Problem Statement
Hospital workers are dissatisfied with increasing workload, poor patient care, and healthcare system pressure. The nationwide nurse deficit, aggravated by the COVID-19 epidemic, is to blame. A 1.1 million-nurse deficit was expected as over 500,000 nurses left the profession by year’s end (Haddad, Annamaraju, & Toney-Butler, 2023). This scarcity is caused by high retirement and turnover rates for experienced and new R.N.s. While an 800,000-nurse deficit was forecast by 2020, the age of working nurses was also an issue. Marć et al. (2018) found that over a million nurses over 50 will retire over the next decade. Smiley et al. (2018) also found that 33% of LPNs over 55 will retire, raising worries about nursing shortages in 10 years. According to a study by An et al. (2022), a significant proportion of newly employed nurses, precisely 33% within the initial year and potentially up to 56% within the subsequent year, choose to discontinue their employment. High retirement and turnover rates among R.N.s contribute immensely to the country’s nurse shortage issue.
One of the ways the American Nurses Association (ANA) and AHA are solving the problem of nurse shortage in the country is by incorporating new registered graduate nurses into the system. Graduate nurses constitute the most substantial pool of registered nurses (R.N.s) accessible for recruitment at a national level. However, newly graduated nurses encounter numerous obstacles as they assimilate into the professional culture of their respective healthcare settings, which results in poor turnover and retention of new R.N.s (An et al., 2022). Numerous elements impact the decision of newly graduated nurses to depart from the nursing profession. These nurses encounter a multitude of problems when entering the workforce. These included, among others, a need for more effective leadership. Nurses are shown to develop emotional exhaustion, which negatively affects the turnover rate when nursing leaders do not exhibit emotional intelligence in modulating work culture (Majeed & Jamshed, 2021). Other factors included an unfavourable work atmosphere, limited opportunities for empowerment, and a lack of mentorship.
The assumption is that if the problem of high turnover rate among new R.N.s is not addressed promptly, the overall health of Americans will continue to deteriorate despite the billions of dollars invested in the healthcare industry. This problem puts tremendous strain on the already stressed nursing profession to train more nurses quickly (Lowman & Harms, 2022). Even with quick training, there is no assurance that the issue of nurse shortage will be resolved because new nurses will continue to exist within the first or second year of professional practice. Because the average financial burden of turnover for an organization can reach a substantial amount ranging from $5.9 million to $6.4 million, it is imperative to prioritize the retention of newly hired nurses and facilitate their smooth integration into the professional practice.
Several solutions have been suggested to address the issue of employee turnover among new graduate nurses and improve retention. One of the solutions is incorporating and enabling new nurses to complete a nurse residency program. The context focuses on analyzing how the program can improve the retention of new R.N.s who often face challenges that make most of them quit within the first year or two of professional practice. Participation in a nurse residency program would equip nurses with resilience and skills to perform successfully in challenging work environments. The study relates to the following PICOT question: In newly graduated nurses (P), how does participation in a nurse residency program, compared to not participating in such a program (C), influence job retention rates within the first two years of professional practice (O)? What specific challenges and facilitators do nurses encounter in their initial years of professional practice (T)?
Population and Setting
The study targets recent nursing graduates with fewer than two years of experience. Nurses with less than two years of professional nursing experience are crucial to the healthcare workforce because they must transition from academic training and adapt to professional nursing environments. This study occurs in hospitals, clinics, and other healthcare facilities where freshly graduated nurses work. By covering multiple contexts, the research study may thoroughly examine NRPs’ performance in different professional environments and assist nurses in transitioning and retaining jobs in their first two years.
Overview of Intervention
NRPs may lower new nurse turnover. NRP is intended for nurses with less than 12 months of experience and is expected to be completed in the first year. The NRP emphasizes educational and personal abilities to help students transition into professional nursing (AbuAlRub & Abu Alhaija’a, 2019). The curriculum includes live lectures, interactive discussion boards, online learning modules, and exercises. These components promote local and system-wide content specialist involvement.
These initiatives help new R.N.s and the healthcare business. First, NRPs foster critical thinking and evidence-based clinical decision-making. Second, they improve clinical nurse leadership, communication, and practice safety. New nurses get tailored development packages via the project. It boosts nurse satisfaction, professional devotion, and teamwork. Finally, it develops clinical decision-making skills and confidence (AbuAlRub & Abu Alhaija’a, 2019). The NRP will affect new nurses, patients, and the healthcare industry, making it successful.
Despite all these benefits, there are still some potential challenges that the effort may have to overcome. One of the main challenges this initiative will likely encounter is a need for more time for the nurses and time management. The newly qualified nurses will likely need help effectively organizing their workflow and efficient time management during their shifts. Managing many tasks for a group of patients can be a daunting task. Moreover, novice nurses may need more prioritization and delegation skills regarding non-nursing responsibilities.
Consequently, increased nurse-to-patient ratios harm time management and organizational abilities (AbuAlRub & Abu Alhaija’a, 2019). More proficiency in time management can engender a sense of disarray and impede the provision of superior patient care. Another challenge may be a need for more commitment from the new nurses. If a nurse is not interested, they will hardly be committed to the program, and it would be difficult for the leaders of NRP to get them on board or have them complete the program.
Comparison of Approaches
In this research project, NRPs will be compared against non-participation by freshly graduating R.N.s. If R.N.s do not engage in organized residency programs, they may have learning issues, inadequate support, and trouble transferring from academic to professional nursing practice. However, joining an NRP would provide R.N.s with a structured framework to address these difficulties and provide focused education, mentoring, and support in the early phases of nursing. Such programs also help freshly minted nurses transition, improving retention and turnover.
Initial Outcome Draft
Implementing NRPs is expected to improve nurse retention rates and other positive impacts. NRPs have demonstrated efficacy in providing enhanced support to novice nurses, facilitating their professional growth and equipping them with the necessary skills to mitigate attrition rates. Nurse residency programs are crucial in facilitating a smooth and effective transition into professional nursing practice for newly graduated nurses. They lead to job satisfaction, empowerment, organizational commitment, and confidence among new graduate nurses.
According to VanCamp and Chappy (2017), nursing leaders and executives have estimated that a mere 10% of newly graduated nurses are successfully prepared to integrate into the nursing industry. The existing body of literature suggests that Nurse Residency Programs (NRPs) play a crucial role in facilitating the transition of novice nurses into proficient professionals by offering supplementary organization and training. As a result, NRPs push the preparedness percentage from 10% to over 50% (VanCamp & Chappy, 2017). The outcome is often minimal turnover intention and better new nurse retention rates. Therefore, integrating NRPs into the U.S. healthcare system will significantly improve retention rates for new R.N.s.
Time Estimate
The research suggests that developing an NRP program that achieves the expected results may take six months. The NRP establishes organizational structures and uses an accredited framework to develop the residency program. The research project will evaluate NRPs’ effects on newly graduating nurses’ work retention rates. The research project would cover the first two years of professional practice for NRP nurses to assess its efficacy in resolving employment retention difficulties early in their careers. The research will examine the immediate and intermediate impacts of NRP involvement on Newly Graduated R.N. retention in the first two years.
Literature Review
Recent studies have shown that residency programs (R.P.s) help newly minted nurses maintain knowledge and skills. Using an integrated literature review, Asber (2019) examined how NRPs affect nursing graduate retention. This study was needed since the Institute of Medicine recommends using and evaluating NRPs. Nursing executives must evaluate the advantages of a residency program for their business. A comprehensive study of 2010–2016 research on new graduate NRP retention rates found that the 1-year retention rate for newly graduating nurses was above the 74% to 100% national average. National programs like Versant and the University Hospital Consortium/American Association of Colleges of Nursing have more excellent retention rates than organization-based ones.
Knighten (2022) presented Vizient and Versant’s one-year “transition to practice (TTP)” approach, which emphasizes nursing competence evaluation within a specialization. Although first- and second-year nurses had a high turnover rate, the TTP group had 53.4% lower turnover rates than their non-TTP peers (Knighten, 2022). The residency program designed by Vizient and the American Association of Colleges of Nursing (AACN) required an academic-practice relationship between the hospital and a nursing school. It included preceptor-guided clinical encounters, monthly seminars, and small group-guided sessions. The program has a 95% retention rate after one year (Knighten, 2022).
Silvestre et al. (2017) examined residency program ROI and hospital cost savings. The study used a randomized, controlled, multisite design to demonstrate a positive return on investment (ROI) and support the business rationale for a novel graduate Registered Nurse Transition to Practice (TTP) program to reduce turnover. The National Council of State Boards of Nursing (NCSBN) established the evidence-based Transition to Practice (TTP) program with over 35 nursing organizations and other partners. Seventy hospitals and 1032 freshly minted R.N.s participated. 81.2% of newly graduated R.N.s worked in hospitals after one year (Silvestre et al., 2017). This was accompanied by a 15.5% TTP turnover. Additionally, retaining each new graduating R.N. saved $7265.
A comprehensive literature review by Van Camp and Chappy (2017) examined correlations between new graduate NRPs, resident satisfaction, and retention rates to provide perioperative recommendations. New graduates who participated in residency programs had more excellent retention rates and higher orientation satisfaction than those who did not. Residency participants found the program helpful.
Effective residency programs like the University Health System Consortium (UHC)/AACN NRP have strong 10-year retention results. The UHC/AACN NRP pilot began in 2002 and was monitored periodically. In 2002–2004, 88% of UHC/AACN NRP participants stayed in the medical facility after the NRP. This proportion remained at 90.3% till 2007. The 2010 report showed 94.6% retention, while the 2014 report showed 95% retention. Over 33,000 residents have participated since 2002, determining these percentages (Goode et al., 2013).
Retention statistics contrasted graduate nurses who participated in a year-long NRP and those who did not. At one year, 88.9% of NRP participants and 80% of nonparticipants were still hospital employees. Interestingly, the non-NRP group retained more people after 18 months (92.1%) than the NRP group (87.7%). Eighty-seven per cent of nonresident participants still participated after two years, whereas 91% of residents were. The time they increased residents’ probability of remaining at the organization.
Compared NRPs in Magnet-designated and non-Magnet institutions based on retention and perceived competence among freshly graduated nurses with less than a year of acute care clinical experience. The evaluation includes nine quantitative studies from 14 U.S. hospitals and 1585 recent graduates. In the first meta-analysis, NRPs retained 93% of newly graduating nurses in Magnet vs non-Magnet institutions. The second meta-analysis found no difference in NRP effectiveness at Magnet-designated vs non-Magnet institutions. Nurses develop and revise rules that improve practice and patient care at magnet-designated hospitals. Magnet hospitals have better treatment and happier nurses.
Ackerson and Stiles (2018) evaluated NRP research on acute care nurse retention. The Cumulative Index to Nursing and Allied Health Literature, Ovid Nursing Journals, and ProQuest Health and Medical Complete databases yielded 42 articles for full evaluation. Most of the 26 included articles were descriptive. Year-long programs showed excellent retention rates. Retention declined in year two. They examined the impact of a one-year NRP vs a typical orientation on new nurse hire satisfaction and turnover. Systematic reviews and peer-reviewed papers from Medline, Nursing & Allied Health, and CINHAL from 2012 to 2017 were used. NRPs increased new nurse graduates’ satisfaction and retention over a year, suggesting they are more effective than regular orientations.
Trepanier et al. (2012) conducted a cost-benefit study of a multisite NGRN residency program between 2007 and 2010 using turnover rate and temporary nurse utilization data from fifteen community-based healthcare institutions owned by a significant for-profit healthcare organization. From 255 NGRNs before and 39 after residency, the estimated 12-month turnover decreased by $15.2 million (average cost per NGRN turnover of $70,500).
This shows that NRPs reduce new R.N. turnover intentions and rates. Improved nurse turnover rates have also improved healthcare coverage and saved healthcare facilities money. However, the research provided little evidence on how graduate nursing programs affect year-two nursing retention. Further research is needed to assess graduate nursing school nurse retention rates thoroughly.
Intervention Plan
Theoretical Model
In directing the intervention strategy for freshly graduating nurses, Dorothea Orem’s Self-Care Deficit Nursing Theory has both strengths and disadvantages. Its comprehensive approach, stressing the significance of the hospital environment in promoting nurses’ self-care abilities, is a significant strength. The model’s emphasis on education is consistent with the intervention’s objective of improving nursing competence, and it serves as a theoretical framework for educational components within the residency program (Dineen et al., 2019).
Intervention Plan Components
The intervention aims to increase job retention among newly graduated nurses in their first two years of practice (Dineen et al., 2019). Several critical elements of the approach promote health, quality, education, and management. A comprehensive intervention strategy targeting human and organizational issues will reduce high turnover rates for new registered nurses, especially as they move from school to employment. Therefore, the strategy will include;
Pre-employment Engagement
Nursing students will increase employer-educational institution partnership via pre-employment engagement to match curriculum with industry requirements. We will facilitate co-op, internship, and apprenticeship programs to provide students practical experience and a realistic preview of their future duties and responsibilities. It will be like career counselling to assist healthcare workers in establishing realistic job market expectations.
Mentorship and Onboarding Programs
Furthermore, the intervention plan would entail implementing robust onboarding processes aimed towards helping new hires acclimate to the expectations and culture of the workplace. Establishing mentorship programs will also ensure pairing of experienced employees with recent graduates, thereby providing support and guidance.
Professional Development Opportunities
It will be essential to offer continuous professional development and learning programs to assist employees in building new skills and staying engaged. This is because such activities will provide an opportunity and career path for the advancement of the demonstration of long-term commitment to the growth of employees.
Regular Feedback and Recognition besides Flexible Work Arrangements
Introducing flexible work schedules, compressed workweeks, and remote work options will accommodate different preference styles while fostering work-life balance. Moreover, it will be essential to implement regular performance evaluations while providing constructive feedback and recognizing achievements. Such will foster a culture of open communication to address identity areas and concerns for improvement.
Engagement Surveys and Competitive Benefits and Compensation
The sector must maintain competitive benefits and wage packages to recruit and retain top people. Additionally, health initiatives and professional development opportunities may boost work happiness. Regular surveys will be vital to monitor employee happiness, identify improvement areas, and resolve complaints. Feedback helps make data-driven choices and adjust interventions to worker needs.
Stakeholder Needs
Identifying the needs and concerns of important stakeholders such as nurses, educators, healthcare administrators, and mentors is critical. Nurses need a supportive atmosphere, constant education, and mentorship to thrive in the workplace. Educators seek curriculum congruence with real-world difficulties, while workforce stability and excellent treatment are prioritized by healthcare administrators (Jangland et al., 2021). Mentors want established programs to help them lead and assist their mentees. Taking care of these issues enables stakeholder support and active engagement in the intervention.
Alignment with Organizational Goals and Policies
Ensuring that the intervention strategy corresponds with corporate goals and policies is critical for smooth integration into the healthcare system. The strategy should help the firm achieve bigger goals, including worker retention, quality improvement, and adherence to accrediting criteria (Hookmani et al., 2021). Alignment with rules supports regulatory compliance and develops an accountability and transparency culture.
Assumptions
The study presumes that stakeholder demands are correctly recognized through surveys, focus groups, or other input forms. It also implies that the suggested intervention is consistent with the healthcare organization’s overall aims and policies. Furthermore, it implies that healthcare administrators are ready to invest in and support the intervention plan’s execution (Hookmani et al., 2021). Assumptions also include the knowledge that regulatory and governing authorities have standards that influence the intervention’s design and implementation, mandating compliance for the plan to succeed.
Evaluation of The Intervention Plan
An intervention plan was devised based on the following PICOT question: For newly graduated nurses with less than two years of professional nursing experience (P), how does participation in a nurse residency program (NRP) (I) compare to not participating in such a program (C) in influencing job retention rates (O) within a timeframe of six months (T)? The study would involve a 3-month planning and development period, a 6-month nursing residency program (NRP), and a 2-year evaluation period of nurse retention rates.
Implementation Plan
A shortage of nursing personnel across the nation, a predicament that the COVID-19 pandemic has worsened, is an alarming concern that may increase the workload for existing staff members, compromise the quality of patient care, and place an excessive burden on the healthcare system. Arising from high retirement and turnover rates among experienced registered nurses (RNs) and new R.N.s, the shortage of nurses equates to tremendous pressure on the already stressed nursing profession to train more nurses quickly. Since this problem has implications for the deterioration of the general population’s health, despite the billions of dollars invested in the healthcare industry, it is imperative to investigate ways to prioritize and optimize the retention of newly hired nurses and facilitate their smooth integration into professional practice.
Developing an effective intervention plan should fully consider the on-the-ground realities of the specific care setting and the target population for the proposed intervention. The plan will focus on an urban teaching hospital such as Johns Hopkins Hospital” in Baltimore, Maryland, USA, characterized by a diverse patient population and associated with a high demand for healthcare services. Investigation into the retention of newly hired nurses to ensure their smooth integration into professional practice would be highly suitable because of the acute nature of challenges that could arise from a shortage of nurses in such an environment. Therefore, this paper is aimed at investigating the following PICOT question: For newly graduated nurses with less than two years of professional nursing experience (P), how does participation in an NRP (I) compare to not participating in such a program (C) in influencing job retention rates (O) within a timeframe of six months (T)? Having already evaluated the impact of nurse residency programs on job retention rates for new registered nurses in addition to the development of a nursing protocol, this paper details the implementation of an intervention plan for the stated PICOT question based on factors such as the culture of the care setting, the resources available, and the stakeholders involved in the project.
The intervention group will consist of nurses enrolled in a 6-month nursing residency program (NRP), with a control group not enrolled in such a program. According to An et al. (2022), a significant proportion of newly employed nurses, precisely 33% within the initial year and potentially up to 56% within the subsequent year, choose to discontinue their employment. Therefore, the study will involve a 3-month planning and development period, a 6-month NRP, followed by an evaluation of nurse retention rates for the next two years, equating to 2.75 years.
Management and Leadership
R.N.s, doctors, nurse administrators, pharmacists, physical therapists, and social workers will create formal committees over the 6-month NRP to promote cooperation. Members would debate and identify NRP components that improve retention, including skill development, mentoring, and supportive work cultures. Multidisciplinary team meetings should also address progress, challenges, and opportunities for development.
Committees and teams should evaluate nurse residency programs and processes using evidence-based approaches. Performance-based measures should assess the NRP’s impact on employment retention and care quality. Informal channels may provide crucial information on professional development possibilities, the NRP’s role in integrating newly graduated nurses into professional practice, and effective feedback systems.
All stakeholders will be notified of the intervention plan’s goals and purpose, emphasizing its need to alleviate the nurse shortage and enhance employment retention. A residency program costs $93,100, or $2,023.91 per resident, including program creation, training materials, and NRP organization and facilitation costs. Since replacing one new graduating R.N. costs $45,000, reducing R.N. turnover may boost ROI. Increasing research shows that the NRP’s initial expenditures outweigh the cost savings from decreased new graduate turnover, proving its worth to the organization (Hansen, 2013). Electronic health records (EHR) and automation will reduce healthcare administration costs. The manual burden is reduced by EHR systems’ paperwork reduction, coordination, appointment scheduling and billing automation. Workload evaluations and flexible scheduling optimize staffing for patient volume variations.
Delivery and Technology
Make use of new technologies for continual improvement to offer the NRP. Online learning platforms and interactive simulation technology can accommodate nurses’ schedules and provide continual education (Yadav et al., 2021). This would promote regulated skill development and practical competence. Information Technology Integrated Instruction (ITII) improved OSCE and lab results in nursing education (Kyaw et al., 2019). Zoom and Microsoft Teams would facilitate committee meetings and interdisciplinary team discussions and allow healthcare workers to communicate remotely (Danton & Bushnell, 2023). Blockchain technology allows the NRP to keep records transparent and secure, protecting participant data.
Stakeholders, Policy, and Regulations
An academic medical centre’s nursing expertise project team manages the nurse residency program. New nurses are important stakeholders, while patients demand competent care from them. The Chief Nursing Officer and Department Director of Education and Research provide clinical leadership, strategic planning, and program administration. The operational development manager leads clinical observations and curriculum for freshly graduating nurses and coordinates professional development. The American Academy of Nursing (AAN) 6-point policy (Figure 1) of 2018 will be used to analyze stakeholders, comprehend regulatory consequences, and provide policy considerations for intervention plan execution (Figure 2)
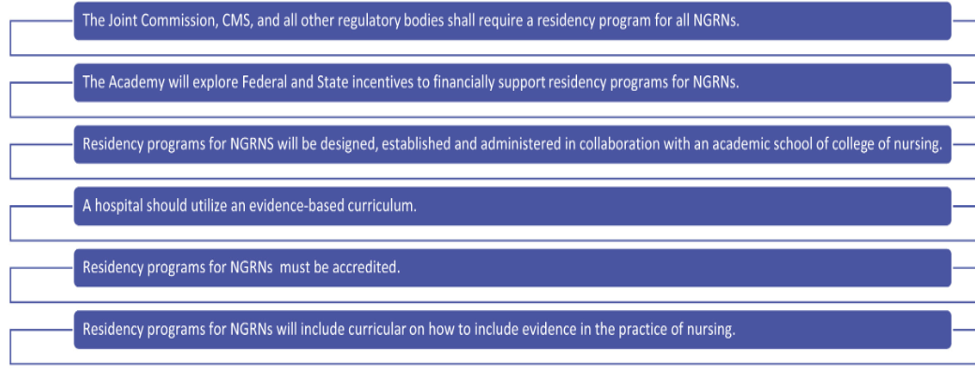
Figure 1. The existing 6-point policy of the American Academy of Nursing (AAN) (Goode et al., 2018)
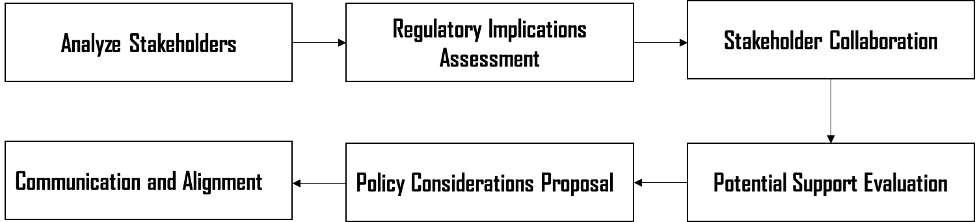
Figure 2. A systematic approach to analyzing stakeholders, understanding regulatory implications, and proposing policy considerations for the implementation of the intervention plan
Timeline
Implementation – Nurse Residency Program (NRP) (6 Months)
To guarantee the program’s efficacy, ongoing assessments and modifications will be made. A watchful eye will be kept on participant engagement, progress, and satisfaction.
Post-Implementation Evaluation (2 Years)
Over the next two years, nurse retention rates will be assessed, with data being collected regularly. The intervention’s results and efficacy will be compared to the control group’s. Responses from participants, interested parties, and pertinent departments will be gathered. Progress and results will be shared frequently to keep all stakeholders involved and supportive (Figure 3).
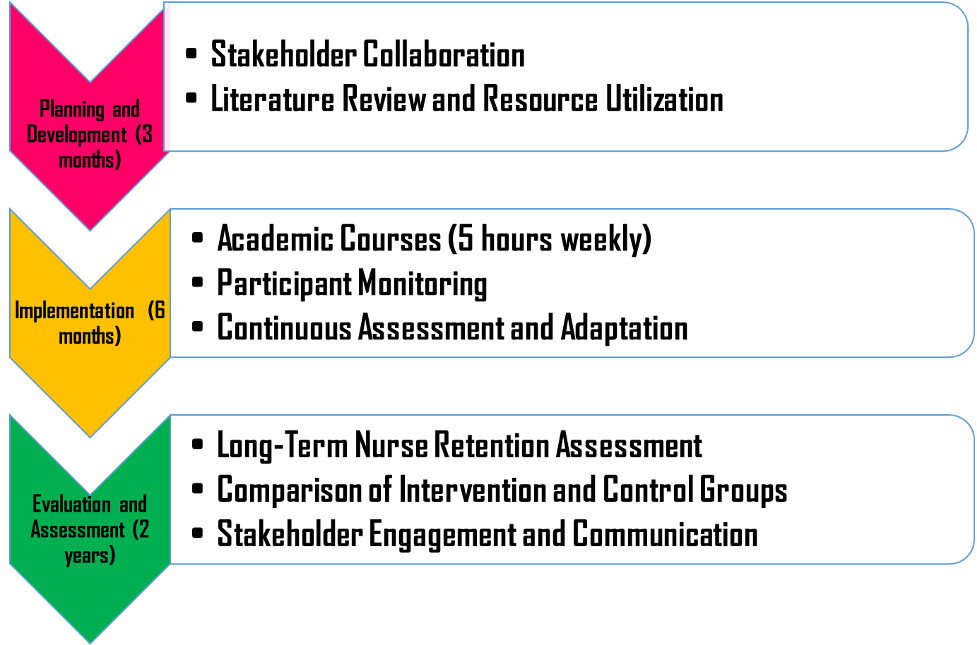
Figure 3. The proposed timeline for the planning and development, implementation of the NRP, and evaluation and assessment of the NRP
Evaluation of the Plan
The plan’s primary objective is to evaluate the effectiveness of NRPs on the retention rate of newly graduated R.N.s. Therefore, the study will deal with three specific and measurable outcomes assessed over the two-year post-intervention period.
- Assessment of the less-than-2-year retention rates in the intervention and treatment groups, followed by an examination of the relationship between turnover for the two groups
- Examination of work engagement levels between the intervention and treatment groups
- Determination of the return on investment (ROI) to compare turnover costs (hiring, vacancy, and training of new R.N.s) against the costs of implementing the NRP
Retention Rate
Following the participation of R.N.s in the NRP, the less-than-2-year retention rates will be determined for both nurses who participated in the program (intervention group) and those who did not (control group). The retention rate will be calculated using the following formula:
A chi-square analysis will be performed in order to evaluate the relationship between retention rates in the intervention and control groups and ascertain the existence of a significant difference between the groups. Analysis will be performed using IBM® SPSS® statistical software, and an alpha level of 0.05 will be used to assess statistical significance.
Advocacy
Nurses can improve quality outcomes while reducing the length of stays, benefiting patients and healthcare institutions. Following Kotter’s 8-step framework, nurses can facilitate communication in change processes and develop a sense of urgency to inform staff and stakeholders of the need for nurse-facilitated patient mobilization (Mount & Anderson, 2015). Nurses are also in a position to affect transformative social change by tackling economic health disparities to promote health equity. For example, RN Lauren Underwood, who also serves as a member of the U.S. House of Representatives, not only addressed the health and economic impacts of the pandemic on African Americans but also sponsored multiple bills, such as H.R. 6142, aimed at improving maternal health outcomes in communities of colour (National Academies of Sciences, Engineering, and Medicine, 2021). The evidence-based curriculum used in the NRP would include thorough training sessions to educate nurses on patient communication, collaboration with other nurses and healthcare professionals, and conducting transparent documentation practices.
Future Steps
The program could also incorporate virtual reality (V.R.) into the training models of the NRP. Compared to traditional teaching instruction, using V.R. could increase theoretical knowledge and provide real-world simulations of problems that nurses could face in the professional work environment. V.R. may provide numerous applications in terms of clinical practice and the application of theoretical knowledge in a risk-free environment. Moreover, using data analytics in the evaluation phase of the plan could aid in monitoring progress, identifying areas for improvement, and improving the program for future participants.
Further improvements involve the implementation of the Continuous Quality Improvement (CQI) framework to allow progressive and gradual improvements in processes, patient outcomes, and safety levels. Implementation of improvements will be followed by measurements of the effects of the improvement, benchmarking, and goal setting (O’Donnell & Gupta, 2023). The project should also promote the adoption of the team nursing care model. Team nursing aims to foster responsibility sharing and teamwork between team members, including an R.N. commonly serving as a supervisor. Cooperative teamwork is the main advantage of providing care because each team member is responsible for the high standard and safety of the treatment delivered (Abusamra et al., 2022).
Reflection on Leading Change and Improvement
The project has provided the researcher with hands-on experience in developing, implementing, and evaluating an intervention plan. The comprehensive development of a compelling PICOT question associated with real-world problems prompted the researcher to support the plan with evidence-based solutions. The project has also taught the researcher how to think critically about aspects that could lead to increased patient safety, more favourable health outcomes, and the promotion of sustainable healthcare. Inspiration by R.N.s such as Lauren Underwood and the acquisition of new knowledge about nursing prospects have resulted in an increased inclination to hone leadership skills and make an effort to become involved in community outreach programs, fostering a healthy excitement for future endeavours in the nursing profession. Furthermore, research as part of the project has increased encouragement and motivation to learn more about technology incorporation and new care models to make a broader societal impact.
The project’s development, implementation, and evaluation have provided strategic planning and management skills. Upon encountering a problem in the real-world nursing profession, the researcher is more informed on how to create a systematic approach to solving workplace problems, such as setting clear objectives with measurable outcomes and using continuous feedback to implement sustainable improvements. Decisions must be based on evidence from the literature or observable workplace practices and interpreted after thorough collaboration with team members and supervisors. Such skills are transferable across different contexts, such as acute care facilities, hospitals, long-term care providers, and academic institutions. Collaboration with fellow students, nurse managers, healthcare groups, and corporate organizations will assist in implementing what has been learned about the importance of maintaining stakeholder support for sustaining projects.
References
Dineen-Griffin, S., Garcia-Cardenas, V., Williams, K., & Benrimoj, S. I. (2019). Helping patients help themselves: a systematic review of primary health care practice self-management support strategies. PloS one, 14(8), e0220116. https://journals.plos.org/plosone/article/file?id=10.1371/journal.pone.0220116&type=printable
Hookmani, A. A., Lalani, N., Sultan, N., Zubairi, A., Hussain, A., Hasan, B. S., & Rasheed, M. A. (2021). Development of an on-job mentorship program to improve the nursing experience for enhanced patient experience of compassionate care. BMC Nursing, 20, 1-18. file:///C:/Users/OG/Downloads/s12912-021-00682-4.pdf
Jangland, E., Gunningberg, L., & Nyholm, L. (2021). A mentoring programme to meet newly graduated nurses’ needs and give senior nurses a new career opportunity: A multiple-case study. Nurse education in practice, 57, 103233.
Kaihlanen, A. M., Hietapakka, L., & Heponiemi, T. (2019). Increasing cultural awareness: qualitative study of nurses’ perceptions about cultural competence training. BMC nursing, 18(1), 1-9. file:///C:/Users/OG/Downloads/s12912-019-0363-x.pdf
Nightingale, J., Fowler-Davis, S., Grafton, K., Kelly, S., Langham, C., Lewis, R., & Harrop, D. (2020). The role of allied health professions and nursing research internships in developing a research culture: a mixed-methods exploration of stakeholder perspectives. Health Research Policy and Systems, 18, 1-17. file:///C:/Users/OG/Downloads/s12961-020-00638-1.pdf
Yip, J. Y. C. (2021). Theory-based advanced nursing practice: A practice update on the application of Orem’s self-care deficit nursing theory. SAGE Open Nursing, 7, 2377960821101199
Ackerson, K., & Stiles, K. A. (2018). Value of nurse residency programs in retaining new graduate nurses and their potential effect on the nursing shortage. The Journal of Continuing Education in Nursing, 49(6), 282-288.
An, M., Heo, S., Hwang, Y. Y., Kim, J., & Lee, Y. (2022). Factors affecting turnover intention among new graduate nurses: Focusing on job stress and sleep disturbance. Healthcare, 10(6), 1122. https://doi.org/10.3390/healthcare10061122
AbuAlRub, R. F., & Abu Alhaija’a, M. G. (2019). Perceived benefits and barriers of implementing nursing residency programs in Jordan. International Nursing Review, 66(1), 43–51. https://doi.org/10.1111/inr.12452
Er, F., & Sökmen, S. (2018). Investigation of the working conditions of nurses in public hospitals on the basis of nurse-friendly hospital criteria. International Journal of Nursing Sciences, 5(2), 206–212. https://doi.org/10.1016/j.ijnss.2018.01.001
Goode, C. J., Lynn, M. R., McElroy, D., Bednash, G. D., & Murray, B. (2013). Lessons learned from 10 years of research on a post-baccalaureate nurse residency program. The Journal of Nursing Administration, 43(2), 73–79. https://doi.org/10.1097/NNA.0b013e31827f205c
Haddad, L., Annamaraju, P., & Toney-Butler, J. (2023). Nursing Shortage. Treasure Island (F.L.): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK493175/
Knighten, M. (2022). New nurse residency programs: Benefits and return on investment. Nursing Administration Quarterly, 46(2), 185-190.
Lowman, G. H., & Harms, P. D. (2022). Addressing the nurse workforce crisis: a call for greater integration of the organizational behavior, human resource management and nursing literatures. Journal of Managerial Psychology, 37(3), 294-303.
Majeed, N., & Jamshed, S. (2021). Nursing turnover intentions: The role of leader emotional intelligence and team culture. Journal of Nursing Management, 29(2), 229-239. https://doi.org/https://doi.org/10.1111/jonm.13144
Silvestre, J. H., Ulrich, B. T., Johnson, T., Spector, N., Blegen. M. A. (2017). A multisite study on a new graduate registered nurse transition to practice program: Return on investment. Nursing Economics, 35(3), 110-118.
Smiley, R. A., Allgeyer, R. L., Shobo, Y., Lyons, K. C., Letourneau, R., Zhong, E., Kaminski-Ozturk, N., & Alexander, M. (2023). The 2022 national nursing workforce survey. Journal of Nursing Regulation, 14(1), S1-S90. https://doi.org/10.1016/S2155-8256(23)00047-9
Van Camp, J., & Chappy, S. (2017). The effectiveness of nurse residency programs on retention: A Systematic review. AORN Journal, 106(2), 128–144. https://doi.org/10.1016/j.aorn.2017.06.003
Adams, J. M., Alexander, G. A., Chisari, R. G., Banister, G., McAuley, M. E., Whitney, K. B., & Erickson, J. I. (2015). Strengthening new graduate nurse residency programs in critical care: recommendations from nurse residents and organizational stakeholders. The Journal of Continuing Education in Nursing, 46(1), 41-48.
An, M., Heo, S., Hwang, Y. Y., Kim, J., & Lee, Y. (2022). Factors affecting turnover intention among new graduate nurses: Focusing on job stress and sleep disturbance. Healthcare, 10(6), 1122. https://doi.org/10.3390/healthcare10061122
Danton, M. H., & Bushnell, I. (2023). Zoom and its discontents: Group decision making in pediatric cardiology in the time of COVID (and beyond). Journal of Medical Systems, 47(1), 1-6.
Cochran, C. (2017). Effectiveness and best practice of nurse residency programs: A literature review. Medsurg Nursing, 26(1), 53.
Hansen, J. (2013). Nurse residency programs: A critical part of the future of nursing. Journal for Nurses in Professional Development, 29(3), 157-158.
Kyaw, B. M., Saxena, N., Posadzki, P., Vseteckova, J., Nikolaou, C. K., George, P. P., Divakar, U., Masiello, I., Kononowicz, A. A., Zary, N., & Tudor Car, L. (2019). Virtual reality for health professions education: Systematic review and meta-analysis by the digital health education collaboration. Journal of Medical Internet Research, 21(1), e12959. doi: 10.2196/12959
Yadav, S., Sharma, N., Mangla, M., & Mahajan, A. (2021). Blockchain and IPFS-based framework for secure student document record keeping. Journal of Educational Multimedia and Hypermedia, 30(2), 165-181.
 write
write