Visual Representation of the Impacts of Determinants on Health
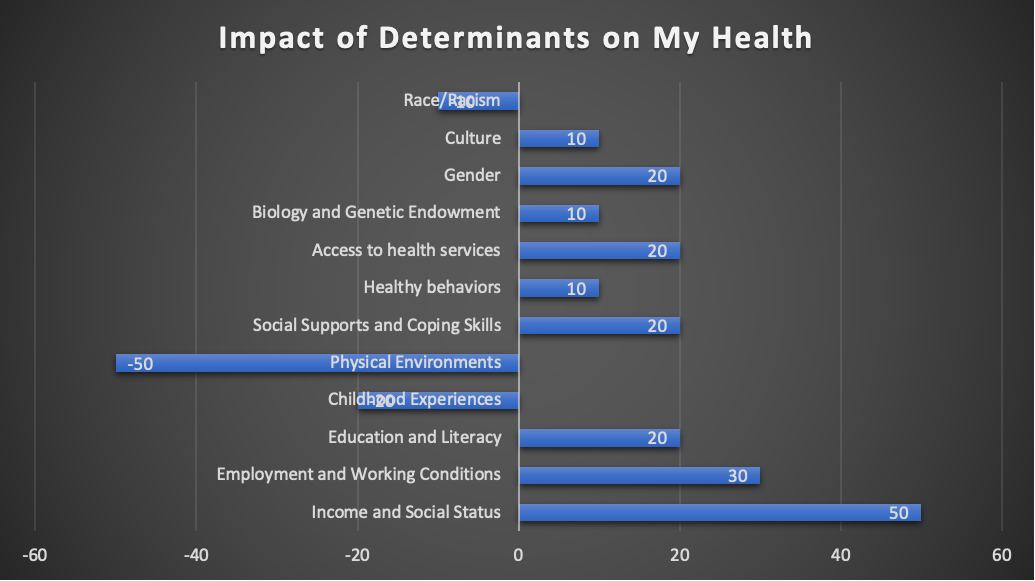
Examples of How the Determinants Affect Health
Income and Social Status
Income and social status have the most significant and most positive impact on my health. I come from a reasonably wealthy background, which positively impacts my life. Research has shown a significant correlation between income and the risk factors for chronic disease (National Academies of Sciences, Engineering and Medicine, 2018). For instance, individuals who come from families that receive low incomes are at a significant risk of hypertension, diabetes, stroke, and heart disease. They are often victims of at least four chronic diseases during their lifetime.
Further research reveals that individuals who come from families that have less than two hundred percent of the federal poverty level are usually at a greater likelihood of being obese as compared to other individuals (National Academies of Sciences, Engineering, and Medicine, 2018). These people are also more likely to be cigarette smokers than wealthy individuals. Instances of psychological distress have also been reported to be significantly higher in adults who live in poverty.
The explanation is that when someone has economic resources such as wealth and income, they have access to services and material goods such as healthcare. A study conducted between 2009 and 2010 found out that individuals aged between eighteen and sixty-four from all races had a greater likelihood of delaying seeking or getting medical care because of the associated costs (National Academies of Sciences, Engineering, and Medicine, 2018). This number has since increased over the years. As families’ incomes increase, there is a corresponding decrease in the number of people failing to get medical care.
Further research also shows that poor people have more difficulty getting to the emergency department than rich people. According to a study conducted in 2014, 28.6 percent of adults living below the poverty line had one or more visits to the emergency department, and 13.5 percent of those at a four hundred percent poverty level (National Academies of Sciences, Engineering, and Medicine, 2018). While people below the poverty level got hospital access, they often reported delayed medical treatment, failure to obtain prescription drugs, and not receiving dental care because of the high costs. Accordingly, there is still lower access to healthcare services for people with low incomes even when they utilize highly hospital and emergency services.
Employment and Working Conditions
Employment and working conditions also affect one’s health positively or negatively. Issues surrounding this include bullying and discrimination in the workplace, stress, workplace injury, dissatisfaction with the job, accidental death, violence, and retrenchment. When an individual works for long hours with a heavy workload and job insecurity, it may largely contribute to their health instability. Work-related stress comes from conflicts with co-workers, job insecurity, heavy workloads, and long hours. Constant dealing with work issues beyond the employee’s control may significantly impact their health by increasing the risk of health issues such as depression and anxiety.
Another perspective of employment and the working benefits that come with it are insurance and the employee’s ability to pay. When an employee has a good job, they will get medical insurance, too, and the ability to pay in case of other illnesses not covered by the insurance. Medical care becomes a significant hurdle for individuals with low incomes and jobs that come without insurance (Henry & KFF, 2016). In my case, my job comes with insurance on all my medical needs, which ensures that I can go for check-ups as well as treatment at all times. This has positively affected my health.
Physical Environments
The physical environment in which one resides also significantly affects one’s health outcomes. When one lives in a city full of concrete buildings and no pathways, they will not have a place to exercise, which will significantly contribute to obesity and the health outcomes associated with it (Ajayi & Amole, 2022). Lopez and Hynes (2006) sought to determine the relationship between the built environment, physical activity, and obesity. They discovered that various features of the sub-urban built environment, such as the lack of sidewalks, poor street connectivity, and low densities, are associated with decreased physical activity, ultimately increasing the risk of being overweight. Residents that live in inner cities also reported significantly higher obesity rates as compared to those that live in the sub-urban.
I live in the inner city, where there are no walkways. Movement is entirely by cars, meaning we never have the chance to exercise and keep our bodies fit. There are also no parks and open spaces. If I am to exercise, I have to travel long distances outside the city, which is sometimes very expensive. As a result, I rarely do so. The physical environment that I reside in, therefore, affects my health negatively as it puts me at risk for obesity and related illnesses.
Race/Racism
Racism is another determinant of health across many countries. Individuals who come from minority communities are often faced with racism during their attempts to access medical care, which negatively impacts their health. Canada is one of the world’s most diverse nations with different races. Nonetheless, access to healthcare is unequal for some races, such as Asian Americans, Pacific Islanders, American Indians, people of Hispanic origin, and Black people. These individuals are often pushed to live in disadvantaged neighborhoods and also attend schools that are inadequately resourced. This results in lower educational attainment (Braveman et al., 2014). As a result, they are often victims of infectious diseases, chronic and disabling sicknesses, and high mortality rates as compared to white Canadians. Minority groups also significantly face difficulty in accessing medical care as compared to whites.
Statistics have revealed further that black adults experience earlier onset for various illnesses as well as greater severity and rapid progression of the diseases. The levels of impairment throughout their life course, as well as comorbidity, are also significantly higher as compared to whites above the age of sixty-five. The same statistics are accurate for Latinos, Asian populations with low socioeconomic status, Pacific Islanders, and American Indians (William & Wyatt, 2015). Many minority groups sometimes feel that if they had someone with the same ethnicity or racial identification in a hospital, they would be more likely to visit the premises as compared to the current state.
As a Canadian minority, I often experience some disparities in access to healthcare, such as those described above. Sometimes, I have to queue for long hours before I can get treatment, unlike most of my peers. The area I live in also has lower-level medical facilities than other areas in the city. Nonetheless, this impact is not very huge. Eventually, they will be able to access healthcare.
Health Promotion Strategies
Physical Environments
Health promotion strategies that can be implemented regarding physical environments include incorporating open spaces around buildings we reside in. I want to clear up the rooftop of my house to create space for exercise. I will also create some walkways around the house so that I can move around and perform exercises. I will also install a home gym so that I can perform some exercises that will go a long way in helping me get fit. This will help me overcome obesity and related illnesses such as hypertension, high blood pressure, and heart disease that I am currently at risk of getting.
Income and Social Status
Regarding income and social status, I intend to work on increasing my income further to access higher peaks of medical services. I intend to do this by opening a business. This business will be in the food industry, whereby I will be selling cookies online. Once the business has gained significant mileage to increase my income tremendously, I can access more health services. Some serious illnesses, such as cancer, are very expensive and may prove to be difficult for me to access at the moment. However, if I increase my income according to this strategy, I will have better access to health care regarding income and social status.
Reflection
This reflection has taught me a lot about health and health determinants. I have learned that health is affected by different issues, such as where an individual stays, the color of their skin, and how much they earn. These different factors contribute positively or negatively to the individual’s health situation. This analysis taught me that individuals could improve their health by improving these single determinants. For instance, by changing one’s diet, one can avoid the risk of becoming obese and thus avoid the associated risks of obesity, such as hypertension, high blood pressure, and heart disease. I have also learned that social structures such as racism negatively impact the health of many people across the country. Individuals from minority races are at a greater risk of getting chronic illnesses because of the areas in which they live, the food that they eat, and their difficulty in obtaining healthcare. From this information I have obtained, I will understand my patients’ surroundings and their impact on their health. It will be easy for me to recommend health promotion strategies to them, thus improving their overall health status in the long term.
References
Ajayi, A. O., & Amole, O. O. (2022). Open spaces and wellbeing: the impact of outdoor environments in promoting health. Cities & health, 6(6), 1106–1121.
Braveman, P., & Gottlieb, L. (2014). The social determinants of health: it is time to consider the causes of the causes. Public health reports, 129(1_suppl2), 19-31.
Henry, J., & Kaiser Family Foundation. (2016). Key facts about the uninsured population.
Lopez, R. P., & Hynes, H. P. (2006). Obesity, physical activity, and the urban environment: public health research needs. Environmental Health, 5(1), 1–10.
National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Care Services; Committee on Health Care Utilization and Adults with Disabilities. Healthcare Utilization as a Proxy in Disability Determination. Washington (DC): National Academies Press (US); 2018 Mar 1. 2, Factors That Affect Healthcare Utilization. Available from: https://www.ncbi.nlm.nih.gov/books/NBK500097/
Williams, D. R., & Wyatt, R. (2015). Racial Bias in Health Care and Health: Challenges and Opportunities. JAMA, 314(6), 555–556. https://doi.org/10.1001/jama.2015.9260
 write
write