Introduction
Obesity has reached epidemic levels in the United States, with rural communities like those in Tennessee being hit especially hard (CDC, 2022). Over one-third of Tennessee adults are obese, and rates are driven by complex, interlinking factors across socioecological levels (CDC, 2022; The Sycamore Institute, 2017). This case study provides an in-depth examination of the drivers of high obesity rates in rural Tennessee counties using an ecological framework. It proposes a multi-level intervention strategy grounded in evidence-based health behavior theories like the Health Belief Model, Transtheoretical Model, and Social Cognitive Theory. Aligned with the PRECEDE-PROCEED planning model, initiatives spanning individual, interpersonal, community, and policy levels are outlined to address root causes over a four-year implementation timeline.
The Obesity Profile in Rural Tennessee
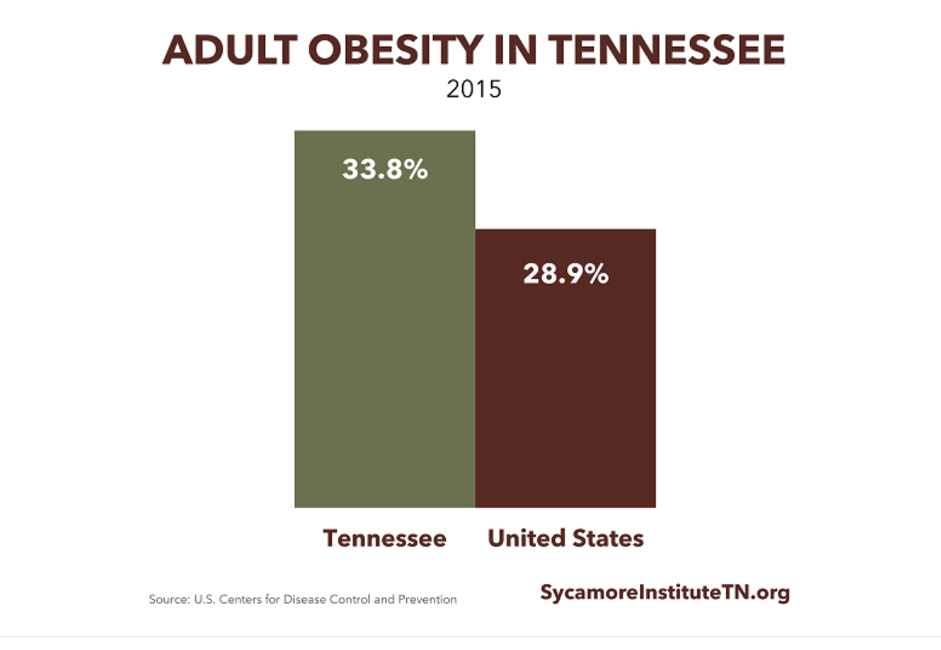
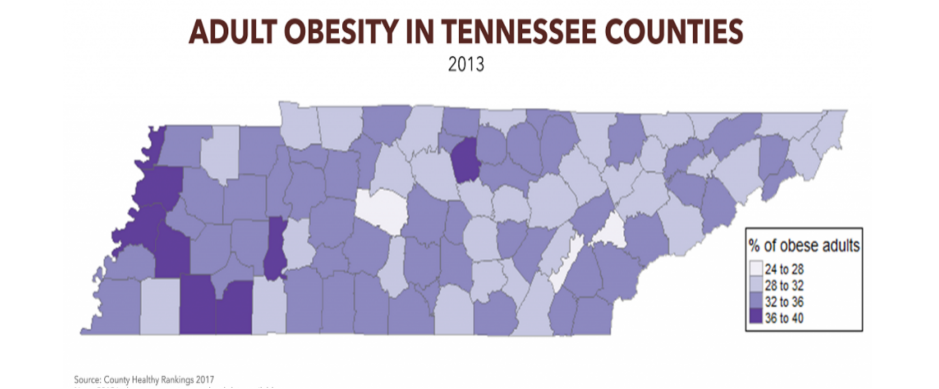
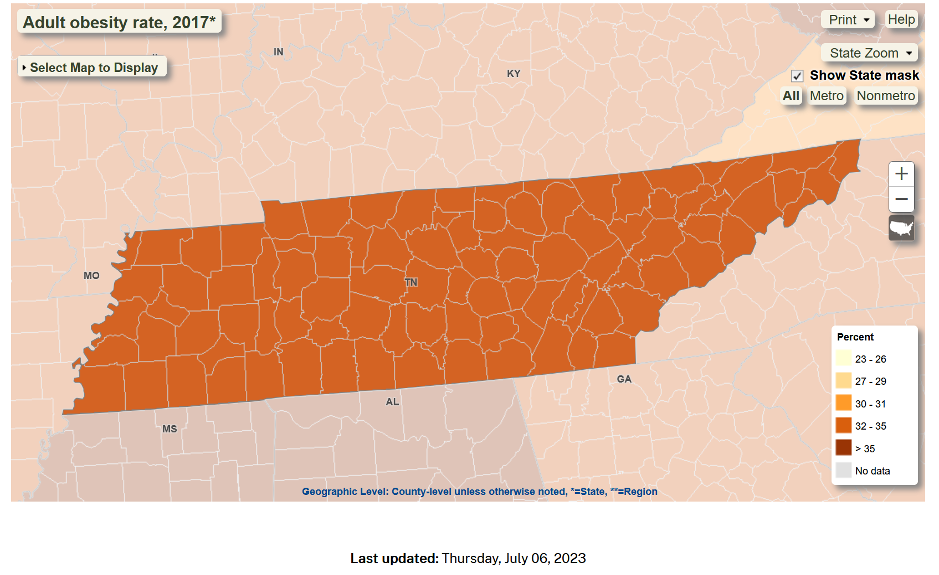
According to the CDC’s 2022 data, 37% of Tennessee adults are obese, higher than the national median of 33% (CDC, 2022). Prevalence varies by demographic factors; for instance, obesity rates are highest among non-Hispanic Blacks at 48.1% (CDC, 2022). Rural counties have slightly higher rates than metropolitan areas (Befort et al., 2012).
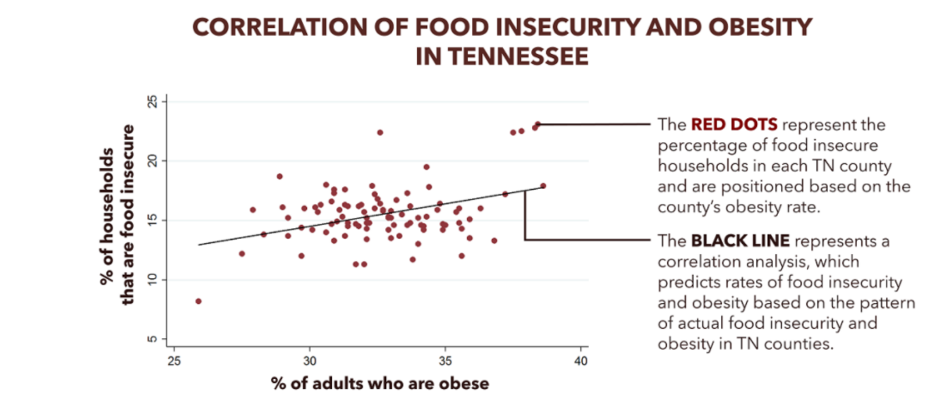
Food insecurity is another major contributor to obesity in Tennessee. 17% of Tennessee households experience food insecurity, higher than the national rate (The Sycamore Institute, 2017). Food insecurity promotes cycles of food deprivation and overeating, which can lead to weight gain over time (Dinour et al., 2007). Tennessee counties with higher food insecurity also tend to have higher obesity rates, demonstrating the link between the two issues (The Sycamore Institute, 2017).
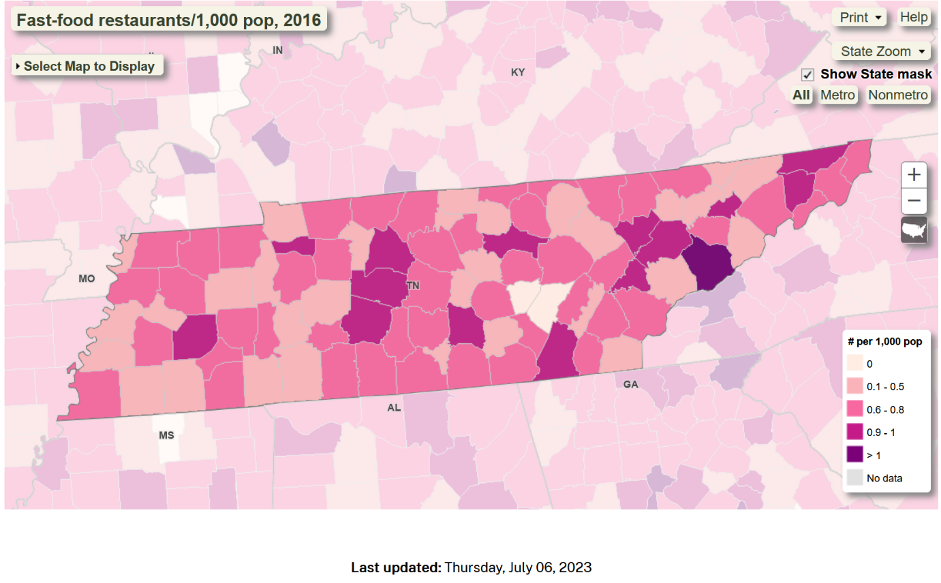
Additional factors in Tennessee’s health profile related to obesity include widespread fast food access, low produce consumption, sedentary lifestyles, and cultural attitudes accepting of larger body sizes (Befort et al., 2012).
Socioecological Linkages to Obesity
Obesity is a complex health issue with many interlinking societal and behavioral causes. Key factors specific to rural Tennessee that link environment and individual behaviors to the obesity epidemic include:
- a) Food insecurity leads to overeating when food becomes available, disrupting normal metabolic regulation (Adams et al., 2003)
- b) Limited access to fresh, affordable, healthy foods and overabundance of low-cost fast food restaurants (Larson et al., 2009)
- c) Car-dependent communities lacking pedestrian infrastructure that promotes active transport (Lovasi et al., 2009)
- d) Cultural attitudes accepting and even celebrating excess weight and traditional high-calorie foods (Befort et al., 2012)
- e) Minimal health education on nutrition, exercise, and obesity prevention starting in childhood (Tennessee Department of Education, 2021)
Assessing Quality of Life and Educational Needs
Several themes emerge from surveying the rural Tennessee landscape to assess the quality of life experiences, educational needs, and attitudes shaping behaviors. Food insecurity and poverty are major concerns, with low-income levels and high food insecurity rates limiting access to health resources (The Sycamore Institute, 2017). Local cultural values around food and activity patterns also contribute to obesity risks (Befort et al., 2012). There are misconceptions about nutrition and underestimation of the health consequences of obesity (Befort et al., 2012). Environments lack infrastructure promoting activity, while sedentary occupations have increased (Befort et al., 2012).
Analysis of Priority Contributing Factors
Food insecurity emerges as a priority intervention target based on its strong influence on obesity in Tennessee (The Sycamore Institute, 2017). At the individual level, food insecurity can promote metabolic dysregulation and unhealthy eating patterns (Adams et al., 2003). Household-level financial constraints determine food access and choices (The Sycamore Institute, 2017). Food insecurity and obesity share community and societal drivers like limited healthy food access and high poverty rates (The Sycamore Institute, 2017).
Recommended Intervention Strategies
Proposed initiatives to address food insecurity as an underlying driver of obesity include:
Individual Level
a) Nutrition education addressing food insecurity-obesity link
Household Level
a) Budgeting and shopping tips for accessing healthy foods on a limited income
Community Level
- a) Improving healthy food access via grocer partnerships and farmers’ markets
- b) Community kitchens and food pantries with fresh produce
Societal Level
- a) Policy changes to strengthen food security safety net programs
- b) Universal school meals and summer feeding programs
These strategies address root causes of food insecurity across socioecological levels to create supportive environments for healthy eating and obesity prevention.
Conclusion
This case study provides an overview of key factors driving high obesity rates in rural Tennessee, prioritizing food insecurity given its strong ties to obesity. A socioecological, multi-level intervention grounded in evidence-based health behavior theories is proposed to promote food security and reduce obesity risks. Taking an ecological approach involving coordinated individual, interpersonal, community, and policy changes can help address Tennessee’s complex obesity epidemic in an impactful, sustainable way.
References
- Centers for Disease Control and Prevention. (2016). Defining adult overweight and obesity. https://www.cdc.gov/obesity/adult/defining.html
- Centers for Disease Control and Prevention. (2017). Adult obesity prevalence maps. https://www.cdc.gov/obesity/data/prevalence-maps.html
- Coleman-Jensen, A., Rabbitt, M.P., Gregory, C.A., & Singh, A. (2016). Household food security in the United States in 2015. United States Department of Agriculture Economic Research Service. https://www.ers.usda.gov/webdocs/publications/err215/err-215.pdf?v=42636
- Critser, G. (2024). Fat nation: Why so many Americans are getting fatter and how government, medicine, and culture contribute to the problem. HarperCollins.
- Edberg, M. (2020). Essentials of health behavior: Social and behavioral theory in public health (2nd ed.). Jones & Bartlett Learning.
- Feeding America. (2016). Map the meal gap 2016: Highlights of overall and child food insecurity findings. http://www.feedingamerica.org/hunger-in-america/our-research/map-the-meal-gap/2014/map-the-meal-gap-2014-exec-summ.pdf
- Martin, K. S., & Ferris, A. M. (2007). Food insecurity and gender are risk factors for obesity. Journal of Nutrition Education and Behavior, 39(1), 31–36. http://dx.doi.org/10.1016/j.jneb.2006.08.024
- RTI International, Center for Health and Environmental Modeling. (2014). Current and prospective scope of hunger and food security in America: A review of current research. http://www.rti.org/sites/default/files/resources/full_hunger_report_final_07-24-14.pdf
 write
write