Introduction
Cervical cancer is one of the most preventable types of cancer, largely due to effective screening programs that allow for the early detection and treatment of pre-cancerous cervical lesions (NHS, 2022). In England, a national cervical screening programme has been in place since 1988, which invites women between the ages of 25 and 64 for regular smear tests to check for abnormal cervical cells (PHE, 2024). It is estimated that this programme prevents up to 5,000 cervical cancer cases each year (CRUK, 2023). However, participation rates have declined, with coverage rates dropping from 72.7% to 69% over the past decade (Douglas et al., 2016).
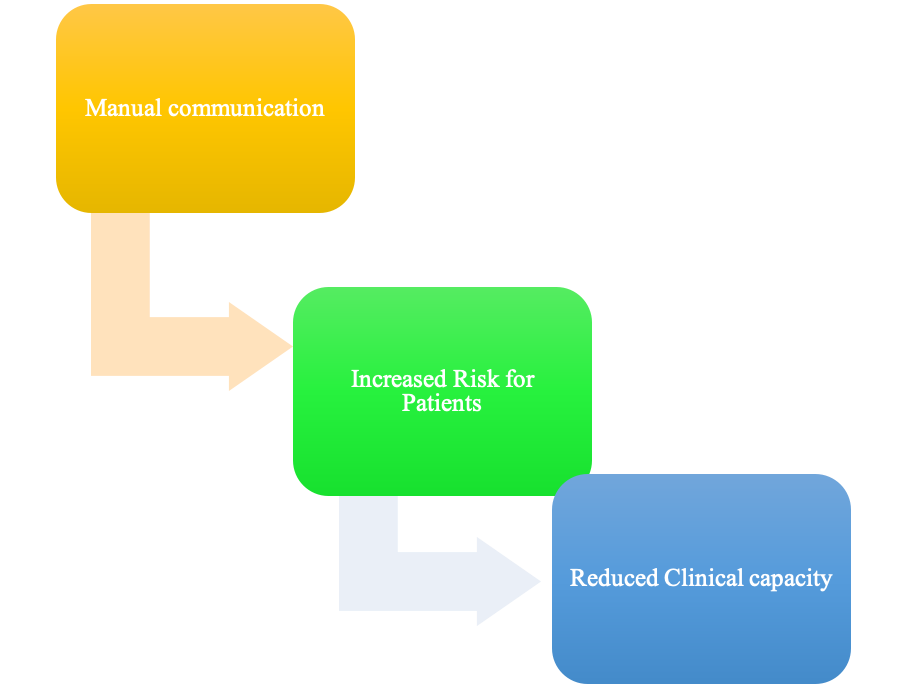
Our general practice clinic carries out approximately 350 cervical screenings each year as part of this national screening programme. Of these tests, around 10% detect abnormal cells that require additional follow-up testing or referral to specialists (PHE, 2024). The current system relies heavily on paper letters, phone calls, and faxes to coordinate follow-up care when abnormal results are found. This leads to dangerous delays and gaps in care continuity – putting patients at risk. Recent research has shown that failures in the follow-up system account for 30% of malpractice claims related to cervical screening (Castanon et al., 2013). To address these problems, we have secured funding through a national digital health initiative to overhaul and automate parts of our current cervical screening pathway. This report provides background on our clinic, analyses key needs identified amongst stakeholders, proposes a system design to transform screening coordination, and provides guidance for implementation and evaluation.
Background and Context
Cervical cancer remains an ongoing public health concern in the UK, with over 27,500 new cases of cervical carcinoma in situ recorded annually. Incidence rates peak among 25-29-year-old women but have declined 10% in the past decade (CRUK, 2023). However, significant inequities exist, with 18% higher incidences in England’s most deprived areas accounting for 2,000 extra cases a year (CRUK, 2023). Mortality sits around 850 deaths annually, predominantly occurring in women over 75 years old. Nevertheless, optimism exists given the 75% reduction in death rates since the 1970s, thanks to screening advancements, alongside a further 18% drop in the last ten years. Survival metrics also highlight progress – with 86% of women diagnosed before age 45 now surviving 10+ years and 63% across all age groups, up from just 46% in previous eras (CRUK, 2023).
However, England continues to lag behind European averages for 5-year survival. The vast majority of cervical cancer burden is preventable through HPV vaccination, targeting infections behind practically all cases. Further mitigating smoking can curb another 21% of the incidence (CRUK, 2023). Ongoing screening to detect pre-cancerous lesions, paired with improved access to timely, affordable treatment, has the potential to make cervical cancer progressively rare. Realising health equity across socioeconomic gradients remains vital to ensure equal prevention and survival opportunities regardless of deprivation. Continued vigilance and evidence-based intervention are needed to relegate cervical cancer to the historical archives eventually.
Our clinic serves a patient population of approximately 15,000, primarily covering the Little Whinging area. We have four general practitioners, two practice nurses, and five administrative staff members who assist with health records, referrals, and appointment bookings. Like most NHS general practices, our clinic utilises EMIS Web – an electronic health record system (EHR) that has been deployed nationally across primary and community care settings (EMIS Health, 2023). Most elements of our cervical screening care pathway have been digitised in EMIS, including tracking screening appointments, recording cervical samples, returning test results, and notifying patients. However, the processes surrounding abnormal results and specialist referrals remain highly manual, relying on paper letters from cytology laboratories to communicate positive results. Our practice nurses then phone the patients, consult paper records to assess screening history, and coordinate next steps for additional testing or onward referral depending on the grade of abnormality.
These referrals are completed by hand faxed to local colposcopy clinics, after which there are more phone calls to book appointments. Patients are added to paper registers to log referral status and follow-ups, which nurses must check regularly and manually update. The problem this system intends to solve is the need for more connectivity between stakeholders and data sources involved in follow-up care for abnormal cervical screening results. Relevant information lives in cytology lab systems, the EHR, paper records, referral clinics, and specialist systems – but there is no way to automatically piece these together to streamline care coordination tasks off the shoulders of our overburdened nurses. The delays this causes impact patient outcomes, while the duplication of administrative work reduces valuable clinical capacity (Huntington et al., 2023).
Proposed System Scope
To begin digitally transforming our abnormal results coordination processes, we propose developing the following tools and system integrations:
- Automated identification of abnormal results – Create tools to automatically flag abnormal cytology results within our EMIS system, using HL7 messaging from the laboratory information management systems (LIMS)
- Instant alerts for responsible staff – Configure custom EMIS protocols to instantly notify assigned care coordinators when relevant abnormal results return
- Streamlined referral generation – Build digitised referral templates that draw data from EMIS to minimise rework, integrated directly with specialist booking systems
By enhancing interoperability between existing health IT systems, developing structured data capture, implementing decision support alerts, and creating standardised electronic referrals, we can begin to bridge the gaps that currently hinder rapid, proactive follow-up care when screening detects cervical abnormalities. The scope of this proposal focuses specifically on the interfaces surrounding abnormal result coordination across the laboratory, GP surgery, and colposcopy clinic settings – rather than tackling the entirety of the screening pathway digitisation. Patient-facing tools for notification and appointment self-scheduling will not be included as part of this first stage.
Key Stakeholders & Needs
We conducted 30-minute interviews with representatives of each key stakeholder group impacted by cervical screening coordination activities to gather structured input on user needs related to our proposed system enhancements. The groups identified, their roles, and summary insights are highlighted in Table 1 below:
Table 1. Key Stakeholders and Needs
| Stakeholder Group | Role | Needs |
| Patients | Undergo regular cervical cancer screening; require appropriate follow-up care based on results | -Timely notifications when abnormal results are detected
– Convenient booking of necessary follow-up appointments – Coordination support throughout the pathway |
| Care Coordinators | Practice nurses tasked with managing screening registries, communicating results to patients, organising additional testing/referrals | – Tools to automatically receive abnormal result alerts
– Ability to digitally track pending recommended follow-ups – Streamlined generation/receipt/documentation of electronic referrals |
| General Practitioners | Responsible for overall care plans for patients; interpret results and determine appropriate triage based on clinical judgement | – Access to holistic clinical timeline in EHR including screening history, abnormal results, referral status and outcomes
– Real-time visibility of pending follow-up coordination tasks |
| Specialist Physicians | Receive referrals from primary care when abnormal results require examination by a colposcopy clinic; carry out biopsies treatments and communicate follow-up recommendations | – Structured symptom/history data paired with referrals
– Notifications when referrals are received to enable rapid triage – Ability to communicate digitally with referring GPs on patient care plans |
These structured insights gathered from subject matter experts amongst our own staff were supplemented by a review of literature on best practices for follow-up coordination processes. Researchers have highlighted the risks posed by fragmented, asynchronous communication channels between cytology labs, primary care clinics, and specialist providers (Rebolj et al., 2022). Integrating systems to push data to key decision-makers automatically is a recognised strategy for overcoming these issues (NHS Cancer Screening Programmes, 2022).
System Requirements
To visually outline how our proposed tools aim to bridge gaps in existing systems and transform interdisciplinary communication, two use case diagrams were developed – illustrating the current vs ideal future state workflows.
As shown in Figure 1 below, the current process is disjointed, relying on manual phone/paper-based communication channels that introduce critical delays:
Future State Diagram
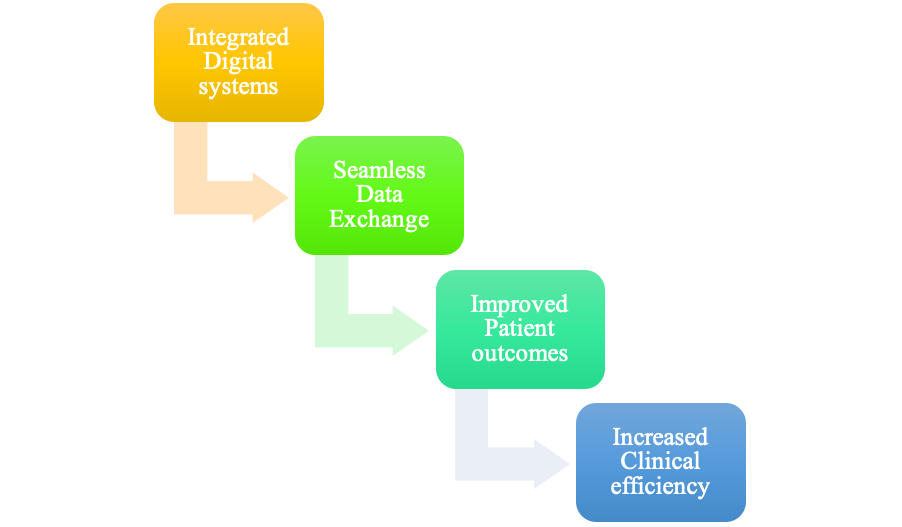
Our newly integrated digital systems would enable seamless data exchange and hand-offs between staff and institutions involved (Figure 2):
Therefore, to realise this future vision, our EHR vendor EMIS will need to incorporate several changes – detailed in the class diagram in Figure 3 below:
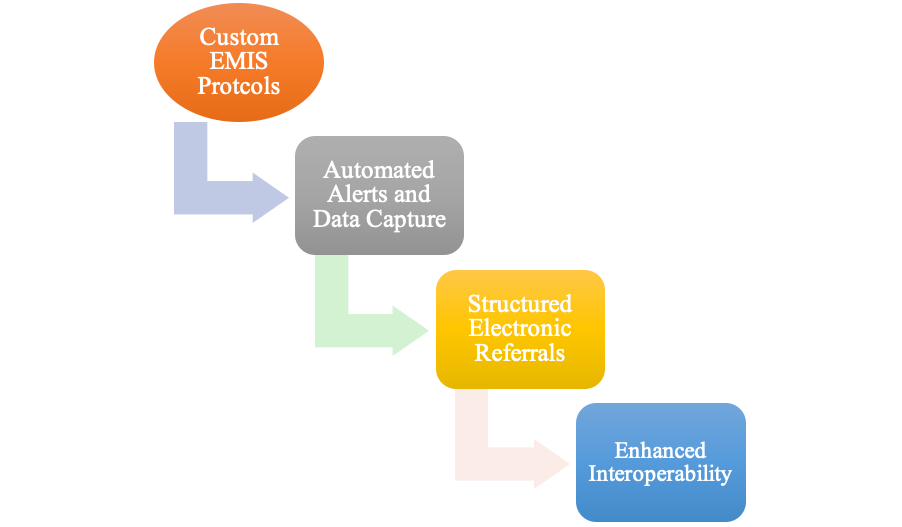
By working with EMIS to build custom protocols for our cervical screening registers that can ingest HL7 lab results, automatically flag abnormal findings, instantly notify staff via API alerts, and enable structured data capture for digital referrals and care plans, we can drive significant improvements.
Proposed System Design
The high-level system design, therefore, involves augmenting the use of the existing EMIS platform to remove paper-based processes. Machine-readable structured pathology result data will act as a trigger to automatically kick off downstream workflows to relevant stakeholders through digital alerts, task assignments, and referral initiation. The updated screening pathway powered by the enhanced system architecture is shown in the diagram below (Figure 4):
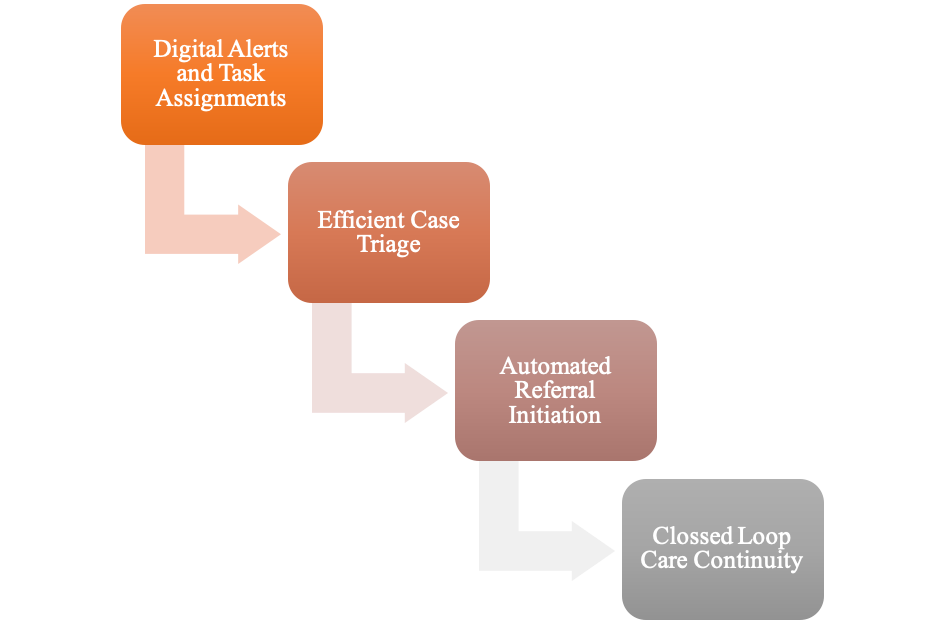
Through embedded protocols customised by our EMIS implementation team, the EHR will now fully replace manual registries, paper correspondence, and basic email/phone communication channels. Automatic notifications will facilitate rapid case triage to determine whether active follow-up is required or results can be filed if returned to normal. Configurable rules will instantly task-relevant general practitioners or nurses based on urgency as soon as abnormal results are validated. Referral templates will harness digitised data from across the patient record to limit rework. Harnessing the newest FHIR interoperability standards, these referrals will be transmitted electronically directly into the outpatient management systems used at our region’s colposcopy clinics – with acknowledgement messages confirming receipt.
Structured care plans from the specialist visits will similarly return to the central EMIS record – closing the loop to support continuity of care and vigilance in screening histories by all providers involved in a woman’s cervical health journey. By linking the relevant clinical and administrative stakeholders through shared data repositories on the back end, we can realise a fully integrated pathway.
Implementation Plan
In order to systematically deploy the range of infrastructure and software enhancements proposed, a structured implementation roadmap will need to be planned in collaboration with our EMIS implementation partners, the high-level timeline in Figure 5 summarises the phases and milestones expected:
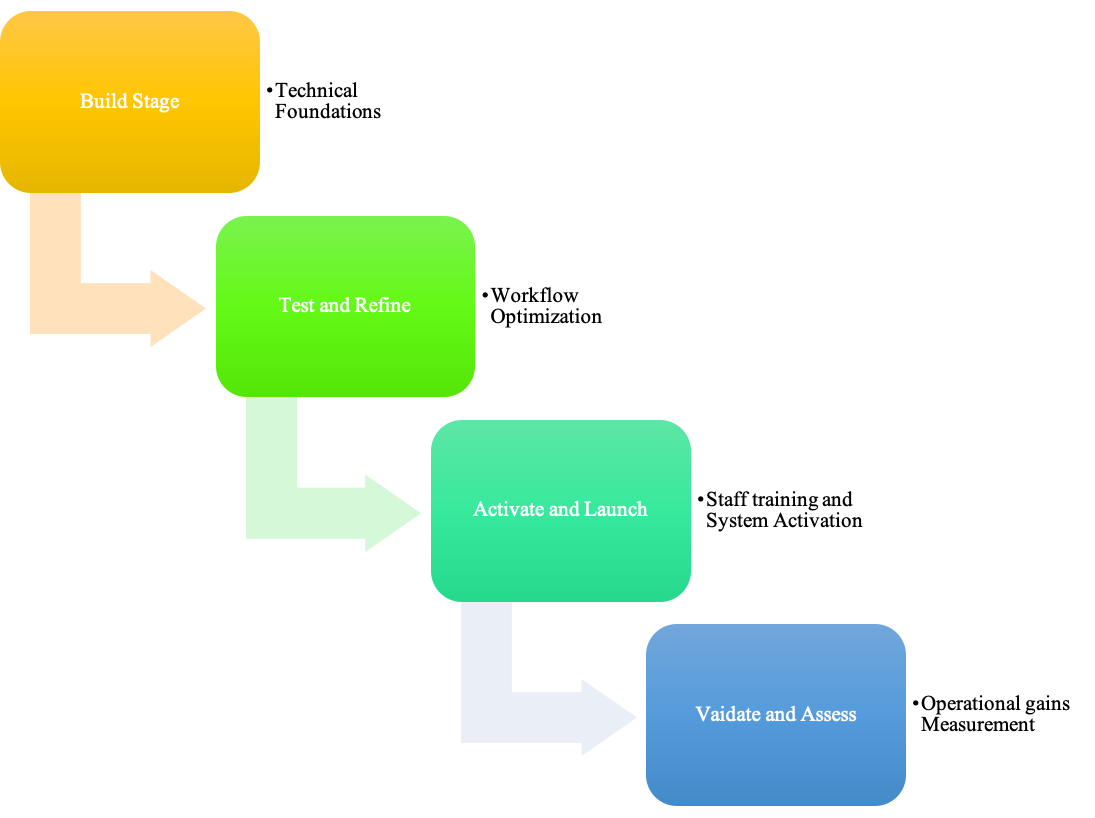
The initial focus during the Build stage will be on working alongside EMIS technical staff to establish the housekeeping elements needed within our system configuration to enable the additional functionality proposed. This includes defining protocols for ingesting the HL7 pathology result feeds, mapping terminologies, configuring user roles/permissions for various alert recipient groups, and building templates for digital referral forms and care plans. With these foundations established, the emphasis will shift to roll-out and testing during the Test & Refine phase. A core project team of GP, nursing, and administrative staff will collaborate closely with the EMIS support team on simulating use cases for screening result identification, care coordinator notification, referral initiations, acknowledgement, and care plan closure.
Using synthetic dummy patient data, end-to-end workflow tests will be undertaken repeatedly to identify frictions and change requirements prior to public launch. Once refinements are finalised during this trial deployment period, the system will be activated through staff orientation and training during Activate & Launch. With digital tools eliminating significant administrative tasks, additional capacity will be available to closely track adoption, support users, and resolve concerns early on. Post-implementation audits will help quantify operational gains in the Validate & Assess phase – feeding back into additional optimisation efforts. Throughout this process, clear protocols should be established for scenario testing and operational training to ensure the continuity of existing services. Core risk considerations relate to managing integrations with external referral systems, developing appropriate data-sharing agreements, and getting internal buy-in amongst providers accustomed to previous ways of working. Mitigation tactics involve early lab linkages, being transparent regarding data visibility, and co-designing workflows with frontline staff.
Evaluation Plan
To track the impact of the newly enhanced system capabilities once launched, both quantitative and qualitative metrics will need to be monitored across the key performance indicators detailed in Table 2 below:
Table 2. Evaluation Metrics & Targets
| Objective | KPI | Target |
| Improved timeliness of care | – Alert to triage elapsed time
– Referral receipt to appointment booking time |
– Median under 8 hours
– Median under 48 hours |
| Reduced wait times | – Average total days from abnormal result to treatment initiation | – 30% reduction within 12 months |
| Increased referrals completed | – Referral completion rate | 90% within one month |
| Enhanced care continuity | – Provider ratings of holistic patient information | – 80% report ‘good or excellent visibility’ |
| Higher staff productivity | – Nursing hours spent on admin per patient | – 50% reduction within six months |
Both system analytics as well as user feedback surveys will be used to regularly assess progress against each of these quantitative indicators at monthly intervals during the first year of deployment. Qualitative interviews with staff will also evaluate ease of use, ongoing opportunities for enhancement, and benefits realised through eliminated rework – providing richer insights to guide continual improvement efforts.
Conclusion and Recommendations
Inefficiencies and delays in our current cervical screening care coordination pathways are introducing dangerous gaps in follow-up care that require urgent intervention. This report summarises opportunities to implement integrated digital systems that enhance interoperability, automate key tasks, and help bridge communication barriers across the various interdisciplinary stakeholders involved.
Specific recommendations based on this analysis include:
- Developing EHR protocols to ingest pathology results and trigger alerts automatically
- Configuring instant notifications when abnormal results are identified to assign care coordinators
- Building templates to capture digital referral data and share it dynamically with specialist clinics
- Tracking quantitative process metrics around referral times as well as qualitative perceptions of continuity
Through structured enhancements of our existing health information systems guided by user-centred design thinking, our surgery can eliminate wasted administrative efforts and instead focus precious resources on enhancing the quality of cervical screening care. The thing is, if you introduce a series of small changes that are planned over time in relation to results coordination, referral generation, and care plan closure, for example, one will have a screening that is interwoven across institutional silos and not just being ordered test upon test. It is clear, therefore, that patient safety and outcomes stand to improve significantly thanks to timely follow-up and evidence-based vigilant management.
With reliable standards in place, additional patient-centred tools could subsequently be layered on this digital infrastructure in future phases – providing value-added support through screening appointment reminders, health education, and care navigation assistance. Therefore, steadily progressing towards preventive cancer screening that is smarter due to smart health systems would provide better early detection and survival outcomes in the long run.
References
Cancer Research UK (CRUK)., 2023. Cervical cancer statistics. https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/cervical-cancer#heading-Zero
Castanon, A., Leung, V.M.W., Landy, R., Lim, A.W.W. and Sasieni, P., 2013. Characteristics and screening history of women diagnosed with cervical cancer aged 20–29 years. British Journal of Cancer, 109(1), pp.35-41.
Douglas, E., Waller, J., Duffy, S.W. and Wardle, J., 2016. Socioeconomic inequalities in breast and cervical screening coverage in England: are we closing the gap? Journal of medical screening, 23(2), pp.98-103.
EMIS Health., 2023. EMIS Web – Connected healthcare software and systems. https://www.emishealth.com/products/emis-web/
Huntington, S., Sudhir, K.P., Schneider, V., Sargent, A., Turner, K., Crosbie, E.J. and Adams, E.J., 2023. Two self-sampling strategies for HPV primary cervical cancer screening compared with clinician-collected sampling: an economic evaluation. BMJ open, 13(6), p.e068940.
National Health Service (NHS)., 2022. Help Us, Help You – Cervical Screening Saves Lives. https://campaignresources.dhsc.gov.uk/campaigns/help-us-help-you-cancer/cervical-screening/#:~:text=Overview,they%20missed%20their%20last%20screening.
Public Health England (PHE). (2024). NHS Screening Programmes in England. https://www.gov.uk/topic/population-screening-programmes
Rebolj, M., Mathews, C.S., Denton, K., HPV Pilot Steering Group, Appleyard, T.L., Cruickshank, M., Cuschieri, K., Ellis, K., Evans, C., Frew, V. and Giles, T., 2022. Cytology interpretation after a change to HPV testing in primary cervical screening: Observational study from the English pilot. Cancer Cytopathology, 130(7), pp.531-541.
 write
write