Hemostasis and Platelets
Hemostasis is the natural process in which the body heals itself following an injury. According to LaPelusa and Dave (2021), hemostasis is a process in which the body stops bleeding from an injury and starts the process of wound healing. The process starts with a vascular spasm followed by the formation of a platelet plug and finally blood coagulation. Other than facilitating recovery in the site of injury, hemostasis also saves the lives of patients.
Platelets play a critical role in hemostasis. According to LaPelusa and Dave (2021), platelets are disc-shaped cells that are responsible for forming clots at the site of injury and preventing further bleeding. Platelets, which are also known as thrombocytes, are produced in the bone marrow from megakaryocytes after derivation from pluripotent stem cells. These cells are produced in large numbers. According to Banasik and Copstead (2019), there are between 150,000 and 400,000 platelets in each milliliter of blood. The body must maintain this number of platelets to facilitate swift healing following injuries. As such, a majority of these cells are in free circulation to necessitate fast transportation to the site of injury. Although most of the platelets circulate freely in the body, 25% of the cells are stored in the spleen and the liver (Banasik & Copstead, 2019). These cells are continuously replenished since their lifespan varies from seven to 12 days.
Thrombocytopenia
Thrombocytopenia is one of the most common disorders associated with platelets and hemostasis. According to Banasik and Copstead (2019), thrombocytopenia is a disorder characterized by a low blood platelet count. This low count slows down the accumulation of platelets in the site of injury and inhibits healing. Studies show that the overall prevalence of thrombocytopenia is 14.9% (Jali & Nkambule, 2020). This disorder poses a critical danger to patients’ health and lives since it slows down the process of blood clotting. A recent study found that every 15-minute decrease in time to hemostasis leads to decreased 30-day mortality and decreased incidence of sepsis, acute kidney injury, multiple organ failure, and acute respiratory distress syndrome (Chang et al., 2020). While medical professionals strive to help their patients recover faster, it is important to teach the community about best practices that can increase the platelets count and hasten the process of hemostasis following an injury. Some of the factors that facilitate swift hemostasis include fibrinogen (factor I), prothrombin (factor II), tissue thromboplastin or tissue factor (factor III), ionized calcium (factor IV), labile factor or proaccelerin (factor V), stable factor or proconvertin (factor VII), and antihemophilic factor (factor VIII) (Banasik & Copstead, 2019). However, other factors like antithrombin III, protein C, protein S, alcoholism, bone marrow disease, autoimmune disease, chemotherapy, and radiotherapy can also aggravate thrombocytopenia and inhibit hemostasis (Banasik & Copstead, 2019; Goyal & Badyal, 2018; Jinna & Khandhar, 2021).
Thrombocytopenia Pathophysiology
Thrombocytopenia is classified based on the disorder’s duration. According to Jinna and Khandhar (2021), the disease is classified as newly diagnosed, persistent (3-12 months), or chronic (longer than 12 months). The disease indiscriminately affects people of all genders. However, it is more common among middle-females compared to middle-aged males (Herman et al., 2020; Saber et al., 2021. The disease is also common among children whose parents had the disease due to the crossing of antiplatelet antibodies over the placenta.
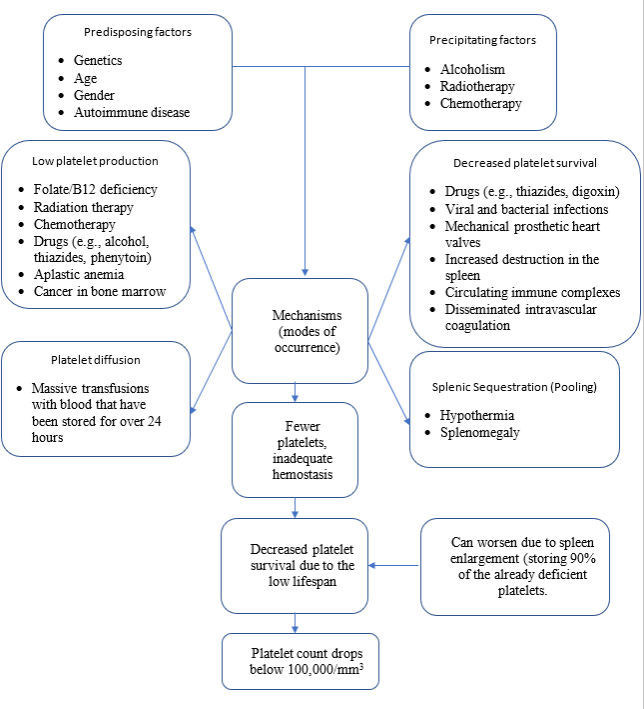
Thrombocytopenia has four mechanisms of occurrence. As Banasik and Copstead (2019) describe, these mechanisms include decreased platelet production, decreased platelet survival, intravascular dilution of circulating platelets, and splenic sequestration or pooling. As demonstrated in figure 1 below, decreased platelet production occurs folate (vitamin B12) deficiency, cancer treatment (radiation therapy and chemotherapy), the use of drugs/substances (phenytoin, thiazides, and alcohol), aplastic anemia, and bone marrow cancer (Banasik & Copstead, 2019). On the other hand, the decreased survival of platelets results from the use of drugs/substances, the presence of prosthetic heart valves, circulating immune complexes, disseminated intravascular coagulation, viral/bacterial infection, and increased destruction in the spleen (Banasik & Copstead, 2019). As explained earlier, this mechanism is worsened by platelets’ low lifespan of between seven and 12 days. In this case, platelets count continues to drop since the rate of replenishment is insufficient. Thrombocytopenia also occurs when a patient is transfused with a large volume of blood that has been stored for more than 24 hours. In this case, the low lifespan of the platelets means that many of them will have died during the storage period. Finally, splenic sequestration or pooling occurs due to hypothermia and splenomegaly. The platelet count lowers dramatically regardless of the mechanism of action.
Figure 1: Thrombocytopenia Pathophysiology
Prognosis
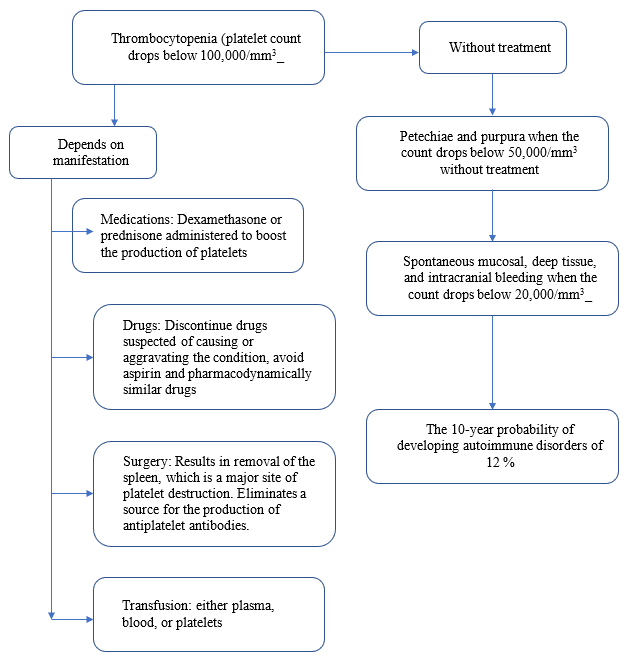
Thrombocytopenia requires medical attention. As explained earlier, the disease affects almost a sixth of the population. The disease can be life-threatening if untreated among patients with severe and chronic cases. One way to treat thrombocytopenia is through medications. Studies have found that dexamethasone or prednisone can boost the production of platelets, particularly when used in combination with rituximab (Wei et al., 2016; Xiao et al., 2021). Patients must also be advised to abandon the use of medications that are suspected to cause the disease. According to Banasik and Copstead (2019), some of these medications include thiazides, furosemide, heparin, digoxin, and certain antibiotics. Patients should also quit alcohol and other substances. Splenectomy may also be conducted to eliminate the organ responsible for holding up to 90% of the platelets and producing anti-platelet antibodies that damage platelets (Banasik & Copstead, 2019). Patients can also benefit from the transfusion of platelets, plasma, or blood. These interventions can improve platelet production. However, lack of treatment can increase the 10-year probability of developing autoimmune disorders by 12% (Jinna & Khandhar, 2021). Figure 2 below is an illustration of thrombocytopenia’s prognosis.
Figure 2: Thrombocytopenia prognosis
References
Chang, R., Kerby, J. D., Kalkwarf, K. J., Van Belle, G., Fox, E. E., Cotton, B. A., Cohen, M. J., Schreiber, M. A., Brasel, K., Bulger, E. M., Inaba, K., Rizoli, S., Podbielski, J. M., Wade, C. E., & Holcomb, J. B. (2019). Earlier time to hemostasis is associated with decreased mortality and rate of complications: Results from the Pragmatic Randomized Optimal Platelet and Plasma Ratio trial. Journal of Trauma and Acute Care Surgery, 87(2), 342–349. https://doi.org/10.1097/ta.0000000000002263
Copstead, L. E., & Banasik, J. L. (2020). Pathophysiology. St. Louis, Missouri: Elsevier.
Goyal, S., & Badyal, D. (2018). Significant thrombocytopenia with sodium valproate in an adult patient with alcohol dependence. Indian Journal of Psychiatry, 60(2), 252-253. https://doi.org/10.4103/psychiatry.indianjpsychiatry_158_17
Hermann, W., Risch, L., Grebhardt, C., Nydegger, U. E., Sakem, B., Imperiali, M., Renz, H., & Risch, M. (2020). Reference Intervals for Platelet Counts in the Elderly: Results from the Prospective SENIORLAB Study. Journal of Clinical Medicine, 9(9), 2856. https://doi.org/10.3390/jcm9092856
Jali, A. G., & Nkambule, B. B. (2020). Prevalence and etiology of moderate and severe thrombocytopenia in a tertiary and quaternary center in KwaZulu-Natal. African Journal of Laboratory Medicine, 9(1). https://doi.org/10.4102/ajlm.v9i1.799
Jinna, S., & Khandhar, P. B. (2021, July 25). Thrombocytopenia. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK542208/
LaPelusa, A., & Dave, H. D. (2021, May 9). Physiology, Hemostasis. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK545263/
Saber, A. M., Aziz, S. P., Almasry, A. Z. E., & Mahmoud, R. A. (2021). Risk factors for severity of thrombocytopenia in full-term infants: A single-center study. Italian Journal of Pediatrics, 47(1), 1-7. https://doi.org/10.1186/s13052-021-00965-1
Wei, Y., Ji, X., Wang, Y., Wang, J., Yang, E., Wang, Z., Sang, Y., Bi, Z., Ren, C., Zhou, F., Liu, G., Peng, J., & Hou, M. (2016). High-dose dexamethasone vs prednisone for the treatment of adult immune thrombocytopenia: a prospective multicenter randomized trial. Blood, 127(3), 296–302. https://doi.org/10.1182/blood-2015-07-659656
Xiao, Q., Lin, B., Wang, H., Zhan, W., & Chen, P. (2021). The Efficacy of High-Dose Dexamethasone vs. Other Treatments for Newly Diagnosed Immune Thrombocytopenia: A Meta-Analysis. Frontiers in Medicine, 8(1), 656792. https://doi.org/10.3389/fmed.2021.656792
 write
write