/NBK482514/
Clarke, A. (1999). Evaluation research: An introduction to principles, methods, and practice. Evaluation Research, 1-224. https://www.torrossa.com/en/resources/an/4911962
Filippou, C. D., Tsioufis, C. P., Thomopoulos, C. G., Mihas, C. C., Dimitriadis, K. S., Sotiropoulou, L. I., Chrysochoou, C. A., Nihoyannopoulos, P. I., & Tousoulis, D. M. (2020). Dietary Approaches to Stop Hypertension (DASH) Diet and Blood Pressure Reduction in Adults with and without Hypertension: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Advances in Nutrition, 11(5), 1150-1160. https://doi.org/10.1093/advances/nmaa041
Gibson, R. S. (2005). Principles of nutritional assessment. Oxford university press, USA. https://books.google.co.ke/books?hl=en&lr=&id=lBlu7UKI3aQC&oi=fnd&pg=PR11&dq=evaluation+process+will+encompass+four+main+components,+including+anthropometric+measurements+(such+as+weight),+biochemical+parameters+(such+as+cholesterol+level),+clinical+evaluation+(such+as+physical+examinations),+and+dietary+history,&ots=RXTCOTcsrG&sig=cb6FCh0nhSB1UWb8txzmNURIkMM&redir_esc=y#v=onepage&q&f=false
Graudal, N., & Jürgens, G. (2018). Conflicting Evidence on Health Effects Associated with Salt Reduction Calls for a Redesign of the Salt Dietary Guidelines. Progress in Cardiovascular Diseases, 61(1), 20-26. https://doi.org/https://doi.org/10.1016/j.pcad.2018.04.008
Graudal, N. A., Hubeck-Graudal, T., & Jurgens, G. (2020). Effects of low sodium diet versus high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride. Cochrane Database of Systematic Reviews(12). https://doi.org/10.1002/14651858.CD004022.pub5
McLean, R. M., Petersen, K. S., Arcand, J., Malta, D., Rae, S., Thout, S. R., Trieu, K., Johnson, C., & Campbell, N. R. (2019). Science of salt: A regularly updated systematic review of salt and health outcomes studies (April to October 2018). The Journal of Clinical Hypertension, 21(8), 1030-1042.
National Health Service. (2021). Salt: the facts. https://www.nhs.uk/live-well/eat-well/food-types/salt-nutrition/#:~:text=Adults%20should%20eat%20no%20more,)%20%E2%80%93%20that’s%20around%201%20teaspoon.&text=Children%20aged%3A,a%20day%20(1.2g%20sodium)
Roth, G. A., Mensah, G. A., Johnson, C. O., Addolorato, G., Ammirati, E., Baddour, L. M., Barengo, N. C., Beaton, A. Z., Benjamin, E. J., Benziger, C. P., Bonny, A., Brauer, M., Brodmann, M., Cahill, T. J., Carapetis, J., Catapano, A. L., Chugh, S. S., Cooper, L. T., Coresh, J., . . . Fuster, V. (2020). Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019: Update From the GBD 2019 Study. Journal of the American College of Cardiology, 76(25), 2982-3021. https://doi.org/https://doi.org/10.1016/j.jacc.2020.11.010
Rossi, P. H., Lipsey, M. W., & Henry, G. T. (2018). Evaluation: A systematic approach. Sage publications.
Schwingshackl, L., Schwedhelm, C., Hoffmann, G., Knüppel, S., Iqbal, K., Andriolo, V., Bechthold, A., Schlesinger, S., & Boeing, H. (2017). Food Groups and Risk of Hypertension: A Systematic Review and Dose-Response Meta-Analysis of Prospective Studies. Advances in Nutrition, 8(6), 793-803. https://doi.org/10.3945/an.117.017178
Siervo, M., Lara, J., Chowdhury, S., Ashor, A., Oggioni, C., & Mathers, J. C. (2015). Effects of the Dietary Approach to Stop Hypertension (DASH) diet on cardiovascular risk factors: a systematic review and meta-analysis. British Journal of Nutrition, 113(1), 1-15. https://doi.org/10.1017/S0007114514003341
Tsao, C. W., Aday, A. W., Almarzooq, Z. I., Alonso, A., Beaton, A. Z., Bittencourt, M. S., Boehme, A. K., Buxton, A. E., Carson, A. P., & Commodore-Mensah, Y. (2022). Heart Disease and Stroke Statistics—2022 Update: A Report From the American Heart Association. Circulation, 145(8), e153-e639.
Tyson, C. C., Nwankwo, C., Lin, P.-H., & Svetkey, L. P. (2012). The Dietary Approaches to Stop Hypertension (DASH) Eating Pattern in Special Populations. Current Hypertension Reports, 14(5), 388-396. https://doi.org/10.1007/s11906-012-0296-1
Yusuf, S., Joseph, P., Rangarajan, S., Islam, S., Mente, A., Hystad, P., Brauer, M., Kutty, V. R., Gupta, R., & Wielgosz, A. (2020). Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. The Lancet, 395(10226), 795-808. https://doi.org/https://doi.org/10.1016/S0140-6736(19)32008-2
Yildiz, M., Esenboga, K., & Oktay, A. A. (2020). Hypertension and diabetes mellitus: highlights of a complex relationship. Current Opinion in Cardiology, 35(4), 397-404. https://doi.org/10.1097/hco.0000000000000748
Walton, J. (2015). Dietary assessment methodology for nutritional assessment. Topics in Clinical Nutrition, 30(1), 33-46. https://doi.org/10.1097/TIN.0000000000000018
WHO. (2021). Hypertension-fact sheet. https://www.who.int/news-room/fact-sheets/detail/hypertension
World Health Organization (2023). Hypertension Fact Sheet. Available at: https://www.who.int/news-room/fact-sheets/detail/hypertension
 write
write