Introduction
Being an essential venture within Public Health, this project assumes great importance. With a focus on bridging the gap in regular dental care access, this initiative targets a significant disparity among Black and ethnic minority populations, particularly in London’s diverse and dynamic environment. Regular dental visits refer to scheduled appointments with a dentist for preventive and proactive oral health care (Steinvik et al., 2023). These appointments are typically recommended at regular intervals, such as every six months, although the specific frequency may vary based on individual oral health needs and recommendations from dental professionals (Charadram et al., 2021).
Empirical findings underscore a significant shift in dental care-seeking behaviour, with the majority of the UK population (about a third) focusing on addressing immediate pain or issues rather than proactive measures (Currie et al., 2021). According to recent statistics, only half of the global population (54%) accesses regular/preventive dental care, highlighting a persistent issue (Currie et al., 2021). The findings from the 2022 Access to NHSdental services report underscore the gap between the White British group (95.5%) and the Black African group (88.4%), with the former demonstrating markedly higher appointment booking success in the UK (Access to NHSdental services, 2022). The persistent gap highlights the urgent importance of tailored measures to improve dental care availability and usage.
A multifaceted challenge emerges in the backdrop of London, celebrated as the UK’s most ethnically diverse city. According to the 2011 Census, a mere 46% of London’s populace identifies as White British, underlining the city’s ethnically heterogeneous composition (Arora et al., 2016). Ethnic minority groups within London confront hurdles in accessing dental appointments, resulting in extended wait times and limited accessibility to preventive care. A symptom-oriented approach is typical among certain ethnic groups, including the Bangladeshi and Vietnamese communities, which often neglect regular checkups (Marshman, Nower, and Wright, 2013).
Deeply embedded in Public Health, this project’s importance is bridging oral health gaps and broader health concerns among Black and ethnic minority groups. The project’s focus on regular dental checkups supports the broader objective of improving community health and preventive care habits. Hence, this project underscores the importance of equitable dental care access and outlines a strategic pathway to address this pertinent challenge, contributing to advancing Public Health objectives within a multicultural urban context.
Project Initiation
This crucial segment sets forth the limits of our undertaking and supports its justification through logical reasoning. The success of this initiative rests upon precise analysis and factual reasoning. This undertaking includes the visualised makeover, arduous hurdles, and exciting possibilities.
Force Field Analysis and Lewin’s Change Theory
The Force Field Analysis is a strategic tool used to evaluate and visualise the driving forces that promote change and the restraining forces that hinder it within a specific context. It provides a structured framework to identify and assess factors influencing a proposed change, helping project teams make informed decisions (Klonek, Lehmann-Willenbrock and Kauffeld, 2014). Identifying crucial aspects that will impact the project’s progress, the Force Field Analysis plays a pivotal role in “Enhancing Regular Dental Checkups among Black Ethnic Minorities in London.” The combination of examining driving and constraining factors enables the creation of targeted approaches to enhance the odds of reaching the project’s objective — securing equal dental treatment opportunities for Black cultural minorities living in London.
Integrating Force Field Analysis and Change Theory clarifies how drives and obstacles interact (Burnes, 2020). According to Dawson (2014), Lewin’s groundbreaking methodology encompasses freeze, modify, and reform steps for successful transition management. Unfreezing encompasses raising awareness regarding the necessity for modification/change; fostering a feeling of pressing importance through the spotlight on dental well-being inconsistencies. Amidst these transformations (changing phase), the project will contrive and execute measures to address restraining and enhancing driving forces. Consistent action transforms change into concrete reality by freezing new standards surrounding regular dental maintenance inside Black racial/ethnic minority groups.
| Driving Forces | Score (1-5) |
INCREASING THE PERCENTAGE OF REGULAR DENTAL VISITS AMONG BMEs IN LONDON |
Restraining Forces | Score (1-5) |
| 1. Public Health Imperative | 4 | 1. Cultural Misconceptions | 4 | |
| 2. Evidence-Based Outcomes | 5 | 2. Language and Communication Barriers | 3 | |
| 3. Cultural Competency Advocate | 3
|
3. Resource Constraints | 2 | |
| 4. Collaborate Partnerships | 4 | |||
| TOTAL | 25 |
The Force Field Analysis Table
An extensive depiction of how these factors impact this project appears in the Force Field Analysis graphical representation above. Between ratings of 3 and 5, notable motivational elements (driving elements) that inspire this undertaking emerge- including a vital public health necessity, scientifically supported results, campaigning for culturally sensitive approaches, and cooperative alliances. From low scores (2-4) emerge the hurdles obstructing advancement, including cultural misperceptions, communication gaps, and scarce assets. Based on a total score of 25, a supportive atmosphere is conducive to transformation, indicating a promising prospect for successful implementation if suitable tactics are implemented to boost driving factors while counteracting hindering ones.
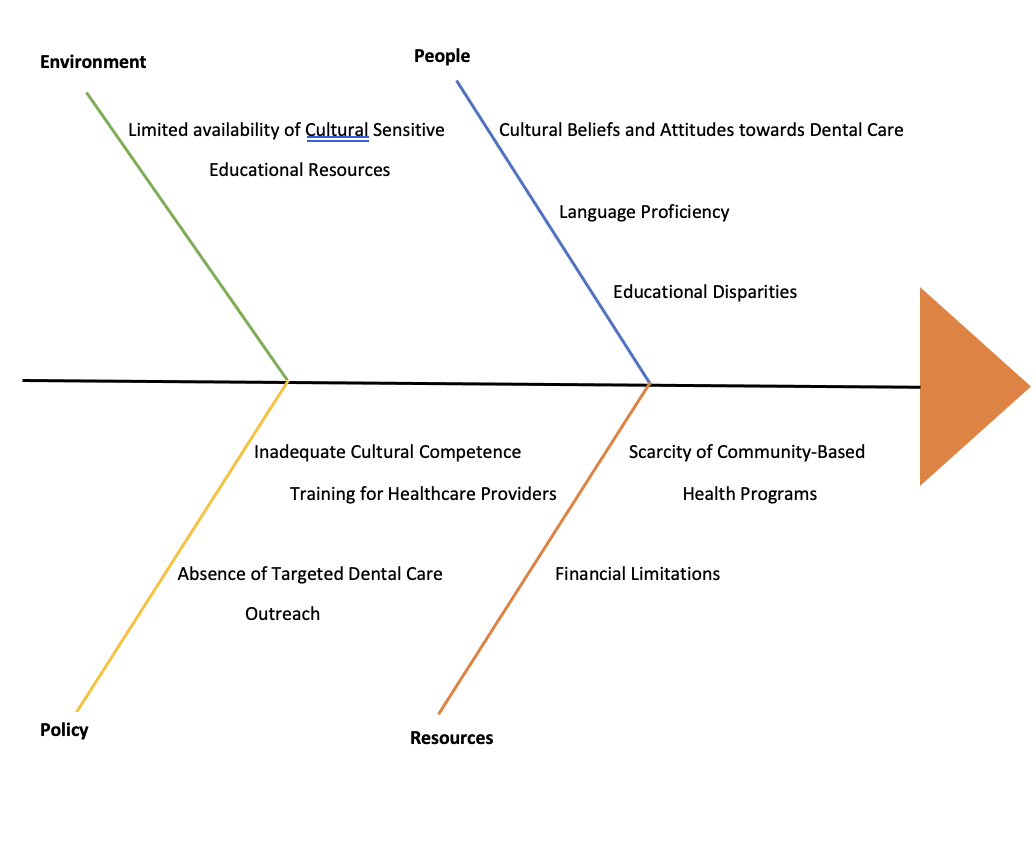
Fishbone Diagram Analysis of Root Causes
The Fishbone Diagram, also known as the Ishikawa or Cause-and-Effect Diagram, is a visual tool employed to dissect and analyse the root causes of a specific issue (Loredana, 2017). Within the framework of the project of boosting regular dental checkups among ethnic minority groups in London, the Fishbone Diagram was employed to investigate the paramount hindering element—Cultural Misconceptions. Specifically, examining the “People” component of the graphic organiser revealed relevant factors such as cultural perceptions regarding oral health, linguistic competency, and knowledge disparities. Under this dimension, we observed deficiencies in provider preparedness through ineffective cultural competency programs. The educational resource scarcity extends beyond cultural sensitivity, falling under the purview of the “Environment”. In this regard, the “Resources” portion sheds light on the economic challenges and sparse supply of area-based medical services. Its significance lies in offering a thorough structure to handle complicated problems such as culturally ingrained misunderstandings. It allows focused endeavours to reframe perceptions, expand accessibility, and adapt oral health programs catering to Black ethnic minority populations.
Project Goal and Objectives
The overarching goal of the project cornerstone revolves around promoting more frequent oral checkups amongst this demographic in London. This objective is tied intimately with the results of the Force Field Analysis and Fishbone Diagram assessment. Through carefully crafted interventions, we aim to drive a cultural revolution centred around promoting oral hygiene practices and enhancing access to preventive dental care. Promoting consistent dental attention will lead to more robust oral well-being and diminished differences in medical health.
Stakeholders and Anticipated Conflict
With multiple parties involved having competing agendas and passions, navigating this complex landscape will require careful management. Enhancing wellness across this demographic, increased dental visit opportunities cater specifically toward elevating oral care standards. These professional groups prioritise ensuring uniform care for individuals across demographics, promoting a fair system. In particular, public health organisations within London, such as the London Borough Public Health Teams, Healthwatch London, and the Greater London Authority’s Health Team, are expected to play an instrumental role. Advocacy, resource coordination, data sharing, and policy alignment will form the foundation of their integration, ensuring a smooth implementation across all healthcare service delivery systems within London’s varied populations. However, stakeholders’ diverse concerns and conflicting ambitions complicate decision-making processes within this expansive landscape. By aligning various viewpoints, we foster durable growth through effective collaboration.
| Stakeholder Group | Involvement |
| Black Ethnic Minority Communities | Beneficiaries; Active engagement and feedback |
| Primary Healthcare Providers | Participants; Integration of dental care into the broader healthcare |
| Local Authorities and Government Bodies | Participants; Policy formulation and resource allocation |
| National Health Service (NHS) Dental Services | Participants; Infrastructure and resource support |
| Educational Institutions and Research Centers | Participants; Research expertise and evaluation support |
| Community and Non-Governmental Organisations (NGOs) | Participants; Grassroots outreach and awareness campaigns |
Project Planning and Feasibility
Main Activities and Evidence-Based Interventions
- Cultural Competence Training for Healthcare Providers: Design practical courses based on facts for oral experts, focusing on understanding various cultures and verbal exchange excellence. Required expertise: Dental educators and cultural competence trainers. Responsible parties: Academic institutions and dental associations. Involvement: Fifteen educational professionals dedicated to dentistry and two experts in cultural sensitivity training.
- Culturally Tailored Educational Campaign: We must design a successful campaign promoting habitual dental appointments by tailoring our messaging to various language communities. Required expertise: Medical professionals, visual artists, and language specialists. Responsible party: Public health organisations, NGOs. Involvement: Five public health professionals, two graphic artists, and three language specialists.
- Community Workshops and Outreach: Join forces to coordinate educational seminars facilitated by neighbourhood figures to correct fallacies and promote good oral care practices. Required expertise: Community organisers and oral health educators. Responsible party: Local community organisations and dental schools. Involvement: Eight community leaders joined forces with four oral health specialists.
- Enhanced Dental Clinic Accessibility: Creating separate medical wings inside neighbourhood gathering places allows for simpler patient navigation. Required expertise: Dentists, clinic administrators. Responsible party: These two institutions provide complementary dental care options—involvement: 10 dentists and two clinic administrators.
Gantt Chart and Relevance
Visualising the project’s trajectory via a timeline, milestones, and connections, a Gantt chart serves as a blueprint for streamlined administration (Grant, 2022). Spanning six months, this initiative smoothly aligns tasks through coordinated efforts, facilitates progress monitoring, and enables prompt modifications. The Chart assumes great importance by promoting dependable tracking, effective planning, and concerted efforts to accomplish the stated aspirations.
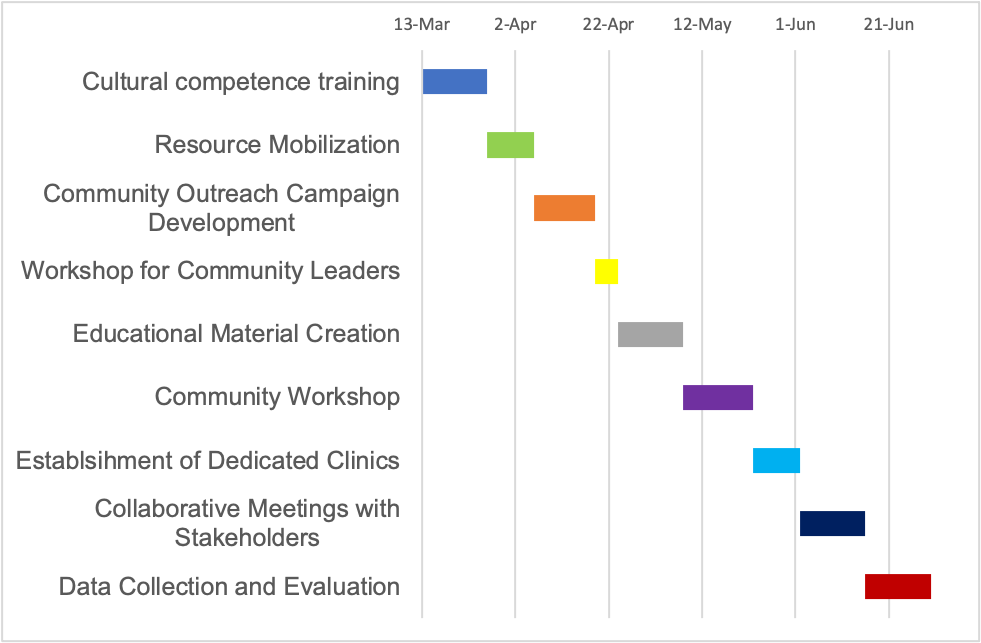
Gantt chart
Risk Analysis and Mitigation Approaches
Through extensive research into possible obstacles, the intricate evaluation of risks for this venture continues with precision. This endeavour involved engaging stakeholders, conducting resource assessments, and delving into community dynamics to unearth potential risks that could impede the project’s progress. One significant risk that emerged from stakeholder discussions is the possibility of encountering community resistance to change. Traditional attitudes and behaviours within communities may impede the adoption of routine dental care. To mitigate this, a phased implementation strategy will be adopted to first pilot smaller group sessions to educate patients about the advantages of proactive oral healthcare before scaling up the initiative’s efforts. Furthermore, esteemed individuals within the community will serve as champions to address concerns and facilitate harmony between long-standing values and project goals.
Another risk highlighted through rigorous resource assessment is the potential shortfall in funding, which could limit the scope of project activities. In addressing this issue, the project group will explore various financial backing options through cooperation with public health groups and nonprofit foundations. Furthermore, a cushion fund will mitigate unforeseen resource shortfalls, allowing crucial tasks to persist unhindered.
Meetings with neighbourhood figures showed dental treatment issues could impact involvement levels and active support. Multiple language support will prominently tackle this hurdle through strategically designed communication materials. Within societal parameters, these materials underline how essential precautionary dental treatment is. Teaming with influential community members helps bridge the gap between our project’s mission and their cherished beliefs.
Stakeholders’ Prioritisation Analysis
Stakeholder prioritisation involves categorising stakeholders based on their influence and interest. Key stakeholders like Black ethnic minority communities, primary healthcare providers, and public health organisations are prioritised for tailored engagement. Communication strategies involve regular feedback loops, community forums, and interactive workshops to ensure alignment and engagement.
Communication and Engagement Plan
Through effective communication, this diverse array of actors/stakeholders is linked by a robust bridge spanning multiple domains. By clear messaging, project objectives, and targeted content, communication fosters collective comprehension, ensures stakeholders remain aligned and enhances project influence. This eventually guides the initiative toward successful implementation, supporting its ultimate purpose of expanding dental care access and promoting awareness among disadvantaged populations (Brady, Goins and Young, 2019; Doten-Snitker et al., 2021).
| Stakeholder Group | What to Communicate | When | How |
| Black Ethnic Minority Communities | Benefits of routine dental visits, debunking myths | Throughout the project duration | Community workshops, culturally tailored materials |
| Primary Healthcare Providers | Project goals, cultural competence training | Prior to training sessions, quarterly | Webinars, presentations, informational materials |
| Local Authorities and Government Bodies | Project objectives, impact on health equity | At project launch, bi-annually | Reports, presentations, policy discussions |
| National Health Service (NHS) Dental Services | Collaboration opportunities, project updates | Regularly, as milestones are achieved | Meetings, reports, email updates |
| Community and Non-Governmental Organisations (NGOs) | Collaborative initiatives, campaign details | Ongoing, as activities are planned | Joint meetings, workshops, shared resources |
| Educational Institutions and Research Centers | Project significance, research opportunities | At project initiation, quarterly | Seminars, conferences, research partnerships |
Project Implementation and Monitoring
A critical stage marks the shift from project planning to execution. Shifting attention with precision allows the successful implementation of intricately planned projects. A structured approach will be adopted to facilitate this transition to ensure a smooth handover of responsibilities, clear communication channels, and a heightened sense of purpose among team members.
One significant undertaking during the execution and surveillance phases is the “Cultural Competency Training session” aimed toward health practitioners; efficient direction necessitates adopting transformational leadership methods. This approach stimulates cooperation while bolstering team members’ confidence and promoting a collective investment in the project’s success (Coun, Peters and Blomme, 2019). Amidst this initiative lie efforts to narrow the gap between quality dental care for diverse groups, prioritising Black ethnic minorities’ needs above all else. Given its spotlight on joint initiatives, delegated authority enhancement, and group motivation, transformative leadership is particularly suited to overcome this obstacle. This leadership style reinforces the importance of inclusion and cultural sensitivity, fundamental values consistent with the project’s vision.
Transformational leaders foster individual growth and a unified vision and motivate their followers toward success (Hetland et al., 2018). By adopting this management model, healthcare practitioners may enhance dental services and assume the role of influential ambassadors for progress nearer to home. Leadership that transforms creates feelings of possession and accountability among healthcare workers, leading them to proactively support efforts to encourage regular dental checkups among Black racial minority groups, enhancing the campaign’s reach. Additionally, this undertaking resonates strongly with the transformative leader’s proclivity to encourage open communication and empathic relationships. Active listening and inclusivity allow transformational leaders to form robust relationships with community members and address disparities effectively. The project’s ultimate aim aligns deeply with tackling cultural myths and rallying participation from the community.
The Gantt chart and communication plan will be adapted accordingly when the selected activity faces unforeseen delays or requires additional resources. This will necessitate the creation of a new timeline and expedited notifications to stakeholders to maintain expectation control. This scenario warrants a participatory leadership model that draws upon group experience and skills via mutual input and consensus.
Leadership and communication skills will play a crucial role in addressing the situation if a risk materialises, such as community resistance due to cultural misconceptions. Leadership transparency and empathy will be crucial in incorporating community voices, eliminating rumours through constructive interactions, and earning genuine goodwill (Mortier, Vlerick and Clays, 2016). Tailoring our messaging accordingly, we aim to increase resonance with the local community. A continuous feedback cycle shall ensure local opinions receive attention and influence plans.
Project Evaluation
According to Herath and Chong (2021), examination of the degree to which the project achieved its goals forms part of the broader process of project evaluation, with particular attention paid to evaluating successful execution throughout the defined timeframe and resource allocation. By implementing this method, we may accurately evaluate the venture’s extensive effects.
Data and information were needed to assess whether the objectives met quantitative and qualitative indicators. Quantitative data includes metrics such as the percentage increase in routine dental visits within the targeted communities. In contrast, qualitative data delves into attitudinal shifts, community engagement levels, and stakeholder feedback (Sturrock et al., 2017). Data sources will include pre-and post-intervention surveys, patient attendance records, and qualitative interviews with community members, healthcare providers, and project team members.
For an accurate evaluation, input from multiple parties involved in communication and leadership is essential (Chatterjee et al., 2017). Providers’ attitudes toward cultural competence training provide insight into their capacity to connect meaningfully with diverse patient groups. Measuring the impact of leadership tactics, the level of acceptance by area inhabitants determines how well we connect with them. These three methods serve as key inputs for obtaining constructive feedback.
The evaluation must examine how their approach aligns with essential project principles and achievements to comprehend project leaders’ efficacy fully. How did the appointed leaders contribute to creating an environment favourable to unity, variety, and respect for differences? Were they instrumental in fostering a productive team environment and active stakeholder participation? By asking these questions, stakeholders will gain insight into both successes and weaknesses inherent for refinement in future initiatives. Additionally, through fostering leadership cohesion, these successful leadership models contribute significantly to enhancing the quality and success of ongoing ventures (Baker, 2020).
Conversely, any discovered gaps or limitations provide enlightening intelligence on how to enhance performance. In light of Hartnell et al.’s (2016) findings, tailoring leadership methods to account for local customs would improve collaboration and increase cross-cultural understanding. Moreover, the review examines the depth of influence these leadership styles have on team collaboration and stakeholder commitment. Project success relies heavily on wholehearted participation and steadfast resolve exhibited by diverse players across healthcare providers, civic groups, governments, and independent organisations. According to Cote (2017), excellent leaders instil a collaborative spirit, increasing productivity and joint success through mutual understanding and commitment.
While the project holds immense potential for positive change, it is important to acknowledge its limitations. Although carefully planned, the timeline of 5 months may have posed constraints on the depth of community engagement and attitudinal shifts. Furthermore, unpredictable community interactions or limited resources may have influenced project results. Realising these constraints is the basis for enhancing performance through practical experience gained via lessons learned.
Conclusion
In conclusion, the journey undertaken in pursuit of increasing regular dental visits among Black ethnic minorities in London has shed light on both the importance of accessible healthcare and the profound impact of effective project management. Evidence of successful teamwork heightened awareness of cultural nuances, and transformative executive direction have all contributed to meaningful evolution within these disadvantaged groups. Lessons learned through this venture will resonate well outside its initial bounds. Following this experience, I am well-prepared to inject novel understandings into my existing domain. Clear communication, active stakeholder involvement, and flexibility significantly shape my response to projects and obstacles. Determined to refine my project management abilities by carefully applying learned lessons, I seek to implement them seamlessly into my work environment.
Additionally, the insights acquired on this expedition are a treasured commodity that I hope to distribute. Committed to instilling best practices throughout my team, I share insightful lessons learned through collaborative experiences. My mission is to empower others through interactive training sessions, tailored mentorship, and established standards of excellence in project management, ensuring they possess the capabilities to excel in this field with assurance and sophistication. Its transferability goes far beyond its unique circumstances; relevant across numerous domains. These principles may easily be adaptable across diverse public health campaigns. This project’s well-designed structure is a comprehensive foundation for effectuating positive changes across numerous fields, including boosting immunisation levels, promoting public health awareness, and campaigning for proactive medicine.
Bibliography
Access to NHS dental services., 2022. ethnicity-facts-figures.service.gov.uk. Available at: https://www.ethnicity-facts-figures.service.gov.uk/health/patient-experience/access-to-nhs-dental-services/latest.
Arora, G., Mackay, D.F., Conway, D.I. and Pell, J.P., 2016. Ethnic differences in oral health and use of dental services: a cross-sectional study using the 2009 Adult Dental Health Survey. BMC Oral Health, [online] 17(1). https://doi.org/10.1186/s12903-016-0228-6
Baker, B., 2020. Power, leadership and culture as drivers of project management. American Journal of Management, 20(1), pp.9-30. http://www.m.www.na-businesspress.com/AJM/AJM20-1/1_BakerB_20_1_.pdf
Brady, A., Goins, R. and Young, M., 2019. Sharing Results. https://www.urban.org/sites/default/files/publication/99636/sharing_results_a_guide_for_communicating_promise_neighborhoods_outcomes_to_diverse_audiences_0.pdf
Burnes, B., 2020. The origins of Lewin’s three-step model of change. The Journal of Applied Behavioral Science, 56(1), pp.32-59. https://journals.sagepub.com/doi/pdf/10.1177/0021886319892685
Charadram, N., Mankiewicz, S., Maggi, S., Petrovic, M., Kossioni, A., Srinivasan, M., Schimmel, M., Mojon, P., Müller, F., e‐Delphi working group and Soiza, R.L., 2021. Developing a European consensus from dentists, dental hygienists and physicians on a standard for oral health care in care‐dependent older people: An e‐Delphi study. Gerodontology, 38(1), pp.41-56. https://aura.abdn.ac.uk/bitstream/handle/2164/17362/Charadram_et_al_Gerodontology_DevelopmentOfACnsensus_AAM.pdf?sequence=1
Chatterjee, R., Suy, R., Yen, Y. and Chhay, L., 2018. Literature review on leadership in healthcare management. J Soc Sci Stud, 5(1), pp.38-47. https://www.vumc.org/faculty/sites/default/files/Healthcare%20Leadership%20Review.pdf
Cote, R., 2017. The vision of effective leadership. International Journal of Business Administration, 8(6), pp.1-10. https://www.academia.edu/download/57898223/Leadership_in_Aviation.pdf
Coun, M.J., Peters, P. and Blomme, R.J., 2019. ‘Let’s share!’The mediating role of employees’ self-determination in the relationship between transformational and shared leadership and perceived knowledge sharing among peers. European Management Journal, 37(4), pp.481-491. https://www.academia.edu/download/86651416/j.emj.2018.12.00120220529-1-1pv4j2l.pdf
Currie, C.C., Araujo‐Soares, V., Stone, S.J., Beyer, F. and Durham, J., 2021. Promoting regular dental attendance in problem‐orientated dental attenders: A systematic review of potential interventions. Journal of Oral Rehabilitation, 48(10), pp.1183–1191 https://doi.org/10.1111/joor.13244.
Dawson, P., 2014. Reflections: On time, temporality and change in organisations. Journal of Change Management, 14(3), pp.285-308. https://www.tandfonline.com/doi/pdf/10.1080/14697017.2014.886870
Doten-Snitker, K., Margherio, C., Litzler, E., Ingram, E. and Williams, J., 2021. Developing a shared vision for change: Moving toward inclusive empowerment. Research in Higher Education, 62, pp.206-229. https://par.nsf.gov/servlets/purl/10149361
Hartnell, C.A., Kinicki, A.J., Lambert, L.S., Fugate, M. and Doyle Corner, P., 2016. Do similarities or differences between CEO leadership and organisational culture have a more positive effect on firm performance? A test of competing predictions. Journal of Applied Psychology, 101(6), p.846. https://psy482.cankaya.edu.tr/uploads/files/Similarities%20or%20Differences%20Between%20CEO%20Leadership%20and%20Culture.pdf
Herath, S. and Chong, S., 2021. Key components and critical success factors for project management success: A literature review. Operations and Supply Chain Management: An International Journal, 14(4), pp.431-443. https://journal.oscm-forum.org/journal/journal/download/20210906130104_Paper_4_Vol._14_No_._4,_2021_.pdf
Hetland, J., Hetland, H., Bakker, A.B. and Demerouti, E., 2018. Daily transformational leadership and employee job crafting: The role of promotion focus. European Management Journal, 36(6), pp.746-756. https://www.sciencedirect.com/science/article/pii/S0263237318300021
Klonek, F.E., Lehmann-Willenbrock, N. and Kauffeld, S., 2014. The dynamics of resistance to change is a sequential analysis of change agents in action. Journal of change management, 14(3), pp.334-360. https://research.vu.nl/files/824901/Klonek,%20Lehmann-Willenbrock%20+Kauffeld%202014%20Dynamics%20of%20Resistance%20to%20Change.pdf
Lewin, K. and Cartwright, D., 1951. Field Theory in Social Science: Selected Theoretical Papers. Social Service Review, 25(3), pp. 409–410. Available at: https://ia802905.us.archive.org/4/items/in.ernet.dli.2015.138989/2015.138989.Field-Theory-In-Social-Science-Selected-Theoretical-Oaoers.pdf
Loredana, E.M., 2017. The analysis of a phenomenon’s causes and effects through the “fishbone” diagram. Ann Econ Ser, 5, pp.97-103. https://www.utgjiu.ro/revista/ec/pdf/2017-05/11_Ecobici%20Loredana.pdf
Marshman, Z., Nower, K. and Wright, D., 2013. Oral health and access to dental services for people from black and minority ethnic groups. [online] Available at: https://raceequalityfoundation.org.uk/wp-content/uploads/2022/10/health_briefing_29-1_0.pdf.
Mortier, A.V., Vlerick, P. and Clays, E., 2016. Authentic leadership and thriving among nurses: The mediating role of empathy. Journal of Nursing Management, 24(3), pp.357-365. https://www.researchgate.net/profile/Anneleen-Mortier/publication/281058213_Authentic_leadership_and_thriving_among_nurses_The_mediating_role_of_empathy/links/607eb3ee2fb9097c0cf79571/Authentic-leadership-and-thriving-among-nurses-The-mediating-role-of-empathy.pdf
Steinvik, L.M., Svartdal, F. and Johnsen, J.A.K., 2023. Delay of Dental Care: An Exploratory Study of Procrastination, Dental Attendance, and Self-Reported Oral Health. Dentistry Journal, 11(2), p.56. https://www.mdpi.com/2304-6767/11/2/56
Sturrock, A., Cussons, H., Jones, C., Woodcock, C. and Bird, L., 2017. Oral health promotion in the community pharmacy: an evaluation of a pilot oral health promotion intervention. British Dental Journal, 223(7), pp.521-525. https://www.nature.com/articles/sj.bdj.2017.784
 write
write